Abstract
BACKGROUND: The prognostic benefits of transcatheter edge-to-edge repair (TEER) remain unclear in patients with atrial functional mitral regurgitation (AFMR).
AIMS: We aimed to investigate the clinical outcomes of TEER for patients with AFMR.
METHODS: We retrospectively classified functional mitral regurgitation (FMR) patients undergoing TEER into those with AFMR or ventricular FMR (VFMR). A residual MR ≤1+ at discharge was considered optimal mitral regurgitation (MR) reduction, and an elevated mean mitral valve pressure gradient (MPG) was defined as an MPG ≥5 mmHg at discharge. The primary outcome was a composite of all-cause mortality and hospitalisation due to heart failure within one year.
RESULTS: Of 441 FMR patients, 125 patients were considered as having AFMR. Residual MR ≤1+ was associated with a lower risk of the composite outcome in both AFMR and VFMR patients, while an MPG ≥5 mmHg was associated with a higher risk of the composite outcome in patients with AFMR but not with VFMR. AFMR patients with residual MR ≤1+ and an MPG ≥5 mmHg, as well as those with residual MR >1+, had a higher incidence of the composite outcome than those with residual MR ≤1+ and an MPG <5 mmHg (50.7%, 41.8%, and 14.3%, respectively; p<0.001). This association was consistent after adjustment for clinical and echocardiographic characteristics.
CONCLUSIONS: An MR reduction to ≤1+ following TEER was associated with a lower risk of clinical outcomes in patients with AFMR, while an MPG ≥5 mmHg was related to a higher risk of clinical outcomes. Optimal MR reduction by TEER may have potential benefits on the prognosis of patients with AFMR, although the prognostic benefit may be attenuated by an elevated MPG.
Functional mitral regurgitation (FMR) is defined as mitral regurgitation (MR) that is mainly caused by an abnormality of left-sided heart function and geometry, as opposed to degenerative MR which is caused by intrinsic structural valve changes1. Growing insights into the pathophysiology of FMR have revealed two subtypes: atrial FMR (AFMR) and ventricular FMR (VFMR)23. While VFMR is attributed to underlying left ventricular (LV) remodelling or dysfunction, AFMR is caused by the enlargement of the left atrium and subsequent mitral annular dilation. According to recent studies, a non-negligible number of patients with FMR are considered to have AFMR, with increased mortality and morbidities45. Given the differences in underlying cardiac remodelling, it is necessary to manage these patients in a manner tailored to the subtype of FMR.
Transcatheter edge-to-edge repair (TEER) is an established alternative option for patients with MR who are considered high risk for cardiac surgery67. The COAPT trial, a randomised control trial comparing TEER with medical therapy, has revealed the prognostic benefit of TEER in VFMR patients7; however, evidence regarding the prognostic impact of TEER for patients with AFMR is still limited. Prior studies indicate the effectiveness of TEER in reducing MR in AFMR patients8910; however, the question as to whether an MR reduction ultimately improves clinical outcomes in patients with AFMR remains unanswered.
Reducing MR by TEER entails the risk of generating relevant mitral stenosis. An elevated mean mitral valve pressure gradient (MPG) after TEER is associated with impaired prognosis in patients with degenerative MR1112. However, this association may be less significant in patients with FMR121314, and prior studies have mainly focused on VFMR. Given the differences in underlying cardiac remodelling, the association between an elevated MPG and prognosis might differ for AFMR and VFMR.
In the present study, we therefore investigated the association of MR reduction and an elevated MPG with clinical outcomes after TEER in patients with AFMR specifically.
Methods
STUDY POPULATION
This study was designed as a retrospective analysis of data from the Bonn registry, which is a prospective, consecutive collection of patient data from the Heart Center Bonn. We identified consecutive symptomatic patients with moderate-to-severe or severe FMR who had undergone TEER between September 2010 and March 2022. Patients with a prior history of surgical or transcatheter mitral valve interventions were excluded from this analysis. All the included patients were deemed ineligible or high-risk for conventional surgery. A standard diagnostic workup was performed, including transthoracic (TTE) and transoesophageal echocardiography (TOE) and left heart catheterisation. The decision about the form of treatment for MR was determined by the interdisciplinary Heart Team at the Heart Center Bonn. The present study was approved by the institutional ethics committee and conducted in concordance with the Declaration of Helsinki. All participants in this study provided written informed consent.
ECHOCARDIOGRAPHIC ASSESSMENTS
All patients underwent TTE and TOE before the TEER procedure. All echocardiographic assessments were performed according to current guidelines15. At the apical two- and four-chamber views, LV end-diastolic and end-systolic and left atrial (LA) volumes were evaluated. LV and LA volumes were indexed by body surface area. The severity of MR was determined based on qualitative and quantitative criteria adapted from Mitral Valve Academic Research Consortium (MVARC) guidelines16. MR was categorised as 0 (none), 1+ (mild), 2+ (moderate), 3+ (moderate-to-severe), and 4+ (severe).
The aetiology of MR was evaluated based on current expert opinion17. Before the procedure, the aetiology of MR was prospectively classified into degenerative or functional MR by experienced echocardiographers. For the current analysis, FMR was retrospectively classified into AFMR and VFMR as follows. AFMR was defined as cases that met all of the following criteria: 1) normal LV systolic function (i.e., LV ejection fraction >50%); 2) no or mild LV enlargement (LV end-diastolic volume index: ≤89 ml/m2 for male and ≤70 ml/m2 for female) without segmental LV wall abnormality18; and 3) moderate or severe LA enlargement (LA volume index: ≥42 ml/m2)18. Patients lacking any one of these criteria were considered to have VFMR.
Residual MR and MPG after TEER were assessed using transthoracic echocardiography at discharge. Residual MR was assessed using qualitative and semiquantitative parameters, according to the current guidelines19. MPG was measured using a continuous-wave Doppler of the mitral inflow during diastole by tracing the entire forward flow contour from the apical views20. Residual MR ≤1+ was considered optimal MR reduction, and an elevated MPG was defined as an MPG ≥5 mmHg21. According to their residual MR and MPG at discharge, patients were stratified into three groups: 1) residual MR ≤1+ with an MPG <5 mmHg, 2) residual MR ≤1+ with an MPG ≥5 mmHg, and 3) residual MR >1+.
