Abstract
The presence of mitral regurgitation (MR) in patients with heart failure represents an independent predictor of mortality. Until now, the standard therapy for severe MR has been cardiac surgery in order to perform mitral valve replacement or mitral valve repair. With the introduction of the MitraClip® system (Abbott Vascular - Structural Heart, Menlo Park, CA, USA) in 2008, there is now an alternative percutaneous treatment option available for high-risk patients. We report on an 84-year-old male patient who was admitted to the emergency room with increasing shortness of breath due to severe functional MR, at stage NYHA III. In the following days the patient developed cardiogenic shock due to failure of the diuretic medication. The case first described here demonstrates an alternative transseptal route of access via a direct atrial puncture of the RA in a patient with absent inferior vena cava. This approach was successfully used to perform a MitraClip® procedure in this patient with functional MR and cardiogenic shock. It was possible to treat mitral regurgitation and the consecutive cardiogenic shock by implanting two MitraClips®.
Introduction
The occurrence of heart failure is often associated with mitral regurgitation (MR). Following myocardial infarction, significant MR has been observed in 65% of these patients with subsequent heart failure within five years1. Within this vicious cycle, the presence of MR in patients with heart failure is an independent predictor of mortality2,3. Until now, the standard therapy for severe MR has been cardiac surgery to perform mitral valve replacement or mitral valve repair. With the introduction of the MitraClip® system (Abbott Vascular - Structural Heart, Menlo Park, CA, USA) in 2008, there is now an alternative percutaneous treatment option available for high-risk patients. Based on the “edge-to-edge” technique by Alfieri4, this involves connecting together the anterior and posterior mitral valve leaflets with a clip. Access into the left atrium is usually gained percutaneously via the femoral vein followed by transseptal puncture. The EVEREST II trial demonstrated the safety and efficacy of the MitraClip®5. As part of the High Risk Study (HRS) within the EVEREST II trial, MitraClip® was also shown to be a possible and effective treatment option in terms of clinical improvement for high-risk patients, with an estimated mortality rate ≥12%6. We are reporting on an alternative access –transatrial– when using the MitraClip® system in a patient experiencing cardiogenic shock with severe MR and lacking the inferior vena cava.
Case report
An 84-year-old male patient was admitted to the emergency room with increasing shortness of breath at stage NYHA III. Known previous cardiac illnesses were ischaemic cardiomyopathy with moderately reduced LV function, three-vessel coronary artery disease with complete surgical revascularisation (LIMA-LAD, vein M1, vein M2) in 1996 and PCI of a vein graft to M2 in 2010, as well as a previous VVI pacemaker implantation in 2009 due to bradycardia and atrial fibrillation. In addition, diabetes mellitus and arterial hypertension were also known. On admission, medication consisted of ASS, clopidogrel, ramipril, metoprolol, spironolactone, amlodipine, nitrates, phenprocuomon and insulin.
An echocardiogram showed severe functional MR due to ischaemic cardiomyopathy. NT-proBNP was 16,030 ng/l. Despite initiation of diuretic medication for decompensated heart failure, there was no clinical improvement and the patient was transferred to the intensive care unit. Correction of the MR was discussed as a further treatment option. With a log EuroSCORE of 45.3% and STS of 17.8%, a MitraClip® intervention was planned. During the procedure, an angiogram demonstrated an extensive collateralisation of the venous femoro-iliacal vessels, but an inferior vena cava could not be visualised (Figure 1). In view of the lack of a natural access route, the procedure was aborted and the patient was returned to the intensive care unit. Within 12 hours, cardiogenic shock developed with lactic acidosis requiring dual catecholamine treatment (noradrenaline, dobutamine). This was followed by renewed discussion of cardiac surgery versus alternative MitraClip® access options (transatrial, transhepatic, transjugular). The log EuroSCORE and STS rose to 62.8% and 27.7%, respectively. Due to the clinical high-risk situation, a minimally invasive approach using the MitraClip® was once again favoured. The procedure took place under general anaesthesia using transoesophageal echocardiography (TEE) and fluoroscopic guidance. Access was gained transatrially. For safety reasons, a 5 Fr catheter was inserted into the internal jugular vein and a 6 Fr catheter into the femoral artery at the beginning of the procedure to enable rapid percutaneous heart-lung machine cannulation in the event of haemodynamic instability. Access to the right atrium (RA) was now gained via a right-anterior minithoracotomy in the 8th ICS. Subsequently, a purse-string suture reinforced with a felt strip in the area of the inferior puncture site of the RA was put in place. Direct puncture of the RA and insertion of a J wire into the superior vena cava were performed and the wire was externalised via a transcutaneous subdiaphragmatical tunnelled 6 Fr catheter. Having established that specific access site, transseptal puncture with an SL1 catheter followed approximately 4.2 cm above the mitral valve annulus under TEE guidance (Figure 2). After successful transseptal puncture, a total of 10,000 I.U. heparin was administered to obtain an ACT ~250 sec. After insertion of a wire into the left superior pulmonary vein, the MitraClip® guide catheter was introduced across the intra-atrial septum into the left atrium, followed by the clip delivery system (CDS) (Figure 3). A MitraClip® was positioned centrally with good reduction of the MR. Due to a residual lateral jet, a second MitraClip® was implanted laterally to the first clip with almost complete elimination of the MR. An echocardiogram ruled out a significant mitral stenosis following implantation of two MitraClips® (dP mean 3 mmHg, MVA 1.9 cm2). The procedure was completed with a very satisfactory result. Subsequently, the CDS and the guide catheter were removed, and the RA access point was closed using the preplaced purse-string suture with a felt pledget. To conclude, insertion of a 24 Fr thoracic drain via the subdiaphragmatically tunnelled access as well as layered closure of the thorax were performed (Figure 4). The femoral artery access was closed using StarClose® (Abbott Vascular, Menlo Park, CA, USA) and the jugular vein using manual compression. The total procedure time was 160 min with a fluoroscopy time of 35 min.
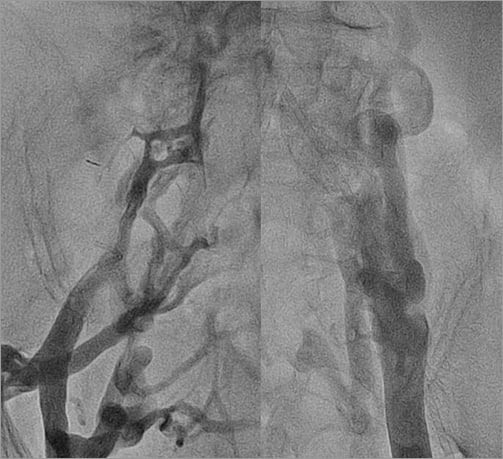
Figure 1. Angiogram of the femoro-iliacal veins.
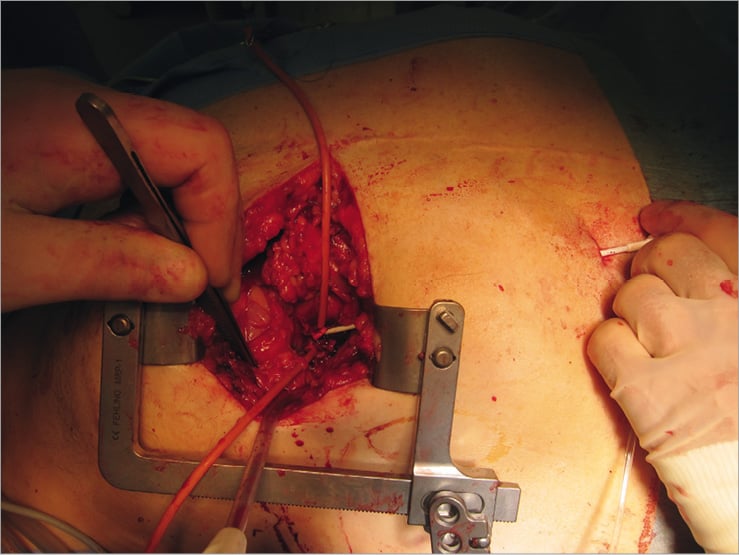
Figure 2. Right anterior thoracotomy with purse-string sutures placed at the inferio-lateral wall of the right atrium and a transcutaneous subdiaphragmatically positioned SL1 sheath into the right atrium.
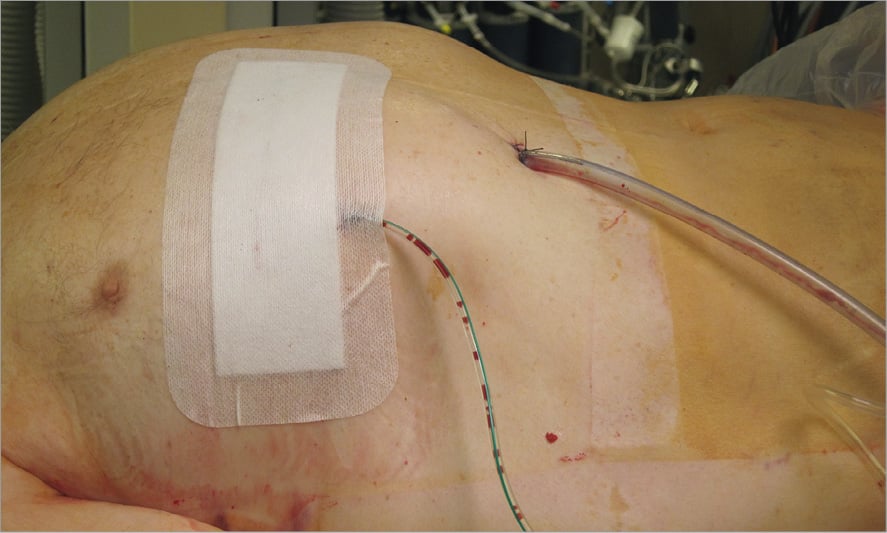
Figure 4. End of the procedure with a 24 Fr thoracic drainage and a Redon drain in place.
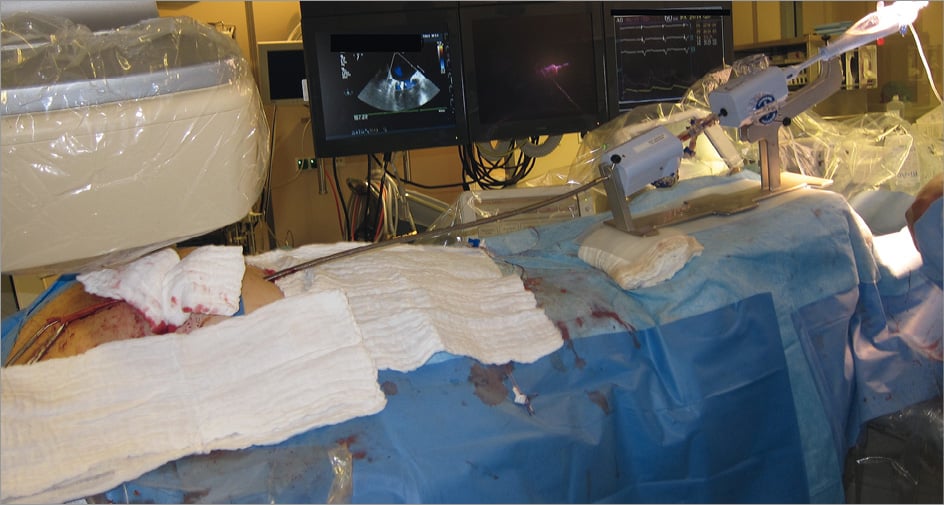
Figure 3. Clip delivery system (CDS) with guide catheter positioned into the left atrium via a direct right transatrial access.
Following the intervention, the patient was able to be weaned from ventilation and catecholamine treatment. The echocardiographic follow-up after seven days showed a very good result with only minimal remaining MR (Figure 5).
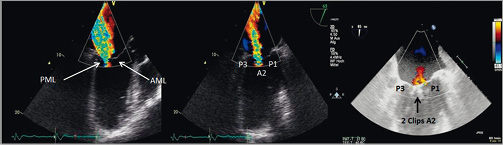
Figure 5. Transoesophageal echocardiography of the mitral valve.
A) Colour Doppler during “LVOT view” displaying the anterior mitral leaflet (AML), the posterior mitral leaflet (PML) and severe MR before clip implantation; B) intercommisural view pre-procedure with severe MR; C) intercommisural view after implantation of 2 clips in a central position resulting in mild MR.
During the last follow-up visit at three months, the functional class (NYHA II) of the patient had improved and the echocardiogram showed persistently mild MR.
Discussion
The presence of MR in patients with heart failure represents an independent predictor of mortality2,3. Current guidelines recommend the correction of MR when there are signs of heart failure7,8. However, older patients in particular frequently exhibit comorbidities such as COPD, renal failure and diabetes mellitus, and therefore represent a high-risk group for surgery2,9. A definite treatment option in these high-risk patients is the CE-certified MitraClip® approach. Various studies have demonstrated a safe and effective implantation of the MitraClip® in severe MR5,6,10,11. The case illustrated here shows a high-risk patient with a log EuroSCORE of 62.8% and STS 27.7% on the day of the procedure. In addition, the intervention took place as an emergency intervention in cardiogenic shock. The brief clinical follow-up process to date shows this to be a possible successful treatment option as an emergency intervention for a patient with cardiogenic shock due to severe mitral regurgitation. However, it is necessary to wait and see how the process continues in order to carry out a final assessment.
The particular feature of this case is the lack of the inferior vena cava. This made the standard MitraClip® procedure with transseptal puncture via the femoral vein impossible. A lack of or complete discontinuation of the inferior vena cava is rare in the general population. In a study involving 7,972 patients, there was found to be a prevalence of 0.15%12. In the literature, alternative access routes are described for a missing or thrombotic inferior vena cava for left-atrial electrophysiological ablation. Singh et al describe a transhepatic approach for two patients13. The closure of the 8 Fr access point took place in one case using bipolar radiofrequency energy and for other patients by implanting a vascular plug. Due to the relatively large access point of 24 Fr for the MitraClip®, we abandoned this access option. The transseptal puncture using the transjugular approach is often difficult due to the limited manoeuvrability of the catheter. Thus, we did not choose this access route either. In our opinion, access via an inferior direct puncture of the RA best imitates the natural route and the associated controllability of the MitraClip® system. Using a right-anterior minithoracotomy approach compared to mitral valve repair sternotomy has the advantage of minimising surgical trauma and lowering the risk of post-sternotomy wound infection. Furthermore, in this special case the patient had a LIMA graft to the LAD and therefore sternotomy was associated with a higher risk of damaging this graft. Within our Heart Team the decision was taken to avoid cardiac surgery with the need of a heart-lung machine due to a very high log EuroSCORE. In addition, a purse-string suture reinforced with a felt strip with subsequent direct puncture of the left ventricle has systematically been shown to be safe, as seen in transapical aortic valve implantation14.
Conclusion
The case described here demonstrates an alternative transseptal route of access via a direct atrial puncture of the RA in a patient lacking the inferior vena cava. This approach was successfully used to perform a MitraClip® procedure in a patient with functional MR and cardiogenic shock. It was also possible to treat mitral regurgitation and the consecutive cardiogenic shock by implanting two MitraClips®.
Conflict of interest statement
The authors have no conflicts of interest to declare.

