Abstract
Aims: The aim of this study was to report medium-term outcomes of MitraClip implantation in inoperable or high-risk surgical candidates with functional mitral regurgitation (FMR) in our single-centre experience.
Methods and results: From October 2008, 109 consecutive patients with FMR underwent MitraClip implantation (mean age 69±9 years; 82% NYHA Class III-IV). Logistic EuroSCORE was 22±16%. Comorbidities included: chronic renal failure (47%), diabetes (22%), COPD (28%). Mean EF was 28±11%; LVEDD was 68±8 mm. Procedural success was 99% and 30-day mortality was 1.8%. At discharge, 87% patients had MR ≤2+. At 12 months, EF was 34.7±10.4% (p=0.002 compared to preoperative value). Actuarial survival at three years was 74.5±7%. Actuarial freedom from MR ≥3+ at 2.5 years was 70±6%. At one-year follow-up, 86% of patients were in NYHA Class I-II. Preoperative pro-BNP level ≥1,600 pg/ml was identified as an independent risk factor of mortality at follow-up.
Conclusions: MitraClip therapy for FMR is a valuable alternative to surgery in high-risk patients. Higher preoperative pro-BNP level is a risk factor for mortality at follow-up. Although patients treated in current practice are high-risk, the procedure remains safe and effective in selected patients.
Introduction
Surgical repair of severe functional mitral regurgitation (FMR) in patients with post-ischaemic or idiopathic dilated cardiomyopathy and left ventricle (LV) systolic dysfunction has been demonstrated to improve symptoms and quality of life1-4. However, perioperative mortality after surgery for FMR is not negligible, and a large number of patients with FMR are not referred for open heart surgery because of high surgical risk or comorbidities5,6. New percutaneous techniques have recently been developed to treat MR with less invasive approaches. The MitraClip™ (Abbott Vascular Inc., Santa Clara, CA, USA) is a device reproducing the Alfieri surgical technique7 with a percutaneous approach, which has been used to decrease the invasiveness of treating both degenerative and functional MR in high-risk patients8-14. The aim of this study was to report the clinical outcomes of MitraClip therapy to treat symptomatic high-risk patients with severe FMR and severe LV dysfunction in our single-centre experience.
Methods
We retrospectively analysed the clinical and echocardiographic data of a cohort of consecutive patients who underwent MitraClip therapy for severe or moderately severe symptomatic FMR refractory to medical therapy. All the patients underwent preoperative coronary angiography and transoesophageal Doppler echocardiography (TEE). The study protocol was performed in accordance with the protocol of the institutional ethics committee, and all patients gave written informed consent for the procedures and data collection.
DESCRIPTION OF THE PROCEDURE
The procedure was performed under general anaesthesia in a hybrid operating room, under TEE and fluoroscopic guidance. Transseptal puncture was performed using a Brockenbrough needle through peripheral venous access at the right groin. Live real-time 3D echocardiography was used to improve the conduct of the implantation. A steerable guide catheter was advanced in the left atrium through the transseptal puncture. The delivery system was inserted and the MitraClip device was implanted corresponding to the origin of the regurgitation jet, perpendicularly to the coaptation line. If the effect of the implant was satisfactory, the clip was deployed. When necessary, more than one clip was implanted. A comprehensive description of the procedure is reported elsewhere15.
PATIENT SELECTION
Patients were selected if they met the basic criteria for intervention of the European Society of Cardiology Task Force recommendations on the management of valvular heart disease16. All the patients underwent transthoracic echocardiography followed by transoesophageal (TEE) examination at baseline. The severity of FMR was graded as: mild, 1+ (jet area/left atrial area <10%); moderate, 2+ (jet area/left atrial area 10-20%); moderately severe, 3+ (jet area/left atrial area 20-45%); and severe, 4+ (jet area/left atrial area >45%). In addition, the vena contracta width at the narrowest portion of the regurgitant jet was measured as follows: ≤0.3 cm, 1-2+; between 0.3 cm and 0.5 cm, 3+; and ≥0.5 cm, 4+. All the patients underwent a multimodality decision-making process including evaluation of surgical risk by logistic EuroSCORE (http://www.euroscore.org/) as well as adjunctive risk evaluation, such as the presence of advanced liver cirrhosis, severe neurological impairment and frailty. Frailty was defined by the Heart Team after collegial discussion, according to the so-called “eyeball test”. Quality of life (QoL) was evaluated using the Minnesota Living with Heart Failure Questionnaire (MLHFQ) and 36-item short-form health survey (SF-36); the six-minute walking test (6MWT) was used to evaluate functional capacity.
