Abstract
Aims: Significant functional mitral regurgitation (FMR) in elderly heart failure patients is increasingly being treated by MitraClip implantation. We sought to assess the prognostic implications of the intraprocedural assessment of vena contracta area (VCA) after MitraClip therapy in such patients.
Methods and results: MitraClip therapy with intraprocedural assessment of VCA was performed in 97 heart failure patients (74±10 years; 66 men; left ventricular ejection fraction [LVEF] 31±12%; 93 patients in New York Heart Association [NYHA] functional Class III [n=59] or IV [n=34]; 86 patients with FMR severity 3+ [n=65] or 4+ [n=21]). Ninety-one patients (94%) were discharged with FMR severity ≤2+. During a median follow-up of 13.4 (interquartile range 4.6-21.1) months, 32 patients died. Multivariable Cox regression identified increasing age (HR [95% confidence interval]=1.05 [1.00-1.09], p=0.0395), a glomerular filtration rate <50 ml/min/1.73 m² (HR=2.7 [1.3-5.7], p=0.0115), and post-MitraClip VCA >25 mm² (HR=4.5 [2.1-9.5], p=0.0001) as independent predictors of mortality.
Conclusions: In heart failure patients with FMR undergoing MitraClip therapy, increasing age, impaired baseline renal function and post-MitraClip VCA >25 mm² are strongly associated with mortality. Post-MitraClip VCA may be used as intraprocedural guidance with respect to patients’ long-term outcome.
Abbreviations
FMR: functional mitral regurgitation
LVEF: left ventricular ejection fraction
MR: mitral regurgitation
TOE: transoesophageal echocardiography
VCA: vena contracta area
Introduction
Functional mitral regurgitation (FMR) due to ischaemic heart disease or dilated cardiomyopathy is common in patients with chronic congestive heart failure1. In heart failure patients with a reduced ejection fraction, the presence and severity of FMR is adversely associated with survival2-5. Implantation of the MitraClip® (Abbott Vascular, Santa Clara, CA, USA) has become the most frequently used percutaneous modality to treat significant mitral regurgitation in patients not amenable to surgery. According to the 2012 European Society of Cardiology guidelines for valvular heart disease, “... the percutaneous MitraClip procedure may be considered in patients with symptomatic severe FMR despite optimal medical therapy (including cardiac resynchronisation therapy if indicated), who fulfil the echocardiographic criteria of eligibility, are judged inoperable or at high surgical risk by a team of cardiologists and cardiac surgeons, and who have a life expectancy greater than 1 year...”6. Vena contracta area (VCA), measured intraprocedurally by three-dimensional transoesophageal echocardiography (TOE), is a novel variable reflecting the severity of MR: it is directly affected by the intervention and can be determined by the addition of planimetered areas in the presence of multiple regurgitant jets7-10. Since about two in three patients undergoing MitraClip therapy in Europe present with FMR and impaired left ventricular function11, i.e., constitute essentially a heart failure population, we sought to assess the association of post-MitraClip VCA with mortality in this challenging cohort.
Methods
PATIENTS
Of the 192 patients with FMR who underwent MitraClip therapy at our institution between December 2010 and February 2014, only those 97 patients not lost to follow-up in whom VCA was determined before and after the intervention were retrospectively chosen as the study cohort. The mean age of the study patients was 74 years, 68% were men, and all had been adjudicated by Heart Team consensus as inoperable or at high surgical risk (Table 1). Of note, 51% of the patients presented with impaired renal function, as reflected by a glomerular filtration rate <50 ml/min/1.73 m² (estimated via the Chronic Kidney Disease Epidemiology Collaboration [CKD-EPI] formula), and 84 patients (87%) had impaired left ventricular function with an ejection fraction ≤45%. The vast majority (96%) of the patients were in New York Heart Association (NYHA) functional Class III or IV (Figure 1).