PROCEDURE
The procedures were performed using the MitraClip system (Abbott) or PASCAL system (Edwards Lifesciences) under general anaesthesia with three-dimensional TOE and fluoroscopic guidance.
OUTCOME MEASURES
The primary outcome was a composite of all-cause mortality and hospitalisation due to heart failure within one year of TEER. All clinical events, including hospitalisation due to heart failure, were independently adjudicated by the local Heart Team based on the criteria of the MVARC guidelines21. The occurrence of clinical events was obtained from admission and outpatient medical records, telephone interviews, or documentation from the referring general practitioners.
STATISTICS
Continuous variables are presented as mean±standard deviation or median with an interquartile range (IQR) and were compared using the Student’s t-test or Wilcoxon test. Cross-sectional comparisons among groups were made using either the ANOVA or Kruskal-Wallis test. Categorical data are presented as numbers with percentages and were compared by the chi-square or Fisher’s exact tests. New York Heart Association (NYHA) Functional Class was compared between baseline and the last follow-up using Bowker’s test. Time-to-event curves are depicted using the Kaplan-Meier method and compared between groups using the log-rank test. Univariate and multivariable Cox proportional hazard models were used to calculate hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) for the outcomes. Covariates in the multivariable model were predefined based on the presumed association with clinical outcomes and were divided into two models. Model 1 included age, male sex, atrial fibrillation, and estimated glomerular filtration rate; model 2 included LV ejection fraction, LA volume index, systolic pulmonary artery pressure, and severity of tricuspid regurgitation (TR). We generated three-knot spline curves to show the relationship between the MPG and its hazard risk in patients with AFMR and VFMR. Statistical significance was set as a 2-sided p<0.05. All analyses were conducted using Stata/SE 15.1 (StataCorp) or R version 4.3.1 (R Foundation for Statistical Computing).
Results
STUDY POPULATION
A total of 441 patients with FMR who underwent TEER were included in the present analysis. The mean age was 77±8 years, and 56.7% of patients were male. The median European System for Cardiac Operative Risk Evaluation (EuroSCORE) II was 4.14% (IQR: 2.68-7.23%) (Supplementary Table 1).
Of these 441 patients, 125 (28.3%) were classified as having AFMR. The baseline characteristics of patients with AFMR are shown in Table 1. Patients with AFMR were older and more frequently female than those with VFMR (Supplementary Table 1). The proportion of atrial fibrillation was higher in patients with AFMR than in those with VFMR. In contrast, prior histories of coronary artery disease and cardiac implantable electronic devices were more frequent in patients with VFMR than in those with AFMR. Patients with VFMR were also considered at a higher risk for cardiac surgery than those with AFMR (EuroSCORE II: 4.71% [IQR: 2.86-8.07%] vs 3.40% [IQR: 2.39-4.97%]; p<0.001).
Echocardiographic assessment at baseline showed that patients with AFMR had a higher LV ejection fraction, a smaller LV volume and a larger LA volume than those with VFMR. The MPG at baseline was more likely to be higher in patients with AFMR, compared to in those with VFMR (1.7 mmHg [IQR: 1.3-2.6 mmHg] vs 1.5 mmHg [IQR: 1.1-2.2 mmHg]; p=0.058), while the severity of MR was comparable between the two groups. The mitral annular diameter was greater in patients with AFMR than in those with VFMR (38 mm [IQR: 35-43 mm] vs 37 mm [IQR: 33-40 mm]; p<0.001). Severe or greater TR was more frequent in patients with AFMR than in those with VFMR (48.0% vs 26.3%; p<0.001).
Table 1. Baseline characteristics of patients with AFMR.
| Residual MR ≤1+ | |||||
|---|---|---|---|---|---|
| Totaln=125 | MPG <5 mmHgn=75 | MPG ≥5 mmHgn=21 | Residual MR >1+n=29 | p-value | |
| Age, years | 80.0±6.5 | 80.7±6.0 | 80.7±7.0 | 77.9±7.0 | 0.12 |
| Male | 54 (43.2) | 30 (40.0) | 7 (33.3) | 17 (58.6) | 0.14 |
| BMI, kg/m2 | 27.2±5.6 | 28.9±6.6 | 26.3±3.8 | 24.1±2.5 | 0.014 |
| EuroSCORE II, % | 4.2±2.8 | 4.0±2.7 | 4.8±2.6 | 4.2±3.0 | 0.48 |
| Diabetes | 30 (24.0) | 18 (24.0) | 6 (28.6) | 6 (20.7) | 0.81 |
| Hypertension | 101 (80.8) | 65 (86.7) | 16 (76.2) | 20 (69.0) | 0.10 |
| Coronary artery disease | 55 (44.0) | 32 (42.7) | 10 (47.6) | 13 (44.8) | 0.92 |
| Prior myocardial infarction | 15 (12.0) | 8 (10.7) | 2 (9.5) | 5 (17.2) | 0.61 |
| Prior PCI | 45 (36.0) | 26 (34.7) | 8 (38.1) | 11 (37.9) | 0.93 |
