Abstract
Aims: Treatment strategies of high-risk patients with mitral regurgitation (MR) differ between disease based on functional and disease based on degenerative origin. In the present study, we aimed to evaluate the effect of surgical, percutaneous, or conservative treatment of MR according to MV mechanism, for high-risk patients.
Methods and results: Survival outcomes of MitraClip, surgical, or conservative strategies were compared for 688 high-risk patients with functional MR and 275 with degenerative MR. Cox regression and propensity analyses were used to correct for differences in baseline characteristics. For functional MR, conservative treatment proved to have a higher mortality hazard when compared to MitraClip treatment (hazard ratio [HR] 1.79, 95% confidence interval [CI]: 1.34 to 2.39, p<0.001), while there was no significant difference in mortality hazard between MitraClip and surgery (HR 0.86, 95% CI: 0.54 to 1.38, p=0.541). For degenerative MR, no clear significant benefit was found when comparing MitraClip to conservative and surgical treatment.
Conclusions: High-risk patients with symptomatic functional MR have reduced mortality when undergoing MitraClip intervention, compared to those receiving conservative treatment.
Abbreviations
DMR: degenerative mitral regurgitation
ESII: EuroSCORE II
FMR: functional mitral regurgitation
LVEF: left ventricular ejection fraction
MR: mitral regurgitation
MV: mitral valve
PH: pulmonary hypertension
SPAP: systolic pulmonary artery pressure
STS: Society of Thoracic Surgeons
Introduction
BACKGROUND
The population of patients with mitral regurgitation (MR) is inhomogeneous. This is partially the result of the different mechanisms that lie at the base of this disease, each being associated with different comorbidity profiles. The aetiology of MR may be divided roughly into primary/organic or degenerative MR (DMR) in which the valve apparatus itself is diseased, and secondary or functional MR (FMR) in which mitral valve (MV) dysfunction is secondary to left ventricular disease1. Also, a distinction among patients can be made based on the level of assessed surgical risk2. Hence a “typical MR patient” is non-existent and consequently no “one size fits all” treatment is available.
CONTEMPORARY KNOWLEDGE
Contemporary ESC (2017) and AHA/ACC (2017) guidelines recommend choosing between surgery, percutaneous, and conservative treatment based on symptom burden, estimated surgical risk, and MV aetiology3,4. Surgical repair/replacement is the gold standard if prognosis benefit is to be expected, if MV repair/replacement is assessed as technically feasible, and if patient risk is not too high. High-risk patients with DMR may be considered for percutaneous therapy, of which MitraClip is currently the most widely used, if surgery is not warranted. For high-risk patients with FMR, a similar strategy is recommended only by the ESC guidelines, whereas the AHA/ACC guidelines do not mention percutaneous treatment for such patients. Medical treatment should be considered as appropriate in both populations3,4. The recommendations for MitraClip in high-risk patients with FMR is based on one one-arm observational study5, while publications which compared treatment of high-risk patients with MitraClip to more established therapeutic options for survival outcome remain scarce6-8. This is also true for specific subpopulations based on MV aetiology9-12.
HYPOTHESIS
In the present study we aimed to evaluate the effect of surgical, percutaneous, or conservative treatment of MR according to MV mechanism, for high-risk patients.
Methods
PATIENT SELECTION
Previously acquired data were used13. In short, data were gathered retrospectively from 1,036 high-risk patients with moderate-severe (grade 3/4) or severe (grade 4/4) symptomatic MR8. Patients from four centres were included. Between January 2009 and April 2016, 568 consecutive patients were treated using the MitraClip® (Abbott Vascular, Santa Clara, CA, USA) (Supplementary Table 1A). Control groups comprising 173 surgically treated patients (Supplementary Table 1B) and 295 conservatively treated patients (Supplementary Table 1C) were included. Patients from the two control groups were selected based on timing of MR diagnosis (for each centre, a selection period of two years prior to first MitraClip was used ranging from January 2007 to June 2012) and the high-risk criteria used by the Heart Team8,13. Patients with a logistic EuroSCORE (LES) ≥20%, age ≥80 years, left ventricular ejection fraction (LVEF) <30%, previous cardiac surgery, pulmonary hypertension, renal insufficiency (defined as glomerular filtration rate <45 ml/min/1.73 m²), underweight or severe overweight, previous chest radiation, chronic obstructive pulmonary disease and emphysema, porcelain aorta, or frailty were deemed high-risk. Only patients who had previously been judged as having either DMR or FMR were used for the current analyses, while patients with mixed (both degenerative and functional) MR were excluded.
