The MitraClip® device (Abbott Vascular, Santa Clara, CA, USA) (Figure 1) is the only available device for transcatheter mitral valve repair that can count more than 30,000 patients treated. The device consists of two movable arms and grippers to grasp the mitral valve leaflets, creating a vertical line of coaptation, forming a double-orifice valve as in Alfieri’s surgical edge-to-edge technique. The EVEREST trial and many registries based on real-world patients demonstrate the improvement of many parameters (NYHA class, mitral regurgitation [MR] grade, six-minute walking test, rehospitalisation rate, left ventricle [LV] volume and diameter). Post-procedural MR ≤2 has been achieved in a high percentage of patients (ranging from 85% to 99% in different registries) and is maintained in about 90% of patients at one-year follow-up.
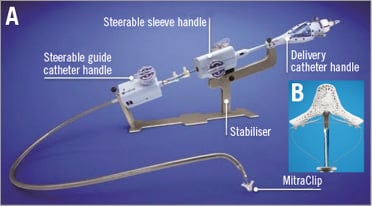
Figure 1. MitraClip system. A) MitraClip system with all its components. B) New MitraClip NT.
To achieve good results, the clinical and echographic selection of patients and the correct execution of the implant are very important.
Clinical selection
Even if the majority of patients treated with MitraClip will benefit from the treatment, it is easy to understand that the more advanced the cardiac disease the less beneficial the treatment will be. Data from many registries suggest that the ischaemic aetiology of MR, NYHA IV at baseline, left ventricular end-systolic volume >110 ml, pulmonary artery pressure >50 mmHg, chronic kidney disease, and moderate to severe tricuspid regurgitation are all independent predictors of rehospitalisation and death. However, probably the most important factor with a negative impact is an impaired right ventricle (RV) function.
Echographic selection
Transthoracic echography (TTE) 2D echo is used to assess MR severity but transoesophageal echography (TEE) is mandatory to confirm initial TTE findings. 3D TEE adds remarkable benefits in the assessment of mitral valve (MV) anatomy and is useful to achieve better procedural results.
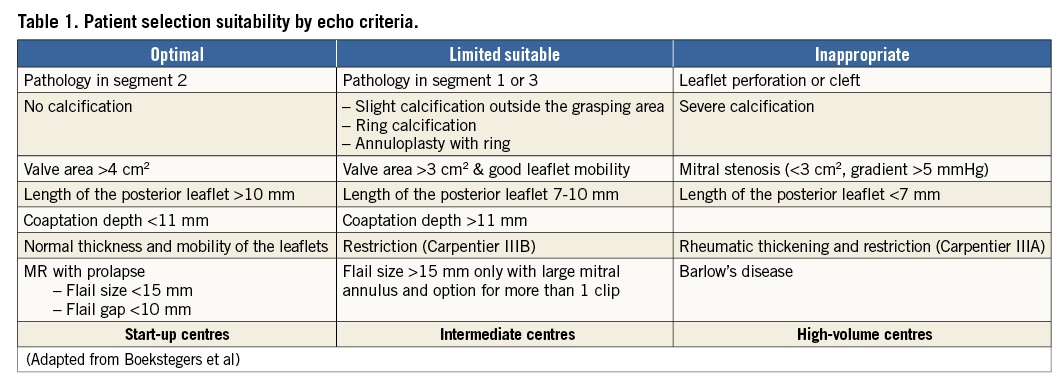
With the increasing experience of operators in managing the device in difficult anatomies, the EVEREST criteria for the selection of patients are outdated.
Modifying the classification of Boekstegers et al we can re-assign the three columns from optimal, limited suitable and inappropriate to optimal for “start-up centres”, limited suitability for “intermediate centres” and appropriate only for “high-volume centres” as in Table 1. There are still concerns regarding stenotic and rheumatic mitral valves.
Optimising procedure and results
The MitraClip procedure can be simplified by dividing it into five steps: 1) transseptal puncture, 2) straddling and steering of the clip, 3) alignment to the mitral valve and commissure line, 4) grasping, 5) final evaluation. Each step is important in order to achieve better results.
Transseptal puncture
This is one of the most important steps. It is recommended to be superior and posterior in the fossa with a height ranging from 3.5 to 4.5 cm depending on the type of disease (functional mitral regurgitation [FMR] vs. degenerative mitral regurgitation [DMR]). The site of the puncture can be modified to reach lesions located in the medial or lateral position, so it should be higher in the case of a medial lesion and lower in the case of a lateral lesion.
Straddling and steering
This is an easy step and it can be carried out using only fluoro in the majority of cases. The fastest manoeuvre is to complete the straddling pointing with the clip to the pulmonary vein and steering by going simultaneously posterior with the steerable guiding catheter (SGC) and medial with the medial/lateral (M/L) knob. An excessive use of the M-knob should be avoided to create less tension in the system.
Alignment to mitral valve and commissure line
In this step, it is crucial to have a perpendicular trajectory in the two-chamber view to avoid entanglement with the chordae by manipulating the M/L knob and/or advancing/retracting the system. In the left ventricular outflow tract (LVOT) view, the arms of the clip should be parallel to the leaflets using the ± knob. The simultaneous view resulting from an X-plane is useful to assess simultaneously in both directions. The clip must be perpendicular to the commissure line to have a simultaneous and symmetric grasping to avoid distorting the valve. The en face 3D reconstruction is very useful to reach this target, especially when the target is out of the A2-P2 scallop. In these cases, a clockwise rotation if lateral or a counterclockwise rotation if medial is required.
Grasping
Even if the scope is the same, the technique may differ in the treatment of FMR and DMR.
In the case of FMR, one central clip strategy should be attempted if the annulus is not too large. After clip implantation, check the result and the remaining jet in order to optimise the results, eventually moving the clip medially or laterally or implanting an additional clip. If the annular size is more than 35 mm, it is more likely that two clips will be implanted. In this case, the medial clip should be implanted first since it will be easier to implant a second clip laterally.
When dealing with DMR, the target of the first clip should be the lesion (flail/prolapse). Then, the use of a second clip is advised, even if significant residual MR is not present, in order to stabilise the first clip and guarantee longer durability. If necessary, more than two clips can be implanted (Figure 2).
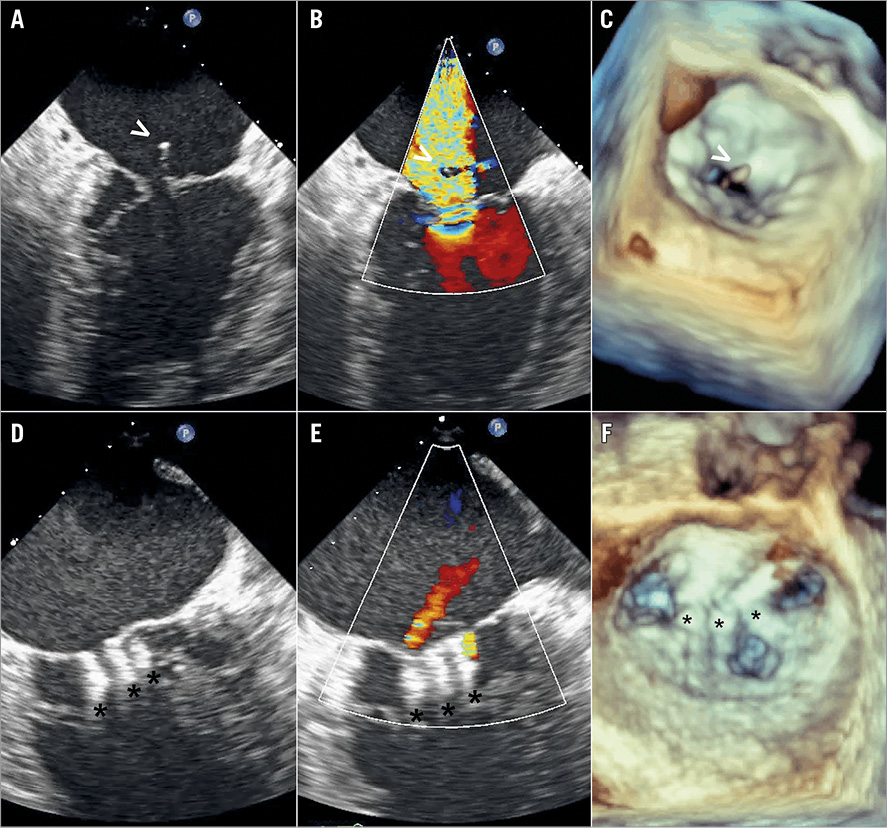
Figure 2. 2D and 3D TEE. Severe mitral regurgitation due to a ruptured chordae (white arrow, panels A, B and C); final result after implantation of three MitraClips (black asterisks, panels D, E and F); and triple orifice creation (panel F).
Evaluation
The grade of residual MR and stenosis and morphological evaluation must be carried out before and after each clip. It is important to conduct the evaluation in the same haemodynamic conditions and with the same ultrasound machine settings. There are no guidelines on the assessment of MR after the creation of a double (sometimes triple) orifice. A multimodality approach seems to be the most reasonable in order to obtain a reliable quantification of MR. In addition to echocardiography, LA pressure measurement is useful. A decrease or even a normalisation is seen in the case of effective reduction of MR. From a morphological point of view, it is important to be sure that both leaflets are grasped and inserted into the clip arms. Three-dimensional echo in diastole is useful for evaluating the geometry and size of the orifices created and the two symmetrical isosceles triangles with the base to the annulus and the apex to the clip. Distortion of the valve or excessive tension on the leaflets must be avoided.
During follow-up visits, usually at one, three, six, 12 months and yearly, TTE is performed to assess the result. The following checks are also carried out: colour flow Doppler of the MR, MV inflow gradient, assessment of pulmonary vein flow, residual atrial septal defect evaluation, systolic pulmonary artery pressure, LV and RV size and volume measurements in systole and diastole, and LVEF. In case of doubt, an additional TEE should be performed.
Conflict of interest statement
C. Grasso is a proctor for Abbott Vascular. H. Ince is a proctor for Abbott Vascular.