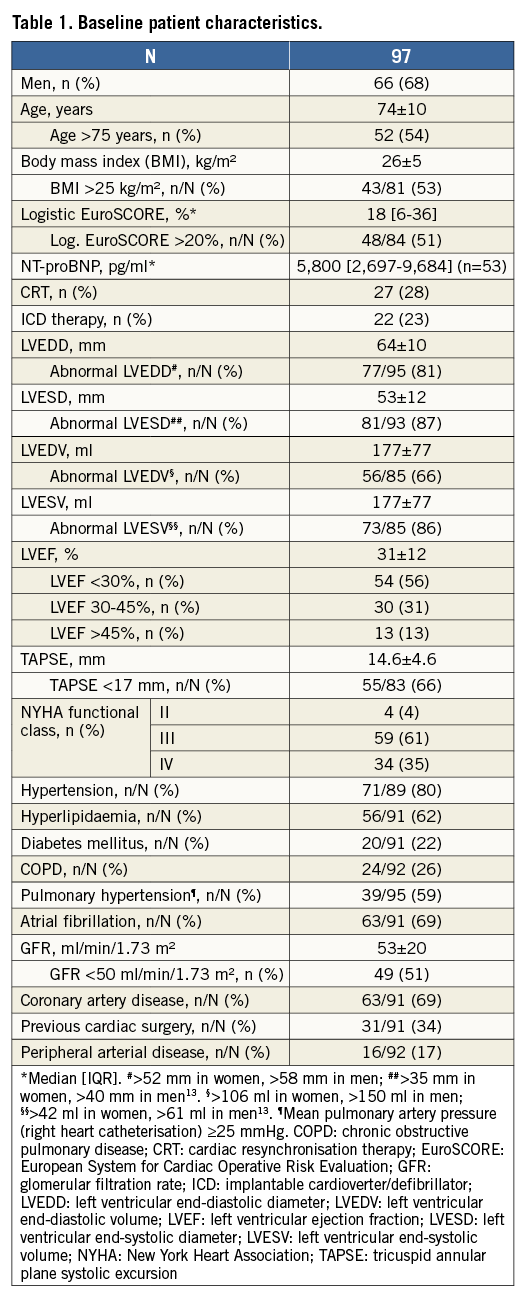
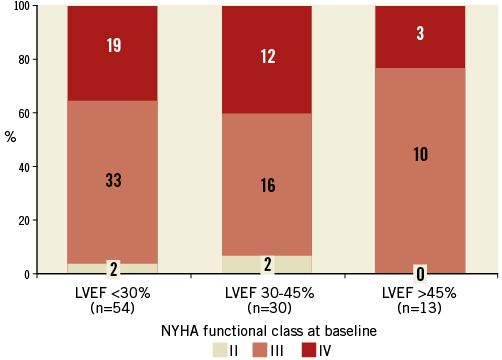
Figure 1. Distribution of baseline New York Heart Association (NYHA) functional class according to left ventricular ejection fraction (LVEF) category.
MITRACLIP IMPLANTATION
MitraClip implantations were performed in accordance with a previously described protocol12. Procedural success was defined as MR severity ≤2+ at discharge.