VARIABLES
Surgical risk scores were determined by using online calculators (www.euroscore.org, riskcalc.sts.org). Renal insufficiency was defined as an estimated glomerular filtration rate <45 ml/min/1.73 m2. The presence of pulmonary hypertension (PH) was determined by using echocardiographic estimated systolic pulmonary artery pressure (SPAP), which was derived from tricuspid regurgitation gradient and estimated right atrial pressure. SPAP was subsequently categorised into “no PH” (unmeasurable or SPAP <31 mmHg), “moderate PH” (SPAP ≥31 and <56 mmHg), or “severe PH” (SPAP ≥56 mmHg). All other characteristics were retrospectively obtained from patient files13. All-cause mortality data were collected by consulting the governmental death registry using social security numbers.
STATISTICAL ANALYSIS
Continuous variables are presented as mean±SD, discrete variables as proportions. Comparisons between groups were carried out by using the one-way ANOVA test between groups for parametric data, with subsequent use of the Tukey honest significant difference post hoc test. Ordinal data were compared using the Kruskal-Wallis H and Dunn’s multiple comparison tests while nominal data were compared using the chi-square test with Bonferroni adjustment.
For survival analysis, Kaplan-Meier estimates were created whereas comparisons were performed using log-rank statistics. We used a univariate Cox proportional hazards model to identify predictors of mortality. To counter imbalances in baseline differences and identify independent predictors, we used a manual backwards stepwise selection of significant variables. Baseline variables that had a significance of p<0.10 in univariate analysis were entered into the multivariate model, with the exception of surgical risk scores. SPSS, Version 24.0 (IBM Corp., Armonk, NY, USA) was used for basic analyses. Additionally, we tried to reduce confounding influences with propensity weighting and by using all variables with a p<0.05 in the Cox model. For the statistical analyses regarding the propensity score, we used the R statistical program (www.r-project.org) version 3.3 (R Foundation for Statistical Computing, Vienna, Austria). P-values <0.05 (two-tailed) were considered statistically significant.
Results
FUNCTIONAL MITRAL REGURGITATION
BASELINE
Six hundred and eighty-eight (688) patients had FMR. Mean age was 72.0±11.2 years, EuroSCORE II (ESII) was 7.4±6.8, and LVEF was 33.1±13.1%. Three hundred and sixty-five (365) patients underwent MitraClip treatment (63% one clip, 34% two clips, 3% three clips). Post-interventional MR grade was less than 3/4 in 97%. Respectively, 95 and 228 patients received surgical therapy (80% repair, 20% replacement) and conservative therapy (59% of whom were on beta-blockers, 59% on ACE inhibitors or angiotensin II receptor blockers, 51% on aldosterone antagonists and 89% on diuretics). The treatment groups differed significantly (Table 1). MitraClip patients were older than patients treated by surgical intervention (mean 72.8 versus 67.5 years) but of similar age compared to conservatively treated patients (mean 72.8 versus 72.6 years). Surgical risk scores were highest in the MitraClip group, with a significantly higher ESII compared to surgically and conservatively treated patients (mean 8.9 versus 4.7 and 6.1, respectively). Although MitraClip patients in general were shown to have the least favourable comorbidity profile, LVEF was significantly lower in patients who underwent conservative management (mean 33.0% versus 29.8%).
