Abstract
Aims: Compare mid-term outcomes after MitraClip® implantation for severe mitral regurgitation (MR) in patients categorised in different logistic EuroSCORE (LES) groups.
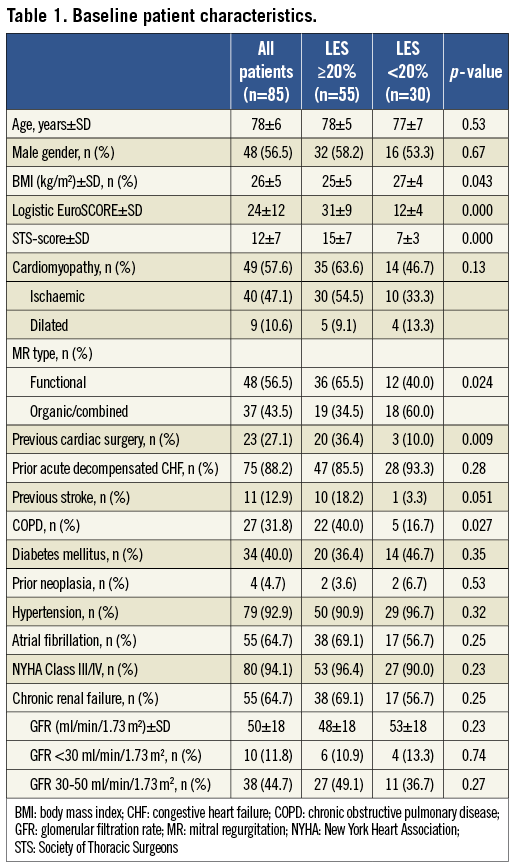
Methods and results: MitraClip was implanted in 85 patients (78±6 years, 48 men [56.5%]) with severe symptomatic MR. Baseline characteristics, perioperative results, mid-term survival, major adverse cerebrovascular and cardiac events (MACCE), and re-hospitalisation were compared in patients with LES <20% (n=30) and ≥20% (n=55). Overall LES was 24±12 (range 2.5-56.3) and STS-score 12±7 (range 1.2-31.2). Overall procedural success rate was 96.5% with an in-hospital mortality rate of 3.5%. Echocardiographic and clinical follow-up confirmed similar mean transmitral pressure gradient (p=0.13), MR degree (p=0.48), and NYHA Class (p=0.93). Estimated six-month survival and freedom from composite endpoint was 80.7%/77.1% in LES ≥ 20% and 90.8/86.6% in LES<20% group, respectively (p= 0.014; p=0.018). Multivariate analysis determined LES ≥20% (OR=8.1; 95% CI 1.002-65.186), mean transmitral gradient after intervention (OR 2.5; 95% CI 1.267-5.131) and residual MR (OR=5.1; 95% CI 1.464-17.946) as predictors for overall mortality.
Conclusions: LES is a good predictor of perioperative results, and follow-up adverse outcomes after MitraClip implantation are significantly influenced by the preoperative risk profile. The presence of residual MR immediately after MitraClip therapy can exacerbate the occurrence of MACCE.
Introduction
Percutaneous implantation of MitraClip® (Abbott Vascular, Santa Clara, CA, USA) has recently been popularised to treat patients with symptomatic severe mitral regurgitation (MR)1,2. The procedure mimics the “edge-to-edge” surgical technique developed by Alfieri et al in the early 1990s3. Although the technique is very promising, follow-up outcome may be negatively influenced by the patients’ preoperative characteristics and, in particular, by the preoperative risk profile. To date, this treatment strategy is assigned to patients rejected from conventional surgical treatment due to anatomical conditions or high comorbidity index. Risk stratification is carried out by clinical judgement in the heart team as well as by using established operative risk stratification scores like the logistic EuroSCORE (LES) and the Society of Thoracic Surgeons (STS) score. LES has been used since 1999 for scientific and clinical purposes. The modified Finnish version is recognised as one of the most reliable risk-scoring methods for prediction of immediate postoperative and late mortality, and has good predictive power4. However, in the real world its ability to predict adverse outcomes after MitraClip implantation has never been investigated. The aim of this study was to investigate early and mid-term clinical outcomes after MitraClip implantation and the impact of the preoperative comorbid profile, as represented in the LES, on mid-term clinical endpoints.