ECHOCARDIOGRAPHY
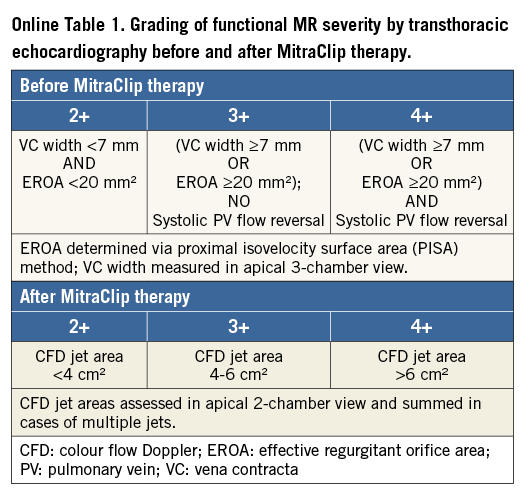
All patients underwent two-dimensional transthoracic echocardiography (Vivid™ E9; GE Vingmed Ultrasound AS, Horten, Norway, or iE33; Philips Medical Systems, Andover, MA, USA) before and after the intervention. Standard parameters of left ventricular dimension were assessed according to recent guidelines. LVEF was calculated from left ventricular volumes via Simpson’s rule, and tricuspid annular plane systolic excursion (TAPSE) served as an assessment of right ventricular function13,14. MR severity was graded by way of vena contracta width, effective regurgitant orifice area, and the presence or absence of pulmonary venous flow reversal before MitraClip therapy15, and via colour flow Doppler jet area after MitraClip therapy16 (Online Table 1).
Intraprocedural TOE was performed with the iE33 echocardiography system and a corresponding probe (X7-2t). Colour Doppler full volumes of the regurgitant jet were acquired over seven to 10 consecutive cardiac cycles. Nyquist limits were set between 40 and 68 cm/sec; colour gain setting was kept at 50% in all patients. Tissue priority was kept at factory settings. To reduce “stitching” artefacts, patients were put on anaesthesia-controlled breath-hold. In patients with atrial fibrillation, Doppler volumes were acquired during episodes with as little cycle length variation as possible. Care was taken to assess pre- and post-MitraClip MR under similar haemodynamic conditions; when needed, fluid challenges and vasodilators were administered to achieve similar blood pressures.
VCA was assessed as previously described7-10 using dedicated software (QLAB 8.0; Philips Medical). Before MitraClip therapy, the frame with the largest VCA in early to mid systole (excluding the very first frame) was identified for plane-corrected planimetry17,18. In order to assess the cross-sectional area at the neck of the vena contracta precisely, the two orthogonal image planes parallel to the jet direction were manually cropped exactly across the regurgitant jet. The plane perpendicular to the jet direction was then moved along the jet to find the minimum cross-sectional area distal to the regurgitant orifice (Figure 2). After MitraClip implantation, the same approach (i.e., alignment of two orthogonal planes with the regurgitant jet, then finding the smallest cross-sectional area in the third orthogonal plane) was used to measure VCAs for each regurgitant jet; single-jet VCAs were added up to arrive at a final post-MitraClip VCA10,17. Very small regurgitant jets with no traceable colour Doppler information at the level of the regurgitant orifice/leaflet tips were not taken into account.
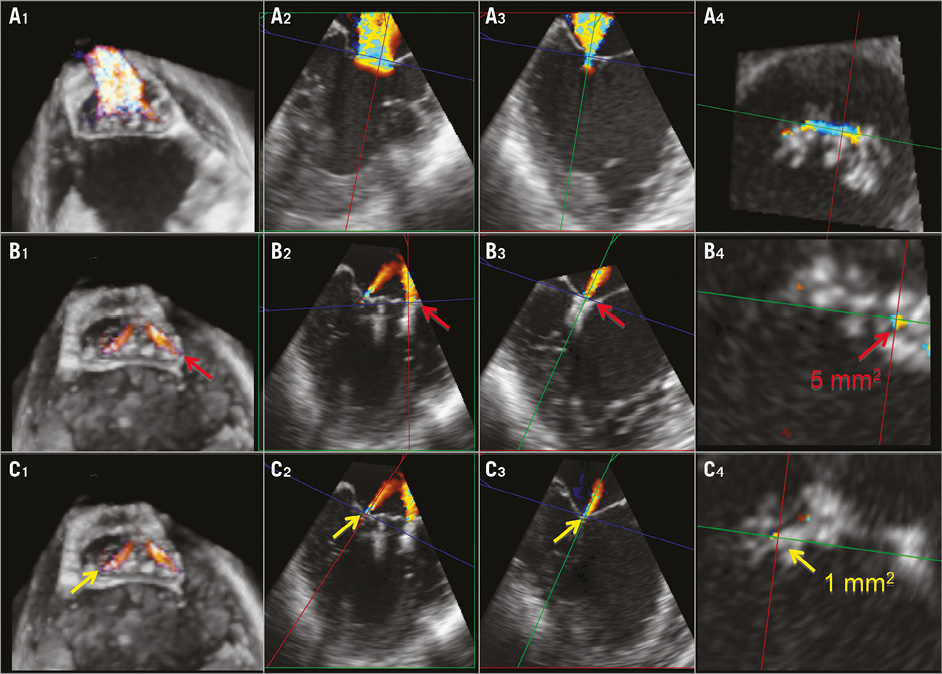
Figure 2. Measurement of VCA by 3D TOE before and after MitraClip implantation. A1-A4 illustrate findings before MitraClip implantation. A1: full-volume colour Doppler view of grade 3+ MR. A2: view of regurgitant jet in cut plane aligned with the jet; red and blue lines denote cut planes orthogonal to the one shown. A3: view of regurgitant jet in cut plane denoted by red line in panel A2; green line denotes cut plane shown in panel A2. A4: view of VCA in cut plane shown in panels A2 and A3 as blue line; VCA was 45 mm². B1-B4 and C1-C4 illustrate corresponding findings for lateral (red arrows) and medial regurgitant jet (yellow arrows), respectively, persisting after MitraClip implantation. With lateral jet VCA 5 mm² and medial jet VCA 1 mm², total post-MitraClip VCA was 6 mm².