Patient selection was partially based on the EVEREST criteria for FMR (central MR with a basal area >4 cm2, coaptation length of at least 2 mm, and coaptation depth <11 mm)8. However, several patients with criteria beyond EVEREST recommendations were treated. The absolute exclusion criteria that we used to determine ineligibility from the procedure were leaflet calcification in the target zone, excessive leaflet retraction, total and irreversible lack of leaflet coaptation, and small valve area with risk of mitral stenosis after clip implantation.
FOLLOW-UP
All the patients were followed up after discharge in a dedicated outpatient clinic with physical examination, ECG, TTE and arrhythmology consultation whenever indicated. Follow-up visits were performed at one month, six months and then yearly.
Statistical analysis
Statistical analysis was conducted using JMP 8.0 software (SAS Institute Inc., Cary, NC, USA). Continuous variables are presented as mean±SD or as median (IQR, Q1-Q3) and categorical variables are expressed as percentages. Univariable comparisons were performed with the Student’s unpaired or paired t-test for continuous normally distributed data, which was tested by the Shapiro-Wilk normality test. The Mann-Whitney rank sum test was used for comparisons of non-parametric continuous data and the chi-square test for categorical data. The threshold of 1,600 pg/ml for preoperative pro-BNP levels was set according to the inclusion criteria of the ongoing COAPT trial17. Survival and freedom from ≥3+ MR were reported using the Kaplan-Meier method; comparisons were performed using the log-rank test. A p-value <0.05 was considered statistically significant, and all reported p-values are two-sided. Univariate analysis of predictors of death at follow-up was performed with Cox proportional hazard regression. Variables with a p-value <0.2 were then inserted in a multivariable model.
Results
PATIENT CHARACTERISTICS
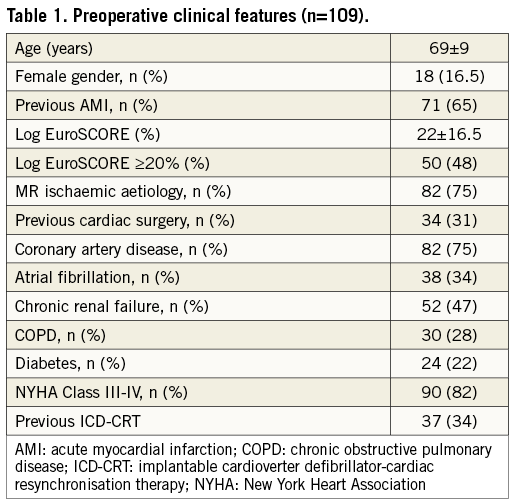
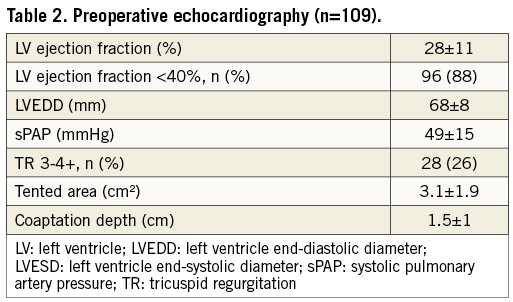
A total of 109 high-risk consecutive patients with severe FMR underwent MitraClip implantation between October 2008 and April 2013 at our institution (75% ischaemic aetiology; 25% idiopathic dilated cardiomyopathy). Demographic and clinical features of the patients are shown in Table 1. A logistic EuroSCORE ≥20% was documented in 48% of the patients. The quality of life questionnaire revealed an important impairment in perceived quality of life in all the patients (MLHFQ was 40±15; SF-36 physical domain was 33±8.7; SF-36 mental domain was 38±9). Median performance of the patients at 6MWT was 190 m (IQR 120-252 m). The preoperative median pro-BNP value was 3,238 pg/ml (IQR 1,452-5,500 pg/ml); 72.3% of the patients had a preoperative pro-BNP value ≥1,600 pg/ml. Table 2 shows the preoperative echocardiography of the study population in detail; 88% of the patients had severe or moderate to severe LV systolic dysfunction (EF <40%). EVEREST criteria were totally fulfilled in only 37% of the patients.