Materials and methods
STUDY DESIGN
All data concerning consecutive patients treated with MitraClip in our institution were prospectively collected in a computerised database and analysed. The indication for treatment of MR was according to current guidelines5 and was discussed in an interdisciplinary cardiology-cardiac-surgeon heart team. Surgical risk was assessed with the Finnish modified version of LES6, the STS mortality risk score7 as well as by clinical judgement. Only patients formally rejected from conventional surgery or patients refusing conventional surgery on a personal basis were treated with MitraClip. Commonly, exclusion criteria for MitraClip were terminal stage of oncologic disease with a life expectancy of less than one year, significant mitral stenosis and acute endocarditis.
PREOPERATIVE/PERIOPERATIVE EVALUATION AND TREATMENT
As part of pre-interventional screening, patients underwent echocardiography and invasive cardiac evaluation with coronary angiography, left ventriculography, and right heart catheterisation. All MitraClip procedures were performed as previously described2 in a hybrid operation theatre, under general anaesthesia, and using fluoroscopic and transoesophageal two and three-dimensional echocardiographic guidance. The MitraClip system included a MitraClip device, a 24 Fr guiding catheter, and a clip delivery system. The number of clips used was at the discretion of the primary operator and depended on the extent of residual MR. Post-interventional care was as per the standard for patients undergoing percutaneous cardiac interventions. Dual antiplatelet therapy with aspirin 100 mg and clopidogrel 75 mg was recommended for six months with aspirin monotherapy after that.
ECHOCARDIOGRAPHIC EVALUATION
The severity of MR was graded in accordance with the American Society of Echocardiography8. Grading criteria for post-procedural MR were adapted to the quantitative assessment of severity of MR in percutaneous mitral valve (MV) repair as reported by Foster and co-workers9. Measurement of left ventricular (LV) volumes and ejection fraction (LVEF) was performed according to the biplane Simpson’s method, whereas the MV orifice areas (MVOA) were assessed using planimetry (2D/3D/QULAB-Philips).
FOLLOW-UP
Clinical and echocardiography follow-up was performed at discharge as well at one, three, six and 12 months after the procedure. Data concerning reintervention, cardiac re-hospitalisation and death were collected together with information about major cardiac and cerebrovascular events (MACCE). MACCE was defined as the composite of death, myocardial infarction, emergency conversion to surgery, cerebrovascular events (haemorrhagic or ischaemic stroke), and major bleeding (fatal bleeding and/or leading to transfusion of two or more units of whole or red blood cells)10,11.
Statistical analysis
Data are presented for the overall cohort as well as for the survivors and deceased patients. Normal distribution of continuous variables was tested by means of the Shapiro-Wilk test. Differences between both groups (LES ≥ or <20%) were tested using the unpaired Student’s t-test, Mann-Whitney test, χ-square, and Fisher’s exact test whenever appropriate. Cox regression analysis was performed to identify the mid-term risk of overall mortality and composite endpoint of mortality, cardiac re-hospitalisation, reintervention, and MACCE associated with LES ≥20%. Kaplan-Meier curves were presented for overall survival, MACCE, cardiac re-hospitalisation and cumulative endpoint, and the log-rank test was used to compare the two groups. A p-value <0.05 was considered significant. Data analysis was performed with the SPSS (version 15, SPSS Inc., Chicago, IL, USA) software package.
Results
From February 2010 to December 2011, 85 patients (48 men [56.5%]) with a mean age of 78±6 years underwent a MitraClip procedure at the University Heart Center in Rostock, Germany. The overall mean LES and STS scores were 24±12 (range 2.5-56.3) and 12±7 (range 1.2-31.2), respectively (Table 1). All patients presented with grade 3+ or 4+ symptomatic MR caused by functional (n=48) and degenerative/mixed (n=37) nature. MV leaflet prolapse was present in 34 (40.0%) patients. Of these, 18 (21.2%) had anterior MV leaflet prolapse, 11 (12.9%) posterior prolapse, and 5 (5.9%) a combined prolapse. Thirty patients (35.3%) had a LES <20 but were considered for MitraClip implantation because of specific reasons not accounted for in the LES calculation (10 patients refused conventional surgical intervention, three patients had prior transcatheter aortic valve implantation (TAVI) or complex aortic valve replacement, 12 patients were frail and had severe pulmonary hypertension (PAPs >60 mm Hg) or LVEF <25%, three patients presented with oncologic/autoimmune disease, one patient had experienced two prior strokes and reported alcohol abuse, and one patient had significant chronic anaemia).