All VCA measurements were performed by two experienced investigators (H. Alessandrini, F. Kreidel). To assess intra-observer variability, both investigators measured post-MitraClip VCAs twice at a three-week interval in 25 randomly selected patients.
FOLLOW-UP
After hospital discharge, follow-up visits were scheduled at six weeks and 12 months, with annual telephone follow-up conducted thereafter.
ETHICS
Written informed consent was obtained from all patients.
STATISTICS
Continuous variables are described as means and standard deviations or as medians plus interquartile range (IQR). Differences between continuous variables were analysed with t-tests (normally distributed data) and the Mann-Whitney U test or Wilcoxon’s signed-rank test (non-normally distributed data or markedly unequal group sizes). Three-group comparisons of continuous variables were assessed using one-way analysis of variance. Categorical variables are described with absolute and relative frequencies. Differences between categorical variables were evaluated with the chi-square or Fisher’s exact test. Linear regression (Pearson correlation) and Bland-Altman analysis were used to evaluate the relationship and agreement, respectively, between VCA measurements by the two investigators. Intraclass correlation coefficients (ICCs) were calculated to assess the reliability of VCA measurement by the two investigators (two-way mixed model) as well as the reliability of repeated VCA measurement by the same investigator (one-way random model). Patient survival was assessed using the Kaplan-Meier method, log-rank test, and Cox proportional hazards regression analysis. All covariates which were statistically significant (p<0.05) on univariate analysis were entered into a “full” multivariable proportional hazards model that adhered to the “10 events per independent variable” recommendation19.
A two-tailed p-value <0.05 was considered statistically significant, except for multiple (n=3) two-group comparisons, for which p<0.0167 was considered statistically significant. Statistical analyses utilised the StatView 4.5 (Abacus Concepts, Inc., Berkeley, CA, USA) and SPSS, Version 22 (IBM Corp., Armonk, NY, USA) software packages.
Results
PROCEDURAL OUTCOMES
In the course of the 97 interventions, a total of 149 clips were implanted, with 51 patients receiving a single clip, 41 patients receiving two clips, and five patients receiving three (n=4) or four (n=1) clips. The mean number of regurgitant jets visualised on transthoracic echocardiography in the apical two-chamber view was 1.2±0.6 (range 0-3). Median total device time, i.e., the time from transseptal puncture to withdrawal of the clip delivery system from the left atrium, was 53 (IQR 36-88) minutes. With baseline MR severity predominantly 3+ (n=42) or 4+ (n=41), the interventions resulted in patients being discharged mostly with MR 1+ (n=52) or 2+ (n=39) (Figure 3). Procedural failures were encountered in six patients (6.2%).