PROCEDURAL AND IN-HOSPITAL OUTCOMES
The procedural success rate was 99%: one patient was converted to conventional surgical mitral valve replacement because of posterior leaflet laceration after clip implantation. One clip was implanted in 33 patients (30.2%), two clips were implanted in 71 patients (65.1%), and three clips were implanted in five patients (4.7%). Procedural time was 95.5±41 min.
Thirty-day mortality was 1.8% (2/109 patients: one from acute cardiogenic shock and multiorgan failure seven days after the procedure; one from haemothorax due to emphysematous bulla rupture 10 days after the procedure). Perioperative results are summarised in Table 3.
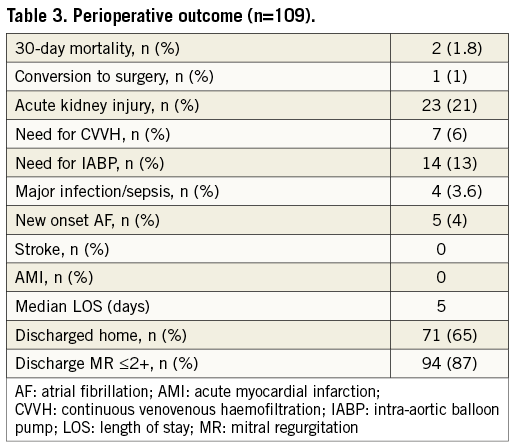
In 57.7% of the patients (63/109), high inotropic support was required in the intensive care unit (defined as adrenaline dosage >0.5 γ/kg/min or association of two or more i.v. inotropic drugs); in 13% of the patients (14/109), an intra-aortic balloon pump (IABP) was required. One patient who underwent conversion to open heart surgery due to structural damage of the mitral valve required transient circulatory support with ECMO because of particularly severe preoperative LV dysfunction; incidence of postoperative new onset acute renal failure (defined as stage 2 or 3 of the modified RIFLE criteria)18 was 21% (23/109 patients) and renal replacement therapy was required in 6% (7/109).
Globally, 63% of the patients had an intensive care unit stay of less than 24 hours. Median postoperative length of stay (LOS) was five days (IQR 3.8-7.6 days). The majority of the in-hospital survivors were discharged directly home (71/107 patients, 66.3% of the total); the rest of the patients were transferred to a cardiopulmonary rehabilitation facility. Pre-discharge echocardiography showed residual MR ≤2+ in 87% of the patients.
FOLLOW-UP
Median follow-up was 13 months (IQR 7-25 months). Overall actuarial survival was 74.5±7% at three years (Figure 1). Patients with a preoperative logistic EuroSCORE ≥20% (71.9±8% vs. 89.8±5.7% at two years; p=0.01), patients with new onset postoperative acute renal failure (67.1±11% vs. 95.7±2% at one year; p=0.003), and patients who required post-procedural IABP (70.1±12% vs. 96.1±2.2% at six months; p=0.009) had a significantly reduced actuarial survival at follow-up.