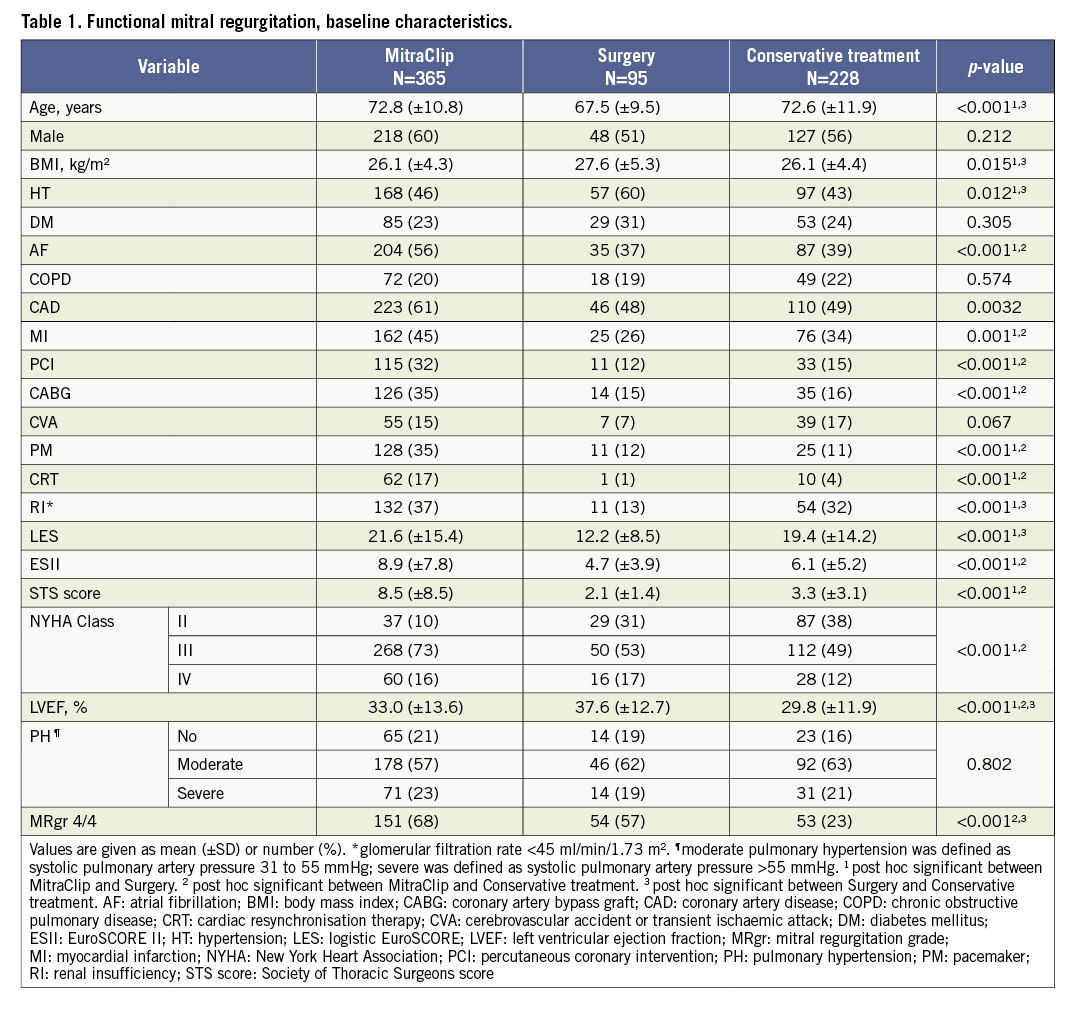
SURVIVAL
Median follow-up of FMR patients was 2.8 (IQR 1.3-5.1) years. For MitraClip patients, follow-up was 2.4 (IQR 1.2-3.6) years. For surgically and conservatively treated patients this was 5.2 (IQR 3.0-6.4) and 3.6 (IQR 1.1-6.1) years, respectively. During three-year follow-up, 122 (33%) patients who underwent MitraClip therapy died. There were 22 (23%) and 102 (45%) observed deaths in the surgery and conservative groups, respectively. Log-rank testing showed a significantly different mortality estimate of p=0.001 (Figure 1). Nominal comparisons using log-rank testing revealed significant differences between MitraClip and surgery (p=0.011) and between MitraClip and conservative treatment (p=0.048). Baseline characteristics associated with mortality outcome were: treatment option, age, body mass index, atrial fibrillation, chronic obstructive pulmonary disease (COPD), myocardial infarction, coronary artery bypass grafting, pacemaker, renal insufficiency, LES, ESII, Society of Thoracic Surgeons (STS) score, New York Heart Association class, and PH. A Cox multivariate prediction model including 683 patients proved that conservative treatment had a higher mortality hazard when compared to MitraClip treatment (HR 1.79, 95% CI: 1.34 to 2.39, p<0.001), while there was no significant difference in mortality hazard between MitraClip and surgery (HR 0.86, 95% CI: 0.54 to 1.38, p=0.541) (Table 2).