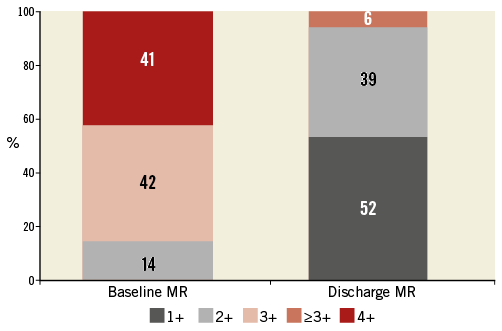
Figure 3. Distribution of mitral regurgitation (MR) severity at baseline and discharge in the 97 study patients.
VCA MEASUREMENT
With VCA values ranging between 0 and 70 mm², the mean difference between two measurements was 0.6±2.8 mm² (ICC=0.986; 95% confidence interval [CI]: 0.969 to 0.994, p<0.0001) for one investigator and 3.2±4.5 mm² (ICC=0.817; 95% CI: 0.631 to 0.915, p<0.0001) for the other. Inter-observer variability for all 194 (97 pre- and 97 post-MitraClip) VCA measurements is illustrated in Figure 4. Overall correlation between investigators was good (Pearson’s r=0.95, p<0.001; ICC=0.949; 95% CI: 0.933 to 0.961, p<0.0001). The Bland-Altman plot revealed a mean bias close to 0 mm² (+1 mm² for pre-, –1 mm² for post-MitraClip VCA measurements), with markedly lower 95% limits of agreement (–23.5 mm² to 21.5 mm²) for post-MitraClip measurements.
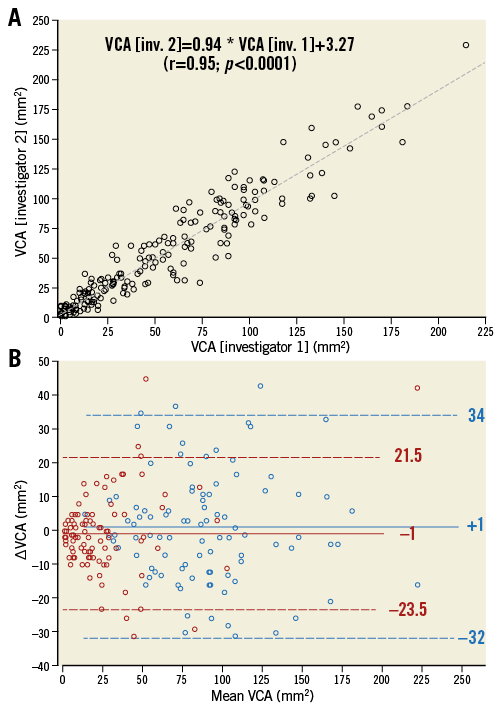
Figure 4. Statistical evaluation of VCA measurements. A) Correlation of VCA measurements by two investigators. Pearson’s correlation coefficient is 0.95. B) Bland-Altman plot of pre- (blue circles) and post-MitraClip (red circles) VCA measurements in 97 patients. Solid horizontal lines denote the mean difference in VCA measurements between the two investigators: +1 mm² for pre-MC, –1 mm² for post-MC measurements. Broken horizontal lines mark the upper and lower 95% limits of agreement (±1.96 standard deviations). MC: MitraClip
The mean VCA between the two investigators was used for all subsequent analyses.
MitraClip implantation resulted in a significant decrease in VCA from 86 (median; IQR 60-108) mm² pre-MitraClip to 17 (7-29) mm² at the end of the procedure (post-MitraClip; p<0.0001). Post-MitraClip VCA increased with increasing discharge MR grade; however, there was pronounced overlap of VCA values between MR grades (Figure 5).
