In 2018, two randomised clinical trials of transcatheter edge-to-edge mitral valve repair (TMVr) for functional mitral regurgitation (FMR) reported very different outcomes. The MITRA-FR trial showed no statistically significant difference in the combined endpoint of death or hospitalisation for heart failure (HF) at one year1. The COAPT trial showed marked improvements in total HF hospitalisations at two years, as well as mortality and multiple other pre-specified secondary endpoints2. We hypothesised that the divergent outcomes of the two trials could be explained largely by enrolment of different patient populations3. Patients in COAPT had a larger mean effective regurgitant orifice area (EROA) and smaller left ventricular end-diastolic volume (LVEDV), a finding we termed disproportionately severe MR. In contrast, MITRA-FR enrolled patients with proportionately severe MR characterised by smaller EROA and larger LVEDV. Figure 1 shows typical examples of these subtypes of FMR and why they might respond differently to medical therapy for HF versus mitral intervention.
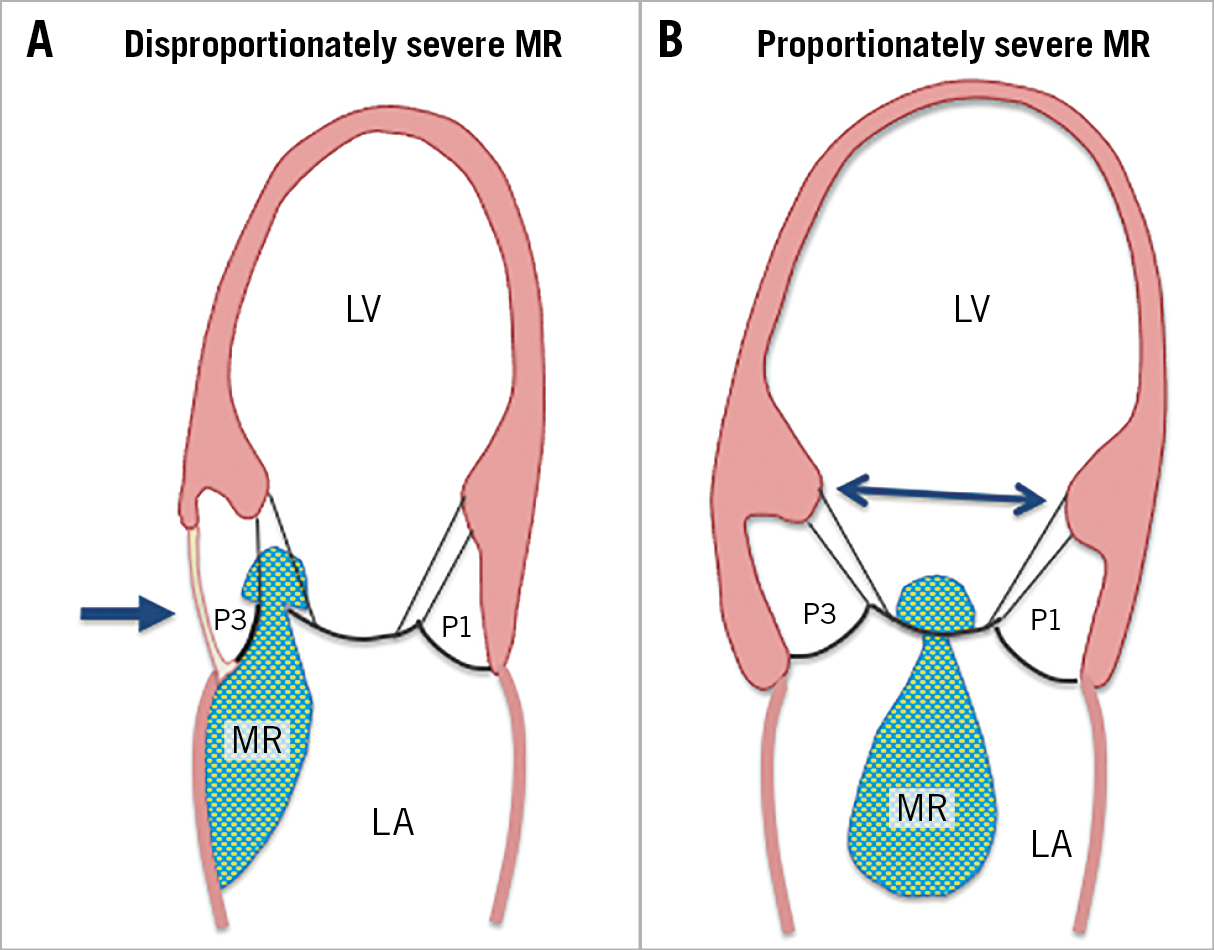
Figure 1. Schematic diagrams of patients with disproportionately severe and proportionately severe FMR. A) Disproportionately severe FMR. In this example, the patient has a focal inferobasal infarct (arrow) with asymmetric tethering of the posterior medial scallop (P3) toward the apex. The lateral scallop (P1) is unaffected. Overall, LV size and shape are not severely dilated, and LV systolic function is preserved. Medical therapy is not likely to reduce MR severity because the focal wall motion abnormality is scar. B) Proportionately severe FMR. This patient has symmetric tethering of the entire posterior leaflet due to global LV dilation/dysfunction with displacement of both papillary muscles (arrow). Medical therapy could induce significant reverse LV remodelling, which could improve FMR by repositioning of the papillary muscles. If such patients are first treated with titration of neurohormonal antagonists to target doses, only those patients in whom FMR is not improved will require mitral intervention.