| Prior CABG | 19 (15.2) | 10 (13.3) | 5 (23.8) | 4 (13.8) | 0.48 |
| Prior stroke | 9 (7.2) | 5 (6.7) | 2 (9.5) | 2 (6.9) | 0.90 |
| Atrial fibrillation | 116 (92.8) | 69 (92.0) | 19 (90.5) | 28 (96.6) | 0.65 |
| NYHA Functional Class | 0.30 | ||||
| II | 19 (15.2) | 11 (14.7) | 4 (19.0) | 4 (13.8) | |
| III | 91 (72.8) | 58 (77.3) | 12 (57.1) | 21 (72.4) | |
| IV | 15 (12.0) | 6 (8.0) | 5 (23.8) | 4 (13.8) | |
| COPD | 26 (20.8) | 15 (20.0) | 4 (19.0) | 7 (24.1) | 0.88 |
| Pacemaker, ICD, or CRT | 30 (24.0) | 16 (21.3) | 6 (28.6) | 8 (27.6) | 0.69 |
| eGFR, ml/min/m2 | 49.3±18.4 | 50.0±18.1 | 42.5±13.5 | 52.6±21.4 | 0.14 |
| Haemodialysis | 1 (0.8) | 1 (1.3) | 0 (0.0) | 0 (0.0) | 0.71 |
| NT-proBNP, pg/ml | 1,986 (1,403-4,019) | 1,954 (952-3,607) | 2,048 (1,561-3,964) | 1,954 (1,691-7,155) | 0.17 |
| Beta blockers | 98 (78.4) | 59 (78.7) | 16 (76.2) | 23 (79.3) | 0.96 |
| RAS inhibitors | 84 (67.2) | 55 (73.3) | 13 (61.9) | 16 (55.2) | 0.18 |
| MRA | 55 (44.0) | 33 (44.0) | 11 (52.4) | 11 (37.9) | 0.60 |
| Loop diuretics | 108 (86.4) | 66 (88.0) | 17 (81.0) | 25 (86.2) | 0.71 |
| Echocardiography | |||||
| LVEF, % | 59.3±6.2 | 58.7±5.4 | 60.9±7.0 | 59.8±7.2 | 0.32 |
| LV end-diastolic volume index, ml/m2 | 50.3±17.7 | 49.6±17.4 | 46.7±17.9 | 55.1±18.1 | 0.23 |
| LV end-systolic volume index, ml/m2 | 20.3±8.2 | 20.6±8.0 | 17.9±8.3 | 21.6±8.7 | 0.30 |
| LA volume index, ml/m2 | 57.4 (48.2-78.7) | 54.9 (44.9-69.2) | 57.6 (52.3-84.8) | 67.1 (54.3-117.1) | 0.017 |
| EROA, mm2 | 33 (30-44) | 34 (28-40) | 30 (29-40) | 35 (30-40) | 0.60 |
| Regurgitant volume, ml | 45.0 (35.5-60.5) | 42.5 (32.5-55.0) | 50.0 (42.0-64.0) | 45.0 (42.0-62.0) | 0.32 |
| MPG, mmHg | 1.7 (1.3-2.6) | 1.6 (1.1-2.4) | 1.6 (1.4-3.0) | 1.9 (1.6-3.1) | 0.069 |
| Mitral annulus diameter, cm | 3.8 (3.5-4.3) | 3.7 (3.5-4.1) | 3.8 (3.5-4.2) | 4.0 (3.6-4.2) | 0.24 |
| sPAP, mmHg | 44.4±18.7 | 45.5±18.1 | 48.5±21.6 | 38.9±17.1 | 0.16 |
| TAPSE, mm | 19.1±4.9 | 19.8±4.7 | 17.9±4.7 | 18.5±5.5 | 0.24 |
| TR ≥severe | 60 (48.0) | 37 (49.3) | 10 (47.6) | 13 (44.8) | 0.92 |
| Values are expressed as number (%), mean±SD, or median (interquartile range). AFMR: atrial functional mitral regurgitation; BMI: body mass index; CABG: coronary artery bypass graft; COPD: chronic obstructive pulmonary disease; CRT: cardiac resynchronised therapy; eGFR: estimated glomerular filtration rate; EROA: effective regurgitant orifice area; EuroSCORE: European System for Cardiac Operative Risk Evaluation; ICD: implantable cardiac defibrillator; LA: left atrial; LV: left ventricular; LVEF: left ventricular ejection fraction; MPG: mitral valve pressure gradient; MR: mitral regurgitation; MRA: mineralocorticoid receptor antagonist; NT-proBNP: N-terminal pro-B-type natriuretic peptide; NYHA: New York Heart Association; PCI: percutaneous coronary intervention; RAS: renin-angiotensin system; SD: standard deviation; sPAP: systolic pulmonary artery pressure; TAPSE: tricuspid annular plane systolic excursion; TR: tricuspid regurgitation | |||||
PROCEDURAL OUTCOMES
The TEER procedures in patients with AFMR were mostly performed using the MitraClip system (92.0%), followed by the PASCAL system (8.0%) (Table 2). The mean number of implanted clips was 1.4±0.8, and the median procedural time was 80 minutes (IQR: 49-99 minutes). No surgical conversion was required. The procedural data for patients with VFMR is shown in Supplementary Table 2.
The echocardiographic assessment at discharge showed that, in patients with AFMR, residual MR ≤1+ was achieved in 96 of 125 patients (76.8%), while an MPG ≥5 mmHg was observed in 27 patients (21.6%). Residual MR ≤1+ with an MPG <5 mmHg was achieved in 75 patients (60.0%) (Figure 1). Residual MR ≤1+ with an MPG ≥5 mmHg was observed in 21 patients (16.7%), while residual MR >1+ was recorded in 29 patients (23.2%).
The rate of residual MR ≤1+ was comparable between patients with AFMR and those with VFMR (76.8% vs 72.2%; p=0.27), while an MPG ≥5 mmHg was more frequent in patients with AFMR than in those with VFMR (21.6% vs 13.3%; p=0.030).
Baseline clinical and echocardiographic characteristics of patients with AFMR, grouped according to the procedural results of TEER, are shown in Table 1. Patients with residual MR ≤1+ and an MPG <5 mmHg had a smaller LA volume index, compared to those with residual MR >1+ or residual MR ≤1+ and an MPG ≥5 mmHg (54.9 ml/m2 [IQR: 44.9-69.2 ml/m2] vs 67.1 ml/m2 [IQR: 54.3-117.1 ml/m2] vs 57.6 ml/m2 [IQR: 2.3-84.8 ml/m2]; p=0.017). In contrast, the severity of MR was comparable between the three groups.
The clinical and echocardiographic characteristics of patients with VFMR, grouped according to procedural results, are shown in Supplementary Table 3.