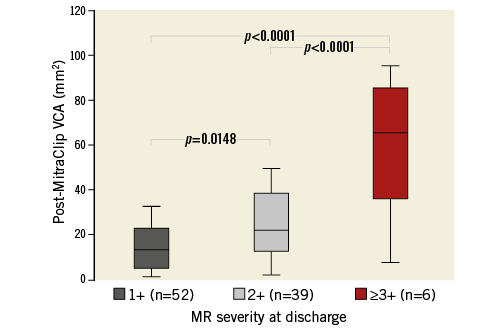
Figure 5. Box plots of post-MitraClip VCA according to MR severity at discharge.
FOLLOW-UP
With two patients lost to follow-up, 95 patients were followed for a median of 13.4 (IQR 4.6-21.1) months. During follow-up, a total of 32 patients died at a median of 408 (IQR 141-642) days post-MitraClip (29 [33%] of 89 successfully, three of six unsuccessfully treated patients). The cause of death could not be determined in four patients; 24 patients died of cardiac reasons at a median of 130 (50-360) days, and the other four patients died of non-cardiac reasons at a median of 57 (26-292) days (p=0.32). Latest post-MitraClip functional status was assessed in 43 of the 63 surviving, successfully treated patients at a median of 18 (14-27) months. At that time, 28 patients (65%) were in NYHA functional Class I or II, with improvement in NYHA class noted in 31 patients (72%), no change in 10 patients (23%), and worsening in two (5%).
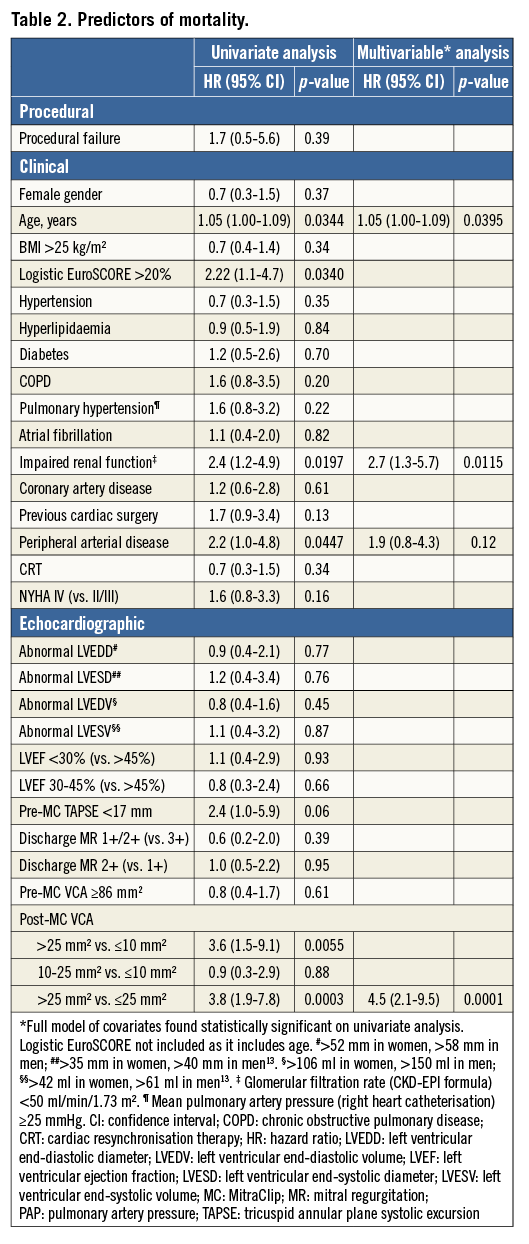
To assess predictors of mortality, pertinent procedural, clinical and echocardiographic variables were tested in univariate Cox proportional hazards models. Increasing age, a logistic EuroSCORE >20%, impaired renal function at baseline, the presence of peripheral arterial disease, and a post-MitraClip VCA >25 mm² turned out to be predictive of mortality. Notably, impaired LVEF (≤45%), NYHA functional Class IV and discharge MR severity did not impact on mortality (Table 2). With no apparent differential impact of the lower two post-MitraClip VCA terciles on mortality (hazard ratio [HR] 0.9, p=0.88), and since the logistic EuroSCORE incorporates age, post-MitraClip VCA dichotomised at 25 mm², age, impaired baseline renal function and peripheral arterial disease were tested in a multivariable proportional hazards model. Increasing age, post-MitraClip VCA >25 mm² and impaired renal function prevailed as statistically significant, independent predictors of mortality, with HRs of 1.05 (p=0.0395), 4.5 (p=0.0001) and 2.7 (p=0.0115), respectively (Table 2).