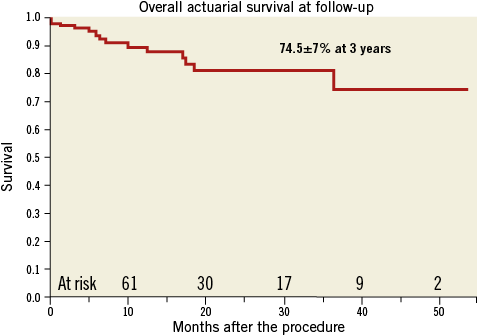
Figure 1. Overall actuarial survival at follow-up.
Cumulative cardiovascular death was 9.1% (10/109 patients: five patients with residual moderate to severe MR died from refractory heart failure, and the causes of death in the other five patients were haemorrhagic stroke, acute myocardial infarction, acute pulmonary oedema with superimposed pulmonary infection, ventricular arrhythmia, and sudden death). One patient underwent heart transplantation because of refractory heart failure 12 months after the procedure; two patients with residual severe MR underwent successful repeat MitraClip implantation 12 and 18 months after the initial procedure, respectively, and two patients ineligible for repeat MitraClip underwent uneventful surgical mitral valve replacement nine and 15 months after the procedure, respectively (logistic EuroSCORE 11.1% and 21.8%, respectively).
Overall actuarial freedom from MR ≥3+ at follow-up was 70±6% at 2.5 years (Figure 2). Freedom from MR ≥3+ at one year was significantly reduced in patients with preoperative TR ≥3+ (65.5±10% vs. 81.7±5%; p=0.01) while no differences were observed according to the adherence to EVEREST criteria (72±6% vs. 87.7±5.8%; p=0.09).
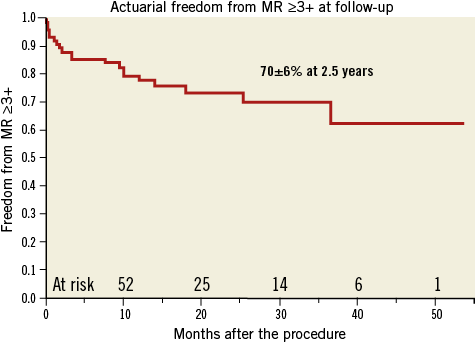
Figure 2. Actuarial freedom from MR ≥3+ at follow-up.
At univariate analysis (Table 4), preoperative logistic EuroSCORE ≥20% (HR 4.4; p=0.01), preoperative level of pro-BNP >1,600 pg/ml (HR 21.2; p=0.01), need for postoperative support with IABP (HR 3.8; p=0.02) and occurrence of postoperative AKI (HR 4.1; p=0.01) were significant risk factors for mortality at follow-up. The multivariate analysis identified a preoperative level of pro-BNP ≥1,600 pg/ml as an independent predictor of mortality at follow-up (HR=4.5; p=0.03). Actuarial survival at one year was 100% for patients with a preoperative level of pro-BNP <1,600 pg/ml and 83.9±5.7% for patients who did not (p=0.05) (Figure 3).
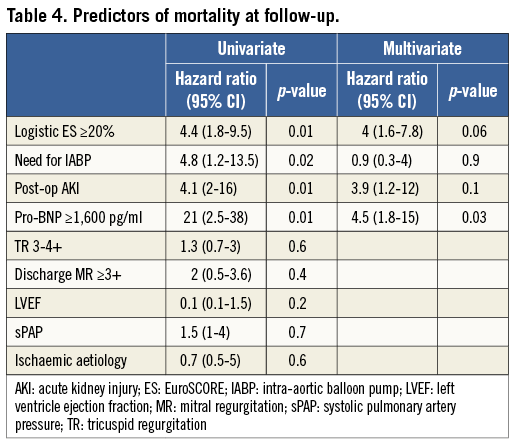
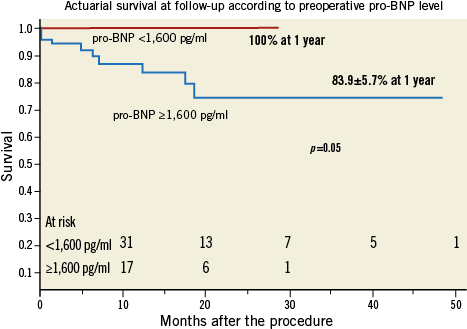
Figure 3. Actuarial survival at follow-up according to preoperative pro-BNP level.