Table 2. Procedural data and echocardiography at discharge in patients with AFMR.
| Residual MR ≤1+ | |||||
|---|---|---|---|---|---|
| Totaln=125 | MPG <5 mmHgn=75 | MPG ≥5 mmHgn=21 | Residual MR >1+n=29 | p-value | |
| Procedural data | |||||
| Device type | 0.41 | ||||
| MitraClip | 115 (92.0) | 70 (93.3) | 20 (95.2) | 25 (86.2) | |
| PASCAL | 10 (8.0) | 5 (6.7) | 1 (4.8) | 4 (13.8) | |
| Number of clips | 1.4±0.8 | 1.3±0.6 | 1.9±0.7 | 1.3±1.1 | 0.021 |
| Procedural time, min | 80 (49-99) | 64 (43-94) | 90 (52-109) | 90 (80-114) | 0.002 |
| Echocardiography at discharge | |||||
| MR severity | <0.001 | ||||
| 0+ | 15 (12.0) | 13 (17.3) | 2 (9.5) | 0 (0.0) | |
| 1+ | 81 (65.6) | 62 (82.7) | 19 (90.5) | 0 (0.0) | |
| 2+ | 19 (14.4) | 0 (0.0) | 0 (0.0) | 19 (65.5) | |
| 3+ | 4 (3.2) | 0 (0.0) | 0 (0.0) | 4 (13.8) | |
| 4+ | 6 (4.8) | 0 (0.0) | 0 (0.0) | 6 (20.7) | |
| MPG, mmHg | 4.0±1.6 | 3.4±1.0 | 6.4±1.0 | 4.0±1.8 | <0.001 |
| Values are expressed as number (%), mean±SD, or median (interquartile range). AFMR: atrial functional mitral regurgitation; MPG: mitral valve pressure gradient; MR: mitral regurgitation; SD: standard deviation | |||||
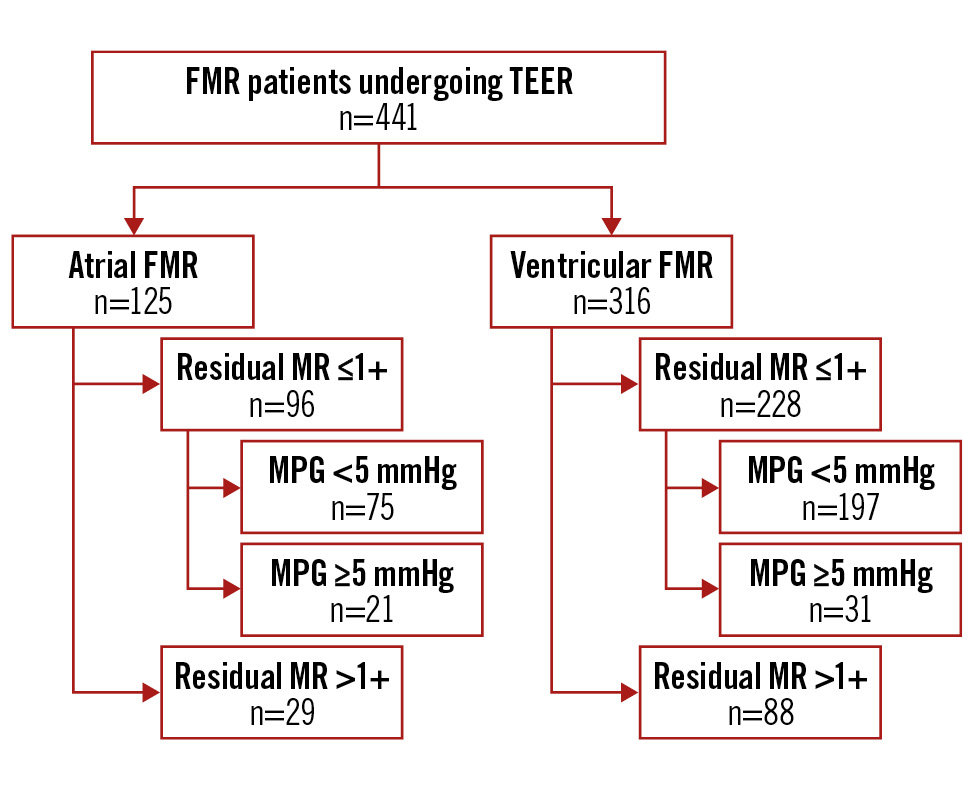
Figure 1. Study flowchart. FMR: functional mitral regurgitation; MR: mitral regurgitation; MPG: mitral valve pressure gradient; TEER: transcatheter edge-to-edge repair
CLINICAL OUTCOMES
The median follow-up was 422 days (IQR: 173-863 days). Within one year, the composite outcome had occurred in 31 of 125 patients with AFMR. In patients with AFMR, residual MR (p=0.025) with an MPG ≥5 mmHg was associated with a higher risk of the composite outcome (HR 2.31, 95% CI: 1.11-4.83; p=0.025) (Figure 2, Supplementary Table 4). In patients with VFMR, a residual MR ≤1+ was also associated with a lower risk of the composite outcome (HR 0.56, 95% CI: 0.35-0.88; p=0.012); on the other hand, the association between an MPG ≥5 mmHg and the composite outcome was not significant for these patients (HR 0.83, 95% CI: 0.41-1.66; p=0.60) (Figure 2, Supplementary Table 4).
The spline curves showed a non-linear association between an MPG and its hazard rate for the composite outcome in patients with AFMR (Figure 3), and the risk of the composite outcome increased with an MPG of >5 mmHg. In contrast, no significant relationship between the MPG and the composite outcome was observed in patients with VFMR.
AFMR patients with residual MR ≤1+ and an MPG ≥5 mmHg, as well as those with residual MR >1+, had a higher incidence of the composite outcome than those with residual MR ≤1+ and an MPG <5 mmHg (50.7%, 41.8%, and 14.3%, respectively; p<0.001) (Figure 4). In the Cox proportional hazard analysis, residual MR ≤1+ with an MPG ≥5 mmHg, as well as residual MR >1+, was associated with a higher risk of the composite outcome than residual MR ≤1+ with an MPG <5 mmHg (HR 4.37, 95% CI: 1.82-10.51; p=0.001; and HR 3.55, 95% CI: 1.51-8.36; p=0.004, respectively) (Table 3). This association was consistent in the multivariable models.