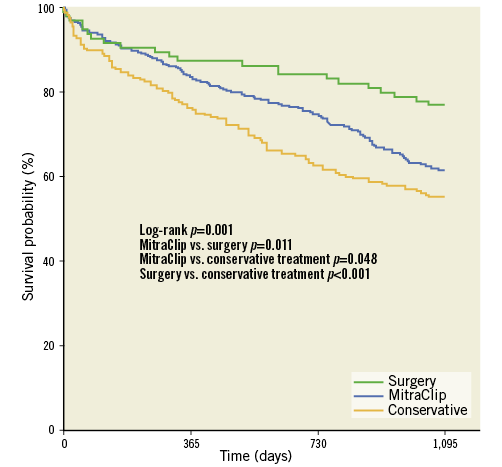
Figure 1. Kaplan-Meier survival estimate of patients with functional mitral regurgitation.
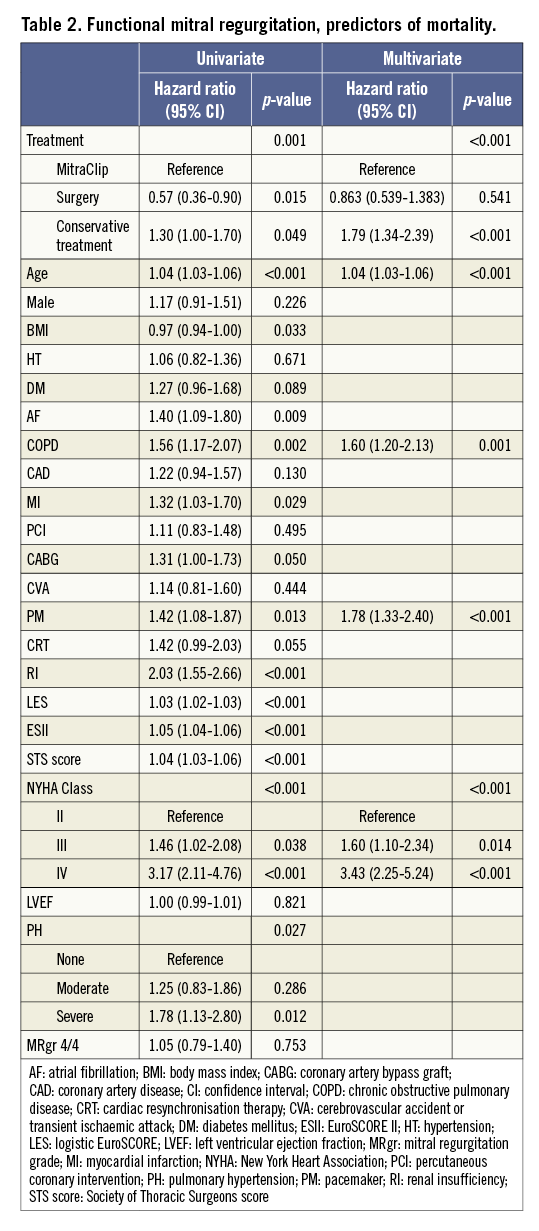
Propensity weighting resulted in an HR of 1.59 (95% CI: 1.18 to 2.13, p=0.002) for conservative treatment compared with MitraClip, and an HR of 1.16 (95% CI: 0.45 to 2.99, p=0.77) for MitraClip compared with surgery.
DEGENERATIVE MITRAL REGURGITATION
BASELINE
There were 275 patients who were identified with DMR. Patients had a mean age of 75.5±9.9 years, an ESII of 5.5±5.1, and an LVEF of 48±13.6%. One hundred and sixty-five (165) patients received MitraClip treatment (56% one clip, 38% two clips, 6% three clips). Reduction of MR to less than 3/4 was achieved in 80%. Sixty-six (66) patients received surgical treatment (69% repair, 31% replacement) and 44 conservative treatment. Similar to the FMR cohort, there were significant baseline differences between the treatment groups (Supplementary Table 2). Remarkably, while MitraClip patients scored significantly higher with surgical risk scores when compared to those in the surgically and conservatively treated groups (mean ESII of 6.5 versus 3.8 and 4.4, respectively) and were older compared to surgically treated patients (mean 75.7 versus 71.4 years), their age was lower compared to conservatively treated patients (mean 75.7 versus 80.8 years). Nonetheless, MitraClip patients had worse comorbidity profiles and LVEF was significantly lower compared to the control groups (mean LVEF 43.7% versus 54.1% and 52.8%).