In this issue of EuroIntervention, Adamo et al report the results of TMVr in 137 patients with FMR at three centres from 2008-2016. The mean age was 70 years, 80% were male and most had NYHA Class III or IV heart failure symptoms4.
Roughly half had ischaemic aetiology. Patients were categorised as having proportionate versus disproportionate MR based on median values of echocardiographic measurements of EROA and LVEDV. Overall, patients were similar to those in COAPT in terms of EROA and LVEDV, with 78% having disproportionately severe MR and 22% proportionately severe MR. Clinical and demographic variables were well balanced between the groups, except that estimated pulmonary artery systolic pressure was higher in those with disproportionately severe MR (49±12 vs 40±13 mmHg, p<0.001). A combined endpoint of death or HF hospitalisation at two years was not statistically significantly different between the proportionality groups (p=0.318), nor was mortality significantly different. On multivariable analysis, statistically significant predictors of outcomes were EuroSCORE II >8%, NYHA class and more than mild residual MR, but not disproportionately severe MR.
Adamo et al convincingly demonstrate no difference in death or HF hospitalisation for disproportionate versus proportionate FMR after TMVr. These findings are consistent with a larger European registry of 1,016 patients showing no difference in mortality at two years across proportionality groups after TMVr5. On the surface, these data could be interpreted to mean that the concept of disproportionately severe FMR does not predict response to TMVr. However, it is important to point out that registries cannot determine response to TMVr since there is no control group of patients treated only with HF medical therapy. It is well known that FMR can respond to neurohormonal antagonists that improve survival in HF6,7,8. In the Adamo study, patients were treated with optimal medical therapy prior to TMVr, thus selecting a group of patients who continued to have symptomatic severe FMR despite medical therapy. It is encouraging that the registry patients have values of EROA and LVEDV similar to those in COAPT, where randomisation occurred after optimisation of medical therapy. Therefore, both the registry data and COAPT are dominated by disproportionately severe MR. Because FMR is secondary to LV dysfunction, mortality and/or HF hospitalisation could be driven primarily by the FMR itself, the underlying LV dysfunction or a combination of both. By first optimising medical therapy and re-evaluating FMR severity and LV function, one can target TMVr to appropriate patients. This will bias the population towards those with disproportionately severe MR who have been shown to have a very poor outcome with medical therapy in a single-centre report9 and in COAPT3. It will also include a smaller group of patients with proportionate MR who fail to respond to medical therapy, perhaps because of limited reverse LV remodelling, intolerance to target doses of neurohormonal antagonists, or unknown reasons. Unfortunately, there is recent evidence that very few HF patients are on optimal doses of all three major classes of neurohormonal antagonists10. The cardiology community needs to improve the appropriate use and up-titration of medical therapy for patients with HF, including those with FMR. It is strongly encouraging that the typical FMR patients treated in European registries appear to resemble COAPT patients closely because those are the patients who have been proven to benefit from TMVr.
Conflict of interest statement
P.A. Grayburn was a COAPT trial investigator, sponsored by Abbott Vascular. A. Sannino received research funding from Edwards Lifesciences.
Supplementary data
To read the full content of this article, please download the PDF.