In contrast, in patients with VFMR, the risk of the composite outcome was comparable between those with residual MR ≤1+ and an MPG ≥5 mmHg and those with residual MR ≤1+ and an MPG <5 mmHg (Figure 4, Table 3).
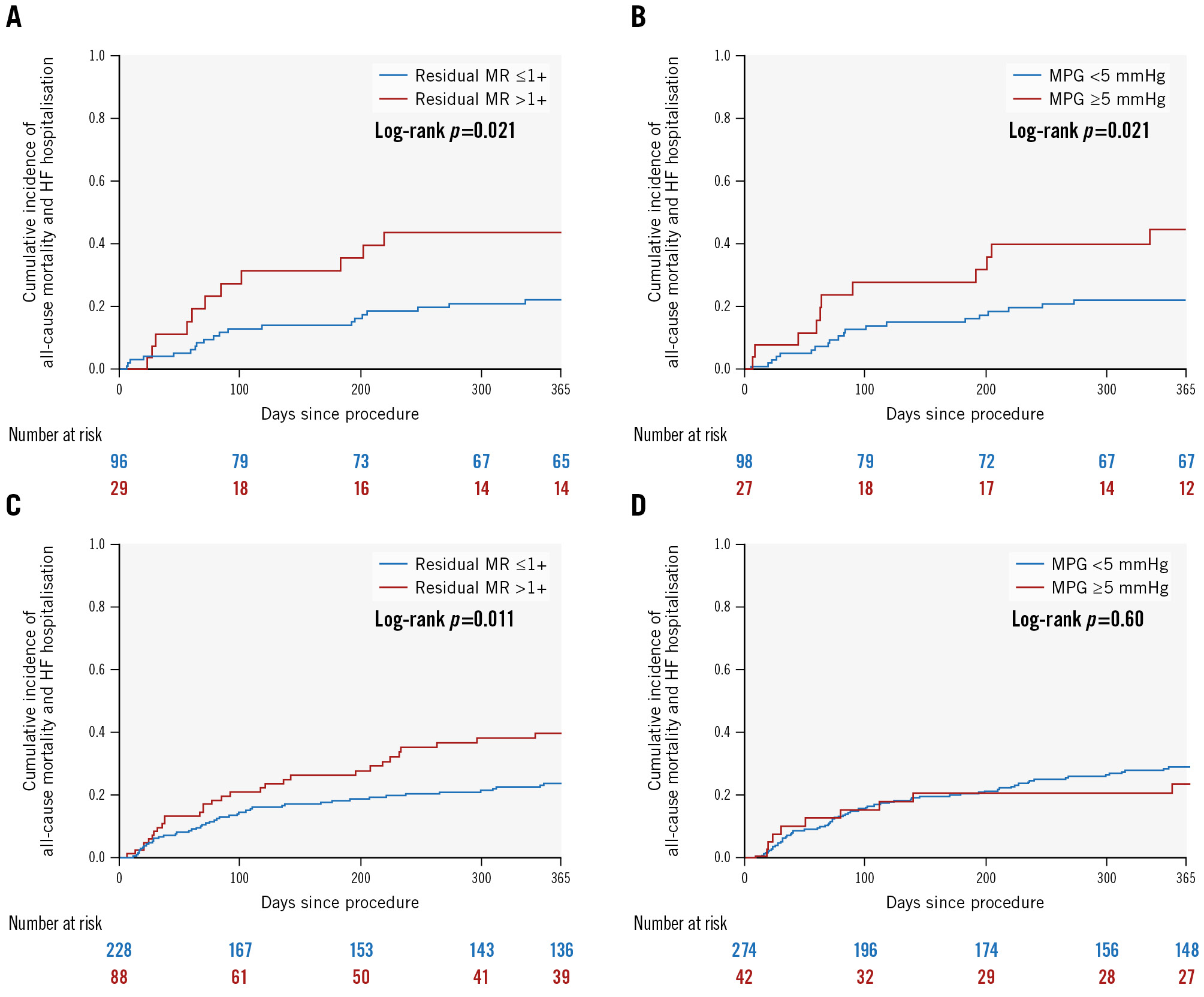
Figure 2. Association of residual MR and MPG with the composite outcome according to FMR aetiology. Incidence of the composite outcome according to residual mitral regurgitation (MR) and mean mitral valve pressure gradient (MPG) in patients with atrial functional MR (A, B) and ventricular functional MR (C, D). FMR: functional mitral regurgitation; HF: heart failure
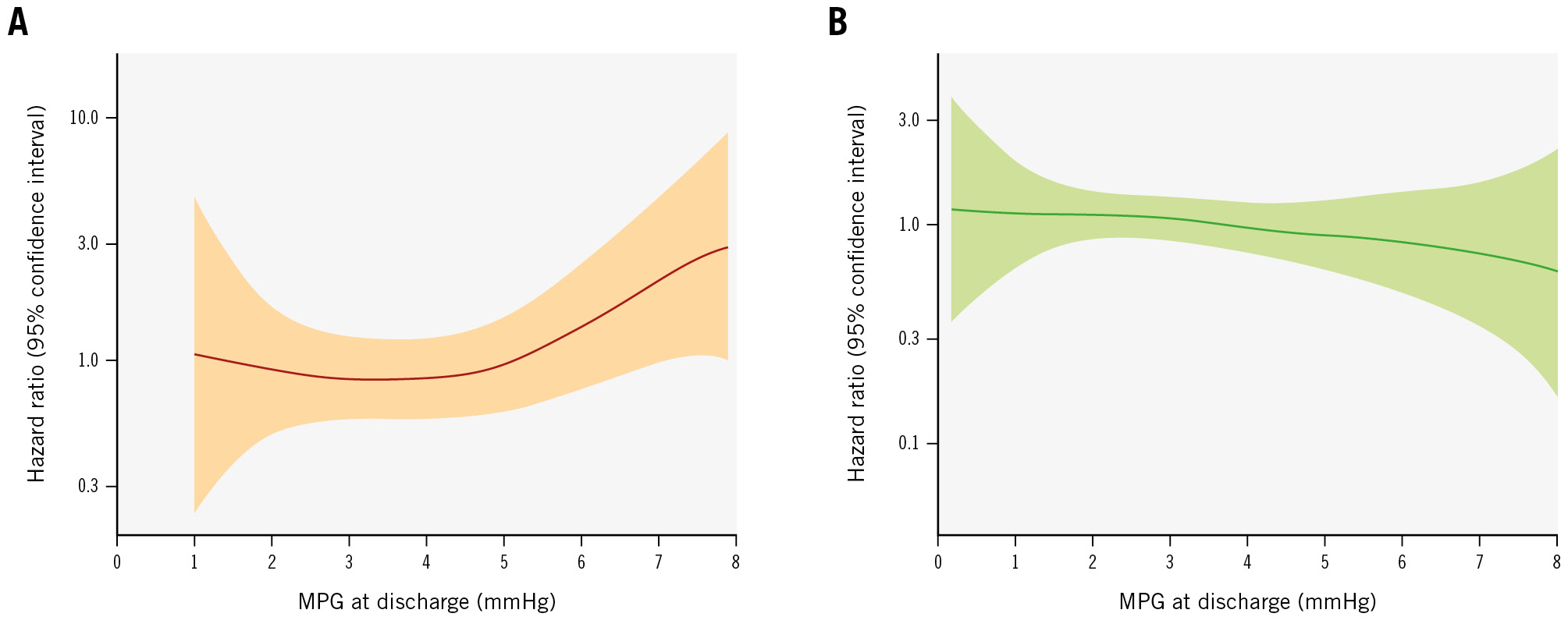