SURVIVAL
Median follow-up of DMR patients was 2.8 (IQR 1.3-5.0) years. For MitraClip patients, follow-up was 2.0 (IQR 1.0-3.6) years. For surgically and conservatively treated patients this was 5.5 (IQR 3.4-7.3) and 3.3 (IQR 1.6-5.1) years, respectively. Fifty (30%) of the patients who underwent MitraClip therapy died during three-year follow-up, while 15 (23%) surgically treated and 21 (48%) conservatively treated patients died. We chose not to analyse survival differences of the treatment options for DMR, since there were only a few patients in the control groups to compare.
Discussion
In the current study we studied all-cause mortality outcomes of three treatment options for MR, within two high-risk populations diagnosed with either FMR or DMR. For both populations we found that patients treated with surgery had the lowest observed mortality, whereas conservatively treated patients were shown to have the highest mortality rate during follow-up. For patients with FMR, MitraClip was an independent predictor of reduced mortality when compared to conservative therapy, while surgery was not shown to be superior compared to MitraClip treatment in a multivariate model.
FMR
MITRACLIP VS. CONSERVATIVE
The baseline characteristics of the MitraClip cohort were similar or even worse when compared to the conservatively treated group. This may seem odd as one would expect that patients who underwent intervention, albeit minimally invasive, would have a lower risk than those merely treated with medication and/or resynchronisation therapy. A potential explanation could be that, at a time when MitraClip was not available, high-risk patients were less likely to be referred to the cardiologist by the general practitioner since there would be no expected treatment benefit14,15. Another potential cause could be that contemporary patients are more likely to be designated to undergo MitraClip treatment instead of conservative management if there are signs of disease progression, though a recently conducted observational study showed the contrary. A significant difference in baseline MR grade (68% MR grade 4/4 in MitraClip, compared to 23% in the conservative group) in the present study supports the latter.
Nonetheless, three previous studies comparing conservative to MitraClip therapy for patients with FMR have been published. The recently published data of the MITRA-FR randomised controlled trial, in which 152 patients were studied in both arms, showed no significant difference in all-cause mortality between the groups. The writers argue that, for FMR, the potential benefit of intervention on MR reduction might be diminished by the course of progression of heart failure. This outcome contradicts the findings of the present study. However, this trial was not powered to study mortality, and the outcome may have been influenced by the lack of MitraClip experience in the participating centres16. Giannini et al presented the results of a study involving 160 patients, in which the Kaplan-Meier survival analysis resulted in three-year mortality rates of 38.6% and 65.1% (p=0.007) for the MitraClip and conservative groups, respectively9. The COAPT trial, primarily designed to study hospitalisation rates, is another recently published study which randomised between MitraClip and conservative treatments for patients with secondary MR: 302/312 patients were included for each arm and, in contrast to MITRA-FR, this study was actually also powered for secondary outcomes such as survival. The investigators found that two-year mortality for patients treated with MitraClip was 29.1% versus 46.1% for those who received conservative therapy (HR 0.62, p<0.001)17. Our present finding, that conservative treatment has an increased adjusted mortality hazard when compared to MitraClip (HR 1.79, p<0.001), adds to the argument for treating patients with the latter if MV anatomy permits. One explanation for better survival among patients treated with MitraClip may be the potential positive effect of repair on left ventricle remodelling18, since LVEF and MR grade19 are both associated with mortality. Another cause could be that patients who were treated with MitraClip received a higher standard of heart failure care through better outpatient follow-up. Also, when comparing the two recently published randomised trials16,17 and the present study, we see that there might be a correlation between pre-interventional MR grade and survival benefit of MitraClip intervention: in MITRA-FR, roughly 60% of the included MitraClip patients had MR grade 4/4; for the present study this was roughly 70%. In COAPT this was roughly 50%; however, their definition of grade 4/4 was stricter, with both higher mean effective regurgitant orifice area and higher mean regurgitant volume. It makes sense that greater potential MR reduction by intervention may lead to greater survival benefit. Also, in MITRA-FR, MR grade reduction to 2/4 or less was achieved in 91%; in the present study this was 93% and for COAPT this was 95%.