At one-year follow-up, a significant improvement in EF was documented (from 27±9.8% to 34.7±10.4%; p=0.002). Echocardiography showed a significant reduction in LV dimensions: LV end-diastolic diameter decreased from 70±7.8 mm to 64±7.8 mm (p=0.003) and LV end-diastolic volume from 202.3±63.8 ml to 174.3±59.4 ml (p=0.003); sPAP decreased from 49±15 mmHg to 44±2.6 mmHg (p=0.08) and 86% of the patients were in NYHA Class I-II at one-year follow-up. A significant improvement was documented with all the quality of life assessments: MLHFQ was 22±18.5, SF-36 physical domain was 41.9±10.6, and SF-36 mental domain was 46.4±10.7 (p<0.000, p<0.0001 and p=0.002 compared to preoperative values, respectively). A significant improvement in 6MWT performance was observed (328.7±80.1 m; mean improvement 108 m; p<0.0001).
Discussion
Functional MR is associated with a poor prognosis in heart failure patients with post-ischaemic or idiopathic dilated cardiomyopathy19,20. Surgical mitral valve repair may be considered in severely symptomatic patients with severe FMR despite optimal medical therapy and cardiac resynchronisation therapy21. Although several studies have reported reverse LV remodelling and improvements in symptoms and quality of life after surgical mitral repair4,22, operative mortality is not negligible, ranging from 8.8% to 21%23-25. Moreover, the number of patients with severe FMR who are not referred for surgery because of high surgical risk, advanced age and comorbidities is increasing6. On the basis of the good results that have been reported with the surgical treatment of FMR with the edge-to-edge technique26, percutaneous edge-to-edge with MitraClip implantation has been used for FMR in high-risk patients with favourable safety and efficacy results10-14,27.
The safety and efficacy of the percutaneous edge-to-edge with MitraClip has been initially tested in the EVEREST I trial8, and then compared to surgery in the randomised EVEREST II trial9. However, most of the patients enrolled in the EVEREST trials had degenerative MR and all patients were surgical candidates.
The real-world setting is very different from the original EVEREST trials: most of the patients treated with MitraClip are at high surgical risk and MR is more often functional rather than degenerative. Several clinical experiences with satisfactory acute and midterm results have now been reported in the literature10-14,27.
Recently, the new European guidelines included the MitraClip as a treatment option in high-risk and inoperable patients with FMR and severe symptoms despite optimal medical therapy (class IIb indication with evidence C), reflecting that there is still a scarcity of data to make stronger recommendations16.
In this study, the single-centre experience with the percutaneous treatment of FMR in selected high-risk patients was reported. The results observed in the present study compare favourably to those reported in the largest real-world registries: in the ACCESS-EU study13, 30-day mortality in patients with FMR (393 patients; logistic EuroSCORE 24.8±18.9%; 67% of the patients with EF <40%) was 2.8%; in the TRAMI registry (1,064 patients, 590 with FMR; logistic EuroSCORE about 20%)14, observed 30-day mortality was 6.7% and 4.7% in patients younger than 76 years and patients older than 76 years, respectively.
In our experience, MitraClip therapy is associated with very low hospital mortality (1.8%), short postoperative LOS (median five days) and the postoperative course was smooth in the majority of the patients, despite the high-risk profile at baseline (48% of the patients had a logistic EuroSCORE ≥20%, with a mean EF of 28±11%). Procedural success was 99%. Moreover, 65% of the patients were discharged directly home. The relatively higher 30-day mortality reported in the ACCESS and TRAMI registries may reflect the fact that they are real-world registries, in which many procedures, at least at the beginning of the enrolment, were done in very sick patients as a compassionate and probably futile treatment. The low mortality and extremely low morbidity reported in our experience point out the importance of careful patient selection to identify patients who could really benefit from the procedure and to reduce procedural risk.