Figure 3. Spline curves for the hazard ratio of MPG in patients with AFMR and VFMR. Spline curves for the relationship between MPG at discharge and its hazard risk are shown in patients with AFMR (A) and VFMR (B). AFMR: atrial functional mitral regurgitation; MPG: mean mitral valve pressure gradient; VFMR: ventricular functional mitral regurgitation
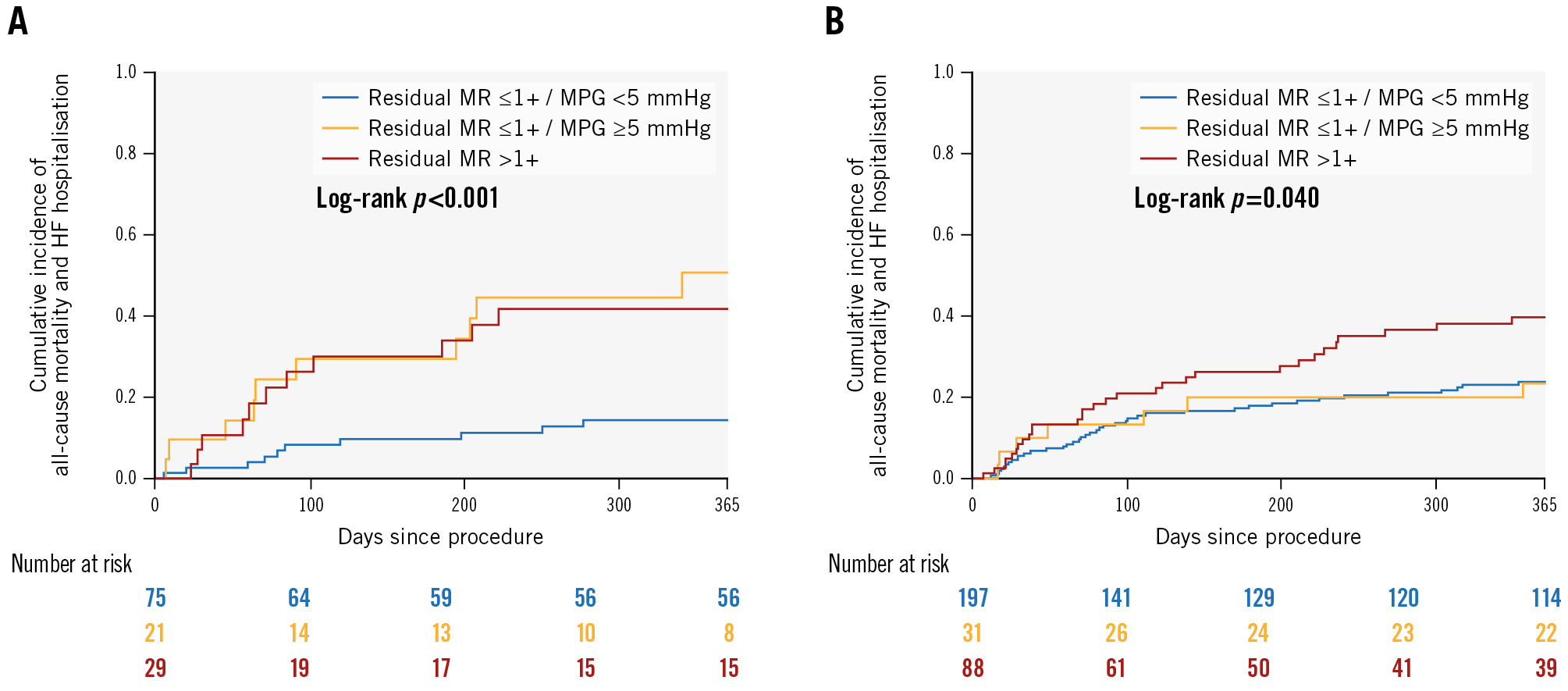
Figure 4. Association of procedural results with the composite outcome in patients with AFMR and VFMR. Incidence of the composite outcome according to residual mitral regurgitation (MR) and mean mitral valve pressure gradient (MPG) in patients with atrial functional mitral regurgitation (AFMR) (A) and ventricular functional mitral regurgitation (VFMR) (B). HF: heart failure
Table 3. Association of procedural results with the composite outcome.
