Introduction
Mitral regurgitation (MR) is a common valvular abnormality with an estimated prevalence of 2.1% for a moderate to severe degree of MR in population-based studies1. If untreated, MR leads to significant morbidity and mortality resulting from left ventricular dilatation and congestive heart failure (CHF)2. Transcatheter mitral valve repair using the MitraClip (Abbott Vascular) has revolutionised the treatment of patients with symptomatic severe primary MR who are at a prohibitive risk for surgery, and for those with symptomatic moderate to severe secondary MR refractory to guideline-directed medical therapy34. Given the association of ageing with MR, as well as concern for peri-operative mortality and morbidity with open-heart surgery, a rising proportion of elderly patients are undergoing the MitraClip procedure. However, there are limited data regarding procedural outcomes following the MitraClip procedure in elderly patients, especially nonagenarians. The objective of this study was to address this knowledge gap using data from a large national database.
Methods
The National Readmissions Database (NRD; 2015-2018) was used to identify patients with MR who underwent the MitraClip procedure using the International Classification of Diseases (ICD) procedure code ICD-10: 02UG3JZ. Similarly, post-procedural complications were identified using appropriate ICD-10 codes and included: complete heart block, need for permanent pacemaker, myocardial infarction, cardiogenic shock, cardiac arrest, pericardial complications, device related complications, stroke or transient ischaemic attack, acute kidney injury requiring haemodialysis, major bleeding, vascular complications, or conversion to mitral valve surgery. The study population was categorised into three comparison groups based on age (<80 years, 80-89 years, and ≥90 years). Outcomes assessed in our study included in-hospital mortality, 30-day readmission, CHF-related readmissions, and post-procedure complications. Hospitals were categorised into low-, intermediate- and high-volume centres according to their annual volume for MitraClip implantations (<5, 5-14 and ≥15, respectively). Hospital volume was identified using “Hosp_NRD” variable provided by the NRD. Our study was deemed exempt from institutional review as the NRD is a publicly available, de-identified database. SAS 9.4 (SAS Institute Inc.) was used for statistical analyses. The chi-square test was used to compare the differences between categorical variables. A hierarchical, multivariable, logistic regression model was performed to assess the effect of age on study outcomes. P-values of <0.05 were considered significant.
Results
We identified a total of 19,284 patients, of whom 8,905 were <80 years of age, 8,708 were 80-89 years old (octogenarian) and 1,671 were ≥90 years old (nonagenarian). The nonagenarian cohort included a greater proportion of females, as compared to the octogenarian and <80 year-old cohorts. The nonagenarian cohort had a higher prevalence of patients in the highest median household income category, with hypertension, CHF, nutritional anaemia, pulmonary hypertension, chronic kidney disease, non-elective admissions, and patients discharged to a skilled nursing facility. Patients in the <80 year-old cohort had a higher prevalence of diabetes mellitus, obesity, tobacco abuse, peripheral arterial disease, chronic obstructive pulmonary disease and liver disease, while atrial fibrillation/flutter was more prevalent in octogenarians (Table 1).