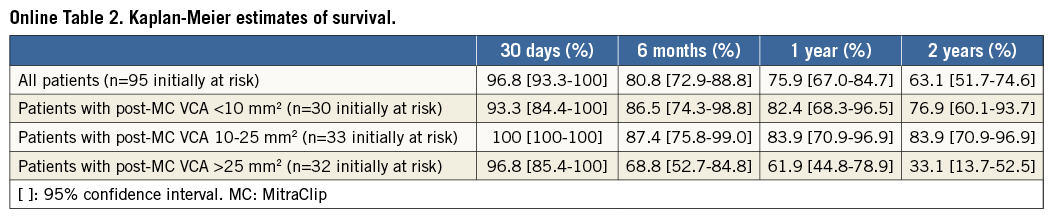
To illustrate the association of post-MitraClip VCA with survival, Figure 6 shows a statistically significant difference (p=0.0005) between survival curves according to terciles of post-MitraClip VCA. Post hoc two-group comparisons revealed no difference in survival between patients in the lower vs. the middle post-MitraClip VCA tercile (<10 mm² vs. 10-25 mm², p=0.83), but statistically significant differences in survival between patients in the middle vs. the upper tercile (10-25 mm² vs. >25 mm², p=0.0015), and between patients in the lower vs. the upper tercile (<10 mm² vs. >25 mm², p=0.0028). Survival estimates are given in Online Table 2.
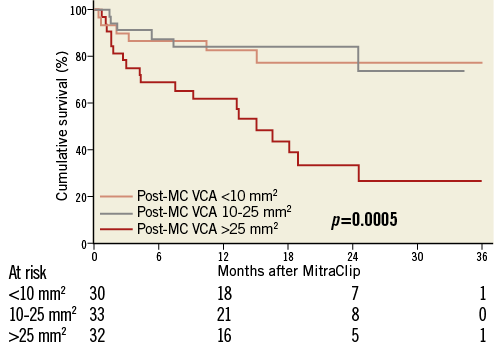
Figure 6. Cumulative survival curves in 95 patients according to terciles of post-MitraClip VCA. Log-rank p=0.0005 indicates overall difference between survival curves. MC: MitraClip
Discussion
MAJOR FINDINGS
Unique to this single-centre study of 97 heart failure patients with predominantly moderate-to-severe (3+) or severe (4+) FMR is the finding of a strong association of mortality with post-MitraClip VCA. Compared with patients in whom VCA was ≤25 mm² after MitraClip implantation, the likelihood of death during follow-up was increased by a factor of 4.5 in patients with a post-MitraClip VCA >25 mm². The only other covariates independently and strongly predictive of mortality were increasing age and impaired baseline renal function, defined as a glomerular filtration rate <50 ml/min/1.73 m².
Functional assessment in 43 of our patients at a median of 18 months after successful MitraClip implantation revealed that 72% had improved from baseline, such that roughly two thirds were in NYHA functional Class I or II at that time point.