| Univariate analysis | Multivariable analysis: model 1 | Multivariable analysis: model 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-value | HR | 95% CI | p-value | HR | 95% CI | p-value | |
| AFMR | |||||||||
| Residual MR ≤1+ and MPG <5 mmHg | 1 (reference) | 1 (reference) | 1 (reference) | ||||||
| Residual MR ≤1+ and MPG ≥5 mmHg | 4.37 | 1.82-10.51 | 0.001 | 4.37 | 1.79-10.66 | 0.001 | 5.11 | 2.07-12.58 | <0.001 |
| Residual MR >1+ | 3.55 | 1.51-8.36 | 0.004 | 3.36 | 1.41-8.00 | 0.006 | 4.00 | 1.64-9.74 | 0.002 |
| VFMR | |||||||||
| Residual MR ≤1+ and MPG <5 mmHg | 1 (reference) | 1 (reference) | 1 (reference) | ||||||
| Residual MR ≤1+ and MPG ≥5 mmHg | 1.01 | 0.45-2.25 | 0.99 | 1.12 | 0.50-2.51 | 0.79 | 1.09 | 0.45-2.63 | 0.84 |
| Residual MR >1+ | 1.80 | 1.12-2.89 | 0.015 | 1.98 | 1.23-3.20 | 0.005 | 1.75 | 1.03-2.99 | 0.039 |
| Multivariable model 1 included age, male sex, atrial fibrillation, and eGFR. Model 2 included LVEF, LA volume index, sPAP, and TR severity. AFMR: atrial functional mitral regurgitation; CI: confidence interval; eGFR: estimated glomerular filtration rate; HR: hazard ratio; LA: left atrial; LVEF: left ventricular ejection fraction; MPG: mean mitral valve pressure gradient; MR: mitral regurgitation; sPAP: systolic pulmonary artery pressure; TR: tricuspid regurgitation; VFMR: ventricular functional mitral regurgitation | |||||||||
NYHA FUNCTIONAL CLASS AT FOLLOW-UP
Data for the NYHA Functional Class were available at the last follow-up in 90 of 125 patients with AFMR (Supplementary Figure 1). Patients with residual MR <1+ and an MPG ≥5 mmHg were more likely to have severe symptoms (i.e., NYHA Class III or IV) at follow-up, compared to those with residual MR <1+ and an MPG <5 mmHg (58.8% vs 31.6%; p=0.042), although an improvement in NYHA Functional Class between baseline and follow-up was also observed in patients with a residual MR <1+ and an MPG ≥5 mmHg (Central illustration).

Central illustration. Association of residual MR and MPG with clinical outcome after TEER according to functional MR aetiology. Residual MR >1+ was associated with a higher incidence of the one-year composite outcome, consisting of all-cause mortality and hospitalisation due to heart failure, in both atrial and ventricular functional MR. In patients with atrial functional MR, residual MR ≤1+ with an MPG ≥5 mmHg also resulted in a higher risk of the composite outcome. HF: heart failure; MPG: mean mitral valve pressure gradient; MR: mitral regurgitation; TEER: transcatheter edge-to-edge repair
Discussion
In the present study, we investigated the association between residual MR, MPG and clinical outcomes after TEER in patients with AFMR. The main findings of the present study are as follows:
1. Residual MR ≤1+ at discharge was associated with a lower risk of the composite outcome in both patients with AFMR and those with VFMR. In contrast, an MPG ≥5 mmHg at discharge was associated with a higher risk of the composite outcome in AFMR but not in VFMR patients.
2. In patients with AFMR, residual MR ≤1+ with an MPG ≥5 mmHg, as well as residual MR >1+, was associated with a higher risk of the composite outcome than residual MR ≤1+ with an MPG <5 mmHg.
3. Patients with AFMR who had residual MR ≤1+ with an MPG ≥5 mmHg showed less postprocedural improvement in terms of NYHA Functional Class than those with residual MR ≤1+ and an MPG <5 mmHg.
AFMR has become a topic of growing interest in the field of FMR. Although ventricular aetiology was traditionally recognised as the mechanism of FMR, recent studies have explored the unique pathophysiology of AFMR and revealed its prevalence, clinical demographics, and prognosis23. Given the differences in underlying cardiac function and geometry, optimal therapeutic management may differ between VFMR and AFMR patients. While TEER is an established treatment option for VFMR, evidence of the prognostic benefits of TEER in patients with AFMR is still lacking.
In the present study, we identified patients with AFMR from a database of subjects who underwent TEER. Based on current expert opinion17, we defined AFMR as a subtype of FMR that fulfils the following criteria: preserved LV ejection fraction, normal or mildly enlarged LV volume, absence of abnormal LV wall motion, and moderate or severe LA enlargement. As a result, approximately a quarter of patients with FMR were considered to have AFMR. Patients with AFMR were older and were more likely to be female and to have atrial fibrillation than those with VFMR. In addition, patients with AFMR had greater mitral annular dilation and had severe or more TR more frequently than those with VFMR. These findings were consistent with the characteristics of patients with AFMR from previous studies4810.
In patients with AFMR, residual MR ≤1+ at discharge was achieved in 77.6% of patients, while an MPG ≥5 mmHg at discharge was observed in 21.6%. The rate of residual MR ≤1+ at discharge was comparable between patients with AFMR and VFMR, which was in line with previous studies8910. In contrast, an MPG ≥5 mmHg was more frequent in patients with AFMR than in those with VFMR. This difference might be attributable to distinct anatomical and functional features of the mitral valve in patients with AFMR17. In addition, due to patients being older, degenerative changes in the mitral annulus might be greater in patients with AFMR than in those with VFMR, affecting postprocedural changes in the MPG after TEER.
The present analysis showed that residual MR ≤1+ was associated with a lower risk of the composite outcome in patients with AFMR. This association was consistent after adjusting for baseline clinical and echocardiographic characteristics. Previous observational studies showed that mitral valve surgery may improve the prognosis of patients with AFMR compared to conservative therapy22. Our finding further infers that TEER is a safe and effective therapeutic option to reduce MR to ≤1+ and that MR reduction by TEER may lead to a better prognosis for patients with AFMR, as shown in patients with degenerate MR or VFMR1123.