MITRACLIP VS. SURGERY
Despite having used similar inclusion criteria to identify high-risk patients, our surgical cohort showed markedly more favourable characteristics when compared to the MitraClip group. This is not surprising since surgical therapy for high-risk patients with FMR was not – and is not – indicated according to European guidelines, whereas MitraClip treatment of such patients may currently be considered (indication class 2b, level of evidence C)4. Indeed, patient profiles from other observational studies of FMR treatment show similar discrepancies between MitraClip and surgical cohorts11,12,18. More importantly, none of these studies found a significant difference in adjusted mortality hazard. It is not surprising that our high-risk surgical cohort was probably highly selected, having a more favourable baseline profile (i.e., mean age 67.5 versus 72.8 years, p<0.001), and therefore was shown to have a better survival outcome when compared to our MitraClip group. We hypothesise that, when correcting for baseline differences, the survival hazard is similar because for FMR other factors that make up this disease, such as (ischaemic) reduced LVEF, contribute more to prognosis than mitral insufficiency itself20. In other words, reducing MR by either surgical or percutaneous intervention does not entirely reverse the clinical problem at hand. This preliminary knowledge will have to be confirmed by the ongoing MATTERHORN randomised controlled trial that is expected to be completed in December 2019 (ClinicalTrials.gov Identifier: NCT02371512).
DMR
We found significant baseline differences for the studied DMR cohorts. In short, the conservatively treated patients had the highest mean age, while the MitraClip patients seemed to have the highest surgical risk scores. Unfortunately, we were not able to include significant numbers of surgically or conservatively treated patients. Such factors made us decide not to perform comparative analyses, since we did not feel that we would be able to draw fair conclusions from the results because of significant selection bias.
Limitations
For this study we retrospectively tried to form matching control groups according to high-risk characteristics such as advanced age or presence of previous cardiac surgery. Still, there were significant differences at baseline that made the inclusion criterion “high-risk” more flexible than anticipated, which may have confounded our outcomes. By using a multivariate model and propensity scoring/matching we could partially neutralise this selection bias; however, the methodology used does not control for unknown confounders. By using previously collected data, we could only study all-cause mortality outcomes. One could argue that knowledge about survival benefit is less essential for a high-risk population burdened with several quality-of-life-reducing comorbidities. Therefore, our preliminary findings should only be used as a complementary factor for decision making. For DMR, we did not perform comparative analyses between the treatment options because of significant selection bias.
Conclusions
High-risk patients with symptomatic functional mitral regurgitation seem to have reduced mortality when undergoing MitraClip intervention compared to those receiving conservative treatment. Our findings need to be supported by future randomised trials designed primarily for studying mortality outcomes.
| Impact on daily practice For functional mitral regurgitation no clear survival benefit of surgery has been shown compared to conservative treatment. The recently published MITRA-FR trial also could not show a clear survival benefit of MitraClip. However, debate continues since the COAPT trial did actually publish evidence of MitraClip superiority over conservative management. The current study supports the finding of the COAPT trial, by showing a superior survival of MitraClip patients when compared to those treated conservatively. Additionally, the present study demonstrated a non-inferiority outcome of MitraClip patients with functional mitral regurgitation compared to similar patients who underwent surgical management. |
Funding
A grant from Abbott Vascular was used to maintain a MitraClip registry at the St. Antonius Hospital.
Conflict of interest statement
B.J. Van den Branden has received a speaker’s fee and is a proctor for Abbott. M.J. Swaans has received personal fees from Abbott Vascular and Boston Scientific for proctoring, and from Philips Healthcare for lecturing. J. Baan Jr has received an unrestricted research grant from Abbott Vascular and is a proctor for Abbott Vascular. J.A. Van der Heyden has received a grant from Abbott. R. Schurer has received personal fees from Abbott and is an occasional proctor for Abbott Vascular. The other authors have no conflicts of interest to declare.
Supplementary data
Supplementary Table 1A. MitraClip cohort.
Supplementary Table 1B. Surgical cohort.
Supplementary Table 1C. Conservative cohort.
Supplementary Table 2. Degenerative mitral regurgitation, baseline characteristics.
To read the full content of this article, please download the PDF.