Midterm follow-up confirmed the clinical benefit of MitraClip therapy in this setting: 86% of the patients were in NYHA Class I-II one year after the procedure, and a significant improvement in perceived quality of life and functional capacity was documented (mean improvement at 6MWT performance of 120 m). These results are consistent with those reported in the ACCESS-EU study13. Similar to other recent reports27, left ventricular reverse remodelling was observed at one-year echocardiography, which has been associated with favourable outcome in the surgical experience4.
Surgical experience showed that residual MR after surgical repair is associated with poor outcome4,24. Recently, Paranskaya et al showed that residual MR grade is a predictor of one-year adverse events after MitraClip treatment28. In our experience, all the patients who underwent MitraClip therapy had an acute reduction in MR grade after the procedure, with pre-discharge echocardiography showing residual MR ≤2+ in 87% of the patients.
In our study, a preoperative level of pro-BNP ≥1,600 pg/ml was identified as an independent predictor of death at follow-up. Plasma levels of pro-BNP are a useful tool to predict mortality and readmission in heart failure patients and may be used for risk stratification in this setting29,30. Recently, Hwang et al reported that elevated preoperative plasma BNP levels in patients with chronic severe MR undergoing surgery predict poor postoperative outcome31.
Neuss et al showed that the preprocedural pro-BNP level was a powerful predictor of poor outcome (composite primary endpoint of all-cause mortality, LV assist device implantation, mitral valve surgery, and unsuccessful implantation), suggesting that in patients with end-stage heart failure and dramatically increased pro-BNP level (>10,000 pg/ml) MitraClip treatment was not able to improve the clinical course32.
In our experience, we also found that a lower threshold of pro-BNP level (≥1,600 pg/ml) was an independent predictor of reduced survival after MitraClip treatment in patients with FMR, suggesting that pro-BNP measurement should be considered for assessing postprocedural outcome and might be useful for defining the appropriate timing decision of the procedure, which should ideally be performed earlier, before the end-stage phase of the disease. Our finding confirms the important role of pro-BNP dosage for proper patient selection.
We observed a higher risk of recurrence of significant MR in patients with preoperative TR 3-4+. In all the patients with preoperative TR ≥3+ who had MR recurrence at follow-up, the mechanism of MR recurrence was recurrent leaflet tethering due to ongoing LV remodelling. Although this finding may suggest a possible prognostic role of preoperative TR grade in patients with functional MR undergoing MitraClip treatment, no differences in terms of survival were observed. The adherence to the EVEREST criteria (which were totally fulfilled in fewer than 50% of the patients) was not associated with the anatomical results, suggesting that new specific criteria are required. However, longer follow-up would be required to determine the real clinical impact of residual MR.
Limitations
This study was an observational, retrospective single-centre study. Therefore, the sample size was too small to make firm conclusions. Moreover, the results include an initial learning curve.
Conclusions
In conclusion, this study shows that MitraClip therapy is a safe procedure in selected high-risk patients with FMR and can be accomplished with low morbidity and mortality. Moreover, MitraClip treatment is associated with an improvement in functional status and quality of life at one year as well as significant LV reverse remodelling. Although an acute reduction of MR can be obtained in the majority of patients after MitraClip, further studies are needed to determine the clinical impact of residual MR after MitraClip implantation. Thus, MitraClip is a valuable clinical option in patients with adequate anatomy who are considered inoperable or with a high surgical risk and should be considered as an important therapeutic modality in the multidisciplinary treatment of heart failure.
| Impact on daily practice MitraClip therapy for FMR is a valuable alternative to surgery in high-risk or inoperable patients. The results of this study show that in daily clinical practice patient selection is the key to improving safety and efficacy. Patients with advanced heart failure have suboptimal outcomes despite MitraClip implantation, and their treatment should be based on a very individualised decision. |
Conflict of interest statement
F. Maisano is a consultant for Abbott Vascular. The other authors have no conflicts of interest to declare.