While there is growing evidence regarding the prognostic benefits of MR reduction by TEER, the association between the postprocedural MPG and clinical outcomes remains a subject of debate. Recent studies suggest that the association between the MPG and clinical outcomes after TEER can vary based on MR aetiology: an elevated MPG may have less impact on the prognosis of patients with FMR, as compared to that of patients with degenerative MR11121314. We added to prior evidence by showing the association between an elevated MPG and a higher risk of the composite outcome in patients with AFMR, but not in those with VFMR. The relationship between the MPG, as a continuous variable, and the composite outcome in patients with AFMR was confirmed by our spline curve. The effect of an elevated MPG on prognosis may be more pronounced in patients with AFMR.
The negative impact of an elevated MPG on the prognosis of patients with AFMR may go beyond the benefit of MR reduction by TEER. In the present study, residual MR ≤1+ with an MPG ≥5 mmHg was associated with a higher risk of the composite outcome than residual MR ≤1+ with an MPG <5 mmHg. Moreover, there was less postprocedural improvement in NYHA Functional Class in patients with an elevated MPG, regardless of an MR reduction to ≤1+. These findings raise the possibility that the benefits of MR reduction by TEER may be attenuated by an elevated MPG in patients with AFMR. Further studies are needed to validate our findings.
The potential explanations for the prognostic impact of an elevated MPG in patients with AFMR may be multifactorial. Patients with AFMR are characterised by advanced LA remodelling and atrial arrhythmia. An elevated MPG, indicating an increase in LA afterload, might be more critical for the advanced remodelled LA that exhibits severe enlargement or dysfunction. Moreover, concomitant atrial fibrillation could enhance LA vulnerability to an elevated MPG. Nevertheless, the association between an elevated MPG and the composite outcome in patients with AFMR was consistent, even after adjusting for LA volume and atrial fibrillation. Our results are hypothesis-generating, and further investigation is needed into the different effects of an elevated MPG on the prognosis of patients with AFMR, compared to its effects on the prognosis of those with VFMR.
Given the prognostic impact of an elevated MPG, the therapeutic strategy that achieves optimal MR reduction without an elevated MPG may be essential to ensure the benefits of MR reduction in patients with AFMR. Appropriate patient selection based on the anatomical features of the mitral valve may improve the procedural results of TEER for patients with AFMR. Further studies are needed to identify the anatomical predictors of an elevated MPG after TEER in patients with AFMR. Device selection during transcatheter mitral valve intervention may also be important. The PASCAL system is a TEER device characterised by a central spacer and nitinol construction24. These features of the PASCAL system may enable optimal MR reduction while minimising the stress on the mitral leaflets and annulus, thereby preventing the risk of mitral stenosis25. Furthermore, alternative transcatheter techniques are potential therapeutic options for patients with AFMR. Direct annuloplasty is reported to be unlikely to increase the MPG, unlike TEER26, and transcatheter replacement techniques may result in a greater reduction of MR without generating relevant mitral stenosis, compared to with TEER27. Thus, patient and device selection for transcatheter mitral valve intervention may need to be discussed in light of the patient’s FMR phenotype.
Limitations
Several limitations should be acknowledged when interpreting the results of this study. First, the retrospective design introduces inherent biases associated with patient selection. Despite the multivariable adjustment for potential confounders, other unmeasured confounders could influence our results. Second, there is no established definition of AFMR so far, and our echocardiographic assessments were not adjudicated by an external core laboratory. Nevertheless, we defined AFMR based on the current expert opinion17, and the characteristics of patients with AFMR were in line with previous reports4810. Third, this study included TEER procedures performed from 2010 to 2022. During these years, there were many developments in TEER devices and techniques, and in terms of how patients with FMR were managed, which might affect our results. Fourth, we evaluated the MPG using echocardiography at discharge and defined a relevant mitral stenosis as an MPG >5 mmHg, according to the MVARC criteria21. MPG is flow dependent and can vary depending on the heart rate, loading conditions, and cardiac output at the time of measurements. In addition, the MPG may vary between the end of TEER procedures and the time of discharge12. Therefore, mitral valve orifice area or MPG, indexed by heart rate and cardiac output, might precisely evaluate postprocedural mitral stenosis28. However, the MPG acts as a reasonable surrogate for the mitral valve orifice area29, and the cutoff MPG value, indexed by heart rate and cardiac output, has not yet been established for patients undergoing TEER. Furthermore, our spline curve showed that the risk of the composite outcome increased with an MPG ≥5 mmHg in patients with AFMR, which confirms the robustness of the applied cutoff MPG value. Fifth, we could not assess left atrial pressure during the TEER procedure. Changes in left atrial pressure after TEER might be valuable in evaluating the haemodynamic effects of MR reduction and an elevated MPG. Finally, we could not assess the durability of MR reduction and the changes in MPG at follow-up.
Conclusions
An MR reduction to ≤1+ by TEER was associated with a lower risk of clinical outcomes in patients with AFMR, while an elevated MPG was linked to an increased risk of clinical outcomes. An optimal MR reduction by TEER may have potential benefits on the prognosis of patients with AFMR, although the prognostic benefit of MR reduction may be attenuated by an elevated MPG.
Impact on daily practice
Transcatheter edge-to-edge repair (TEER) is safe and effective in reducing mitral regurgitation (MR) in patients with atrial functional MR (AFMR). In the present study, an MR reduction to ≤1+ following TEER was associated with a better prognosis in patients with AFMR; however, the prognostic benefit of MR reduction was attenuated by an elevated mean mitral valve pressure gradient (MPG). Optimal MR reduction following TEER may improve the prognosis of patients with AFMR, although the prognostic benefit of MR reduction may be attenuated by an elevated MPG.
Funding
This research did not receive any grants from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest statement
T. Tanaka has been financially supported in part by a Fellowship from the Japanese College of Cardiology and the Uehara Memorial Foundation; he has also received honoraria from Canon Medical Systems. A. Sugiura has received honoraria for lectures from Edwards Lifesciences. G. Nickenig has received research funding from the Deutsche Forschungsgemeinschaft, the German Federal Ministry of Education and Research, the EU, Abbott, Edwards Lifesciences, Medtronic, and St Jude Medical; he has also received honoraria for lectures or advisory boards from Abbott, Edwards Lifesciences, Medtronic, and St Jude Medical. M. Weber has received lecture or proctoring fees from Abbott and Edwards Lifesciences. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.