The primary intention of our study was to assess whether three-dimensional VCA as a fairly easily acquired parameter is of prognostic value. A previous study found that a reduction in VCA by >50% was associated with a smaller annulus area pre-MitraClip and a greater reduction in atrial and ventricular volumes six months post-MitraClip17, but, to the best of our knowledge, a VCA of 25 mm² has never been discussed as a marker of procedural success.
PREDICTORS OF MORTALITY AFTER MITRACLIP THERAPY
Of note, in our study, baseline LVEF and baseline NYHA functional class were not associated with mortality after MitraClip therapy. These covariates were found to predict mortality in the German TRAMI (n=749) and the Italian GRASP-IT (n=304) registries20,21. However, it must be realised that almost all of our patients had impaired left ventricular function (mean LVEF 31%, n=84 with LVEF ≤45%) and that almost all presented with heart failure symptoms of NYHA functional Class III or IV. Apparently, in this patient cohort, minor variations in LVEF towards the better or the worse did not affect mortality. NYHA functional Class III at the time of the intervention, as opposed to NYHA Class IV, appeared to be beneficial in terms of survival only for the first year after treatment and thus corresponds to the finding of Franzen and co-workers22. By two years, however, that benefit was lost in our patients.
Both the TRAMI and GRASP-IT registries identified procedural failure as predictive of mortality20,21. With a procedural failure rate of only 6.2% in the 97 patients of our study, an association between procedural outcome and mortality was not apparent.
CLINICAL RELEVANCE
The presence of MR in heart failure patients has been shown to impact adversely on the patients’ prognosis: in particular, mortality was directly associated with the severity of MR2-5. In our study, however, we did not observe an association with mortality of discharge MR severity assessed by regurgitant colour flow jet area. Apparently, post-MitraClip MR grade as determined via that variable is not a reliable representation of the true severity of residual MR.
Since VCA can be measured during the procedure, post-MitraClip VCA assessment may become a means to indicate whether the number of clips implanted is sufficient in terms of prognosis or not. In our patients, a post-MitraClip VCA >25 mm² was associated with a poor prognosis. Although it is tempting to consider a post-MitraClip VCA of 25 mm² as a cut-off that discriminates patients with a favourable prognosis from those with a poor prognosis, it must be realised that grouping of patients by terciles is arbitrary. The 25 mm² value represents the upper limit of the middle tercile (i.e., the 67th percentile of the total post-MitraClip VCA distribution) in our cohort of 97 patients; the uncertainty when considering 25 mm² as a generally valid cut-off is reflected by a 95% confidence interval ranging from 21 to 30 mm². Therefore, greater numbers of patients are needed to confirm the clinical validity of the 25 mm² post-MitraClip VCA cut-off.
Limitations
Patients in this retrospective single-centre study were not enrolled consecutively but rather based on the availability of i) VCA measurements pre and post MitraClip therapy, and ii) follow-up information. The study did not involve an independent echocardiographic core laboratory. The presence or absence of reverse remodelling and its prognostic impact were not assessed, and the velocity time integral across the mitral valve was not measured; therefore, regurgitant volumes could not be calculated retrospectively. The number of patients studied was not high enough for a narrow 95% confidence interval associated with the 25 mm² post-MitraClip VCA cut-off. Validation of a prognostically relevant cut-off would require a separate patient population.
Conclusions
In heart failure patients undergoing MitraClip therapy for significant functional MR, we have introduced the “new” quantitative echocardiographic variable of post-MitraClip VCA to assess prognosis. Post-MitraClip VCA may lend itself as a tool to guide interventional decision making with respect to the patient’s long-term outcome. Our findings require prospective validation in larger patient cohorts.
| Impact on daily practice Intraprocedural measurement of VCA by 3D TOE may be helpful to assess the acute outcome of MitraClip implantation. |
Conflict of interest statement
U. Schäfer and K-H. Kuck have received research grants from Abbott Vascular. The other authors have no conflicts of interest to declare.
Supplementary data