IMPACT ON ECHOCARDIOGRAPHIC PARAMETERS
At discharge, no patient had grade 4+ MR, whereas 5 (5.9 %) had grade 3+ MR. In the overall group, MVOA reduced immediately after MitraClip from 5.1±1.0 to 2.9±0.5 cm2 (p=0.001), with a corresponding increase in mean transmitral pressure gradient from 2.3±0.1 to 3.4±1.4 mmHg (p=0.001). A comparison of both groups revealed significant differences for LVEF (p=0.001), annulus diameter (p=0.004), MVOA (p=0.020), mean transmitral pressure gradient (p=0.015) and left ventricular end-systolic diameter (LVESD) (p=0.031) (Table 2), whereas the degree of MR after MitraClip implantation was equally distributed in both groups (Figure 1).
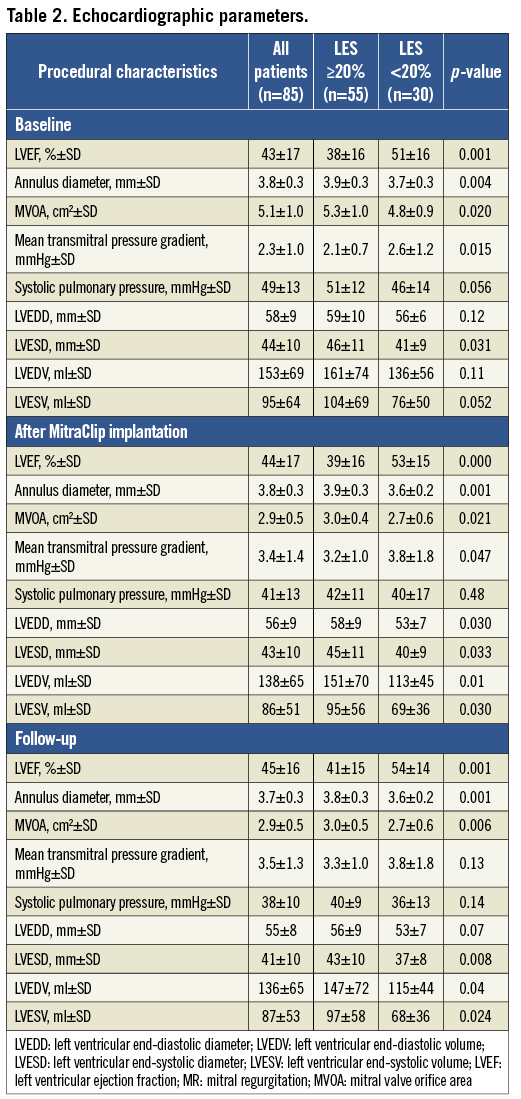
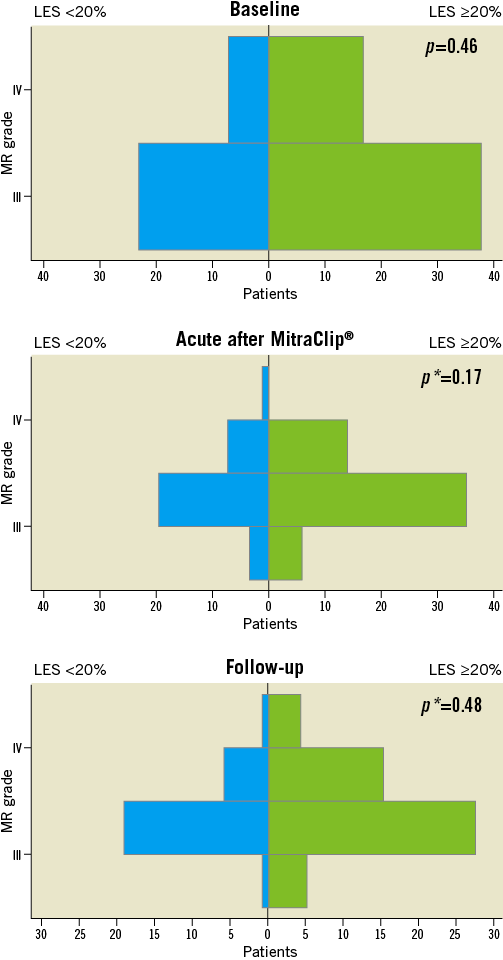
Figure 1.Mitral regurgitation at baseline, during hospital stay and during follow-up after MitraClip. LES: Logistic EuroSCORE; MR: mitral regurgitation; p*: MR grade ≤2
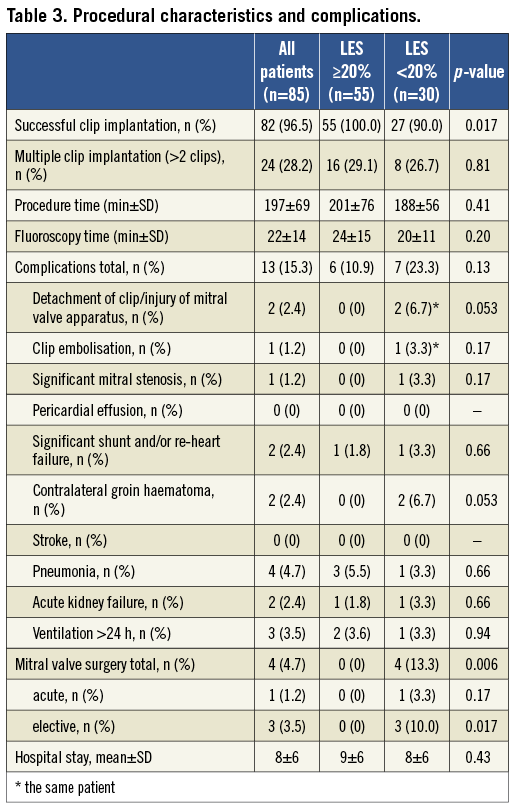
PROCEDURAL AND IN-HOSPITAL OUTCOMES
Successful clip placement was achieved in 82 patients (96.5%) with an in-hospital mortality rate of 3.5%. Median total procedure and device implantation time were 197±69 min and 22±14 min, respectively (Table 3). Procedural success was defined as the implantation of at least one clip and residual MR of grade ≤2 without new onset of significant MV stenosis. The procedure was carried out with one clip in 17.0%, two clips in 55.3%, three clips in 22.3%, four clips in 4.7%, and five clips in 1.2% of patients. Failed procedures were reported in three patients due to post-procedural significant MV stenosis, new MR grade 3 caused by partial detachment of a clip two weeks after the initial successful procedure, and because of a new significant MR due to complete clip detachment and embolism.
CLINICAL OUTCOMES
Clinical outcomes at a mean follow-up of 211±173 days (min-max 4-652, median 135) were performed in all patients who survived. Overall mortality (32.7% vs. 10.0%; p=0.020) and MACCE rate (34.5% vs. 10.0%; p=0.014) were higher in LES ≥20%, whereas congestive heart failure requiring hospitalisation (p=0.26) was not different between both groups (Table 4). Functional NYHA (New York Heart Association) Class had improved in 69 patients (81.2%), whereas no patient had NYHA Class IV (Figure 2).
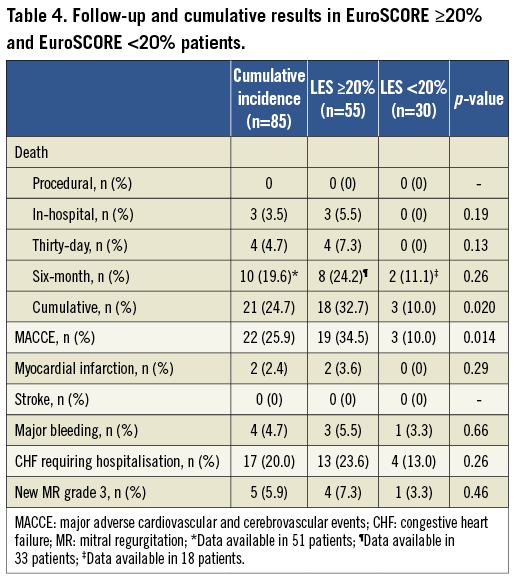
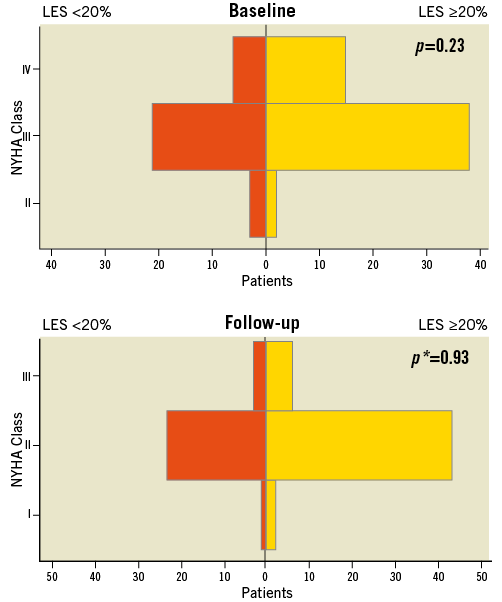
Figure 2.NYHA Class during baseline, during hospital stay and during follow-up after MitraClip. LES: logistic EuroSCORE; NYHA: New York Heart Association; p: NYHA III+IV; p*: NYHA I+II
DETERMINANTS OF FOLLOW-UP MORTALITY AND CUMULATIVE EVENTS
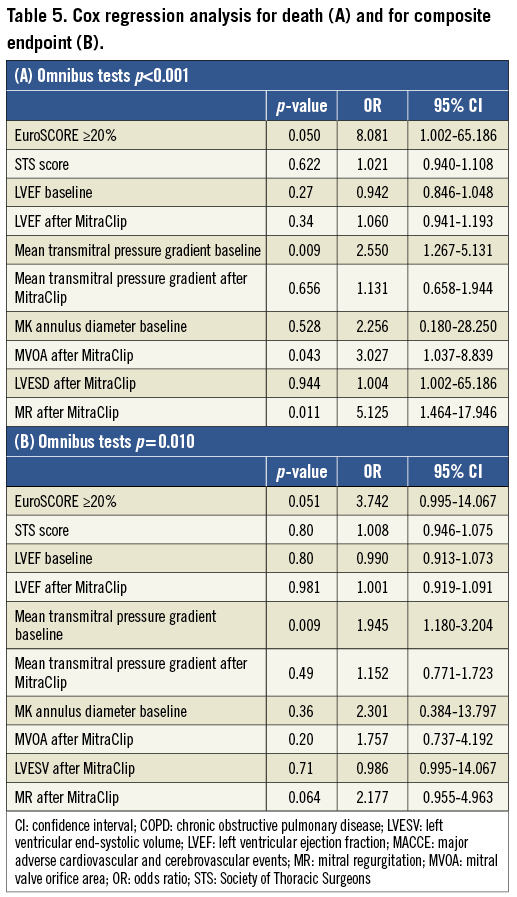
Cox regression analysis models revealed that a LES ≥20% (OR 8.1; 95% CI 1.002-65.186), mean baseline transmitral pressure gradient (OR 2.5; 95% CI 1.267-5.131), residual MR after the procedure (OR 5.1; 95% 1.464-17.946) and MVOA after the procedure (OR 3.0; 95% CI 1.037-8.839) were predictors for overall mortality (Table 5A). Predictive factors for the composite endpoint were determined in a second analysis. An association was just given for the mean transmitral pressure gradient (OR 1.9; 95% CI 1.180-3.204) (Table 5B).
Discussion
ACUTE RESULTS OF MITRACLIP THERAPY
The feasibility of MV repair using the MitraClip has already been demonstrated and is confirmed by our present data. Patients at higher risk for conventional surgery referred nowadays to MitraClip treatment present mainly with functional MR consequential to left ventricular dilatation and severe dysfunction. In experienced centres, even patients with complex comorbid profiles can be subjected to MitraClip therapy with an overall success rate of 96.5%. Nevertheless, a trend for higher thirty-day mortality is often observed in patients with higher LES. Our reported 30-day mortality rate in patients with LES ≥20% was 7.3% and is confirmed by other authors in patients with similar preoperative risk assessment12,13: it is mainly determined by the pre-existing cardiac and respiratory dysfunction. When the MitraClip therapy is applied to patients with a lower comorbidity rate, the 30-day course is almost uneventful.
MID-TERM RESULTS
In the high-risk subgroup analysis of the EVEREST II trial (STS-score 14.2±8.2) 12-month survival was 75.6% and freedom from major adverse events 57.7%, respectively14. Rudolph et al have shown, in a cohort of high-risk patients rejected from conventional MV surgery (LES 36%), a 51% one-year event-free survival rate including freedom from death, cardiac rehospitalisation and reintervention. Rehospitalisation accounted for approximately 31% and mortality for 22% of events14. More recently the same group presented, in a larger cohort of similarly complex patients, a commendable 89.6% one-year survival rate13. Equally encouraging results with a six-month survival rate of 88.5% have been proposed by Van den Branden et al in patients with LES >20%12. Our analysis shows an estimated 80.7% six-month overall survival rate and 77.1% freedom from composite endpoints (Figure 3). Rehospitalisation for exacerbation of congestive heart failure (CHF) occurred in 23.6% of these, which was significantly lower than prior intervention (85.5%). This reduction in the rehospitalisation rate is a positive achievement which, in the future, will eventually be optimised by a more holistic approach including total percutaneous MV repair (annuloplasty and MitraClip placement), resynchronisation when required, aggressive treatment of arrhythmias, and timely medical therapy and cardiac rehabilitation.

Figure 3.Freedom from rehospitalisation (A), MACCE (B), and cumulative events (C) (death, MACCE, re-hospitalisation and reintervention) curves as well as survival (D). LES: Logistic EuroSCORE; MACCE: major adverse cardiovascular and cerebrovascular events, defined as the composite of death, myocardial infarction, stroke, emergency conversion to surgery and major bleeding
RISK STRATIFICATION
The existing validated operative risk stratification indices have been proposed to guide patient selection for percutaneous treatment of heart valve pathologies16,17. It is still very controversial as to whether these indices could give a realistic prediction of the perioperative mortality and follow-up outcome. It is known that, with improvement of operative techniques and perioperative management, there might be an overestimation of perioperative mortality by these scores. Thus, a further refinement of the LES resulted in the EuroSCORE II. However, our aim was not to prove the accuracy of the LES, but to show differences in different risk categories18. Thus, we decided to use the LES for better comparison with the published data1,2. The cut-off for defining the groups was almost decided a priori and on the basis of previous experience with TAVI16,17. We revealed that the presence of a baseline LES of ≥20%, the mean transmitral pressure gradient, and residual MR after intervention were predictors for overall mortality.
MV HAEMODYNAMIC PARAMETERS AND IMPACT ON FOLLOW-UP
In our analysis patients at higher operative risk presented with enlarged MV annuli and MVOA. These findings do not seem to impact on the reparability of the valve. In fact, acute success rate is similar in both groups. On the contrary, the preoperative and immediate postoperative performance of the MV seems to have a strong impact upon follow-up mortality and composite outcome independently from the patient preoperative risk profile. In particular, baseline MV gradient is directly and strongly related to follow-up mortality. It could be argued that patients with an increase of baseline MV gradient may suffer from a further increment after MitraClip implantation. This condition may lead to further congestion in the pulmonary circulation and progressive increase of the pulmonary resistances and, in the long term, to adverse outcomes. The transmitral gradient was evaluated as a predictor for worse clinical outcome. However, the relevance of this parameter, considering the low values and impact of minimal changes on p-value, should be relativised. More important is the fact that only one of our patients presented with new mitral stenosis which could be associated with a worse outcome. This one patient underwent surgical treatment.
Moreover, the degree of residual MR and MVOA after MitraClip implantation impacts independently and negatively on follow-up survival, an association which was also known from the MV surgery19,20. This emphasises the importance of complete elimination of MR during intervention and thus underscores the need for multiple clips to improve outcomes.
Limitations
The present study represents a single-centre experience with a small sample size and limited follow-up. Thus, the resulting low event rates are difficult to deal with. Large-scale registries and randomised controlled trials are needed to define feasibility and efficacy in different subgroups. Although our aim was not to prove the accuracy of different risk scores, newer risk stratification scoring systems had to be used to determine whether a patient was a candidate for surgery or not.
Conclusion
This study confirms the feasibility of the MitraClip in high-risk patients with MR unsuitable for conventional MV surgery. Mid-term results are determined by baseline comorbidity index, expressed by LES, and by the presence of residual MR immediately after MitraClip therapy. Thus, there should be a good selection of patients which should be treated by a multidisciplinary team using different scoring systems and clinical judgement, and there should be an effort to eliminate MR at all costs to improve clinical outcomes.
Conflict of interest statement
The authors have no conflicts of interest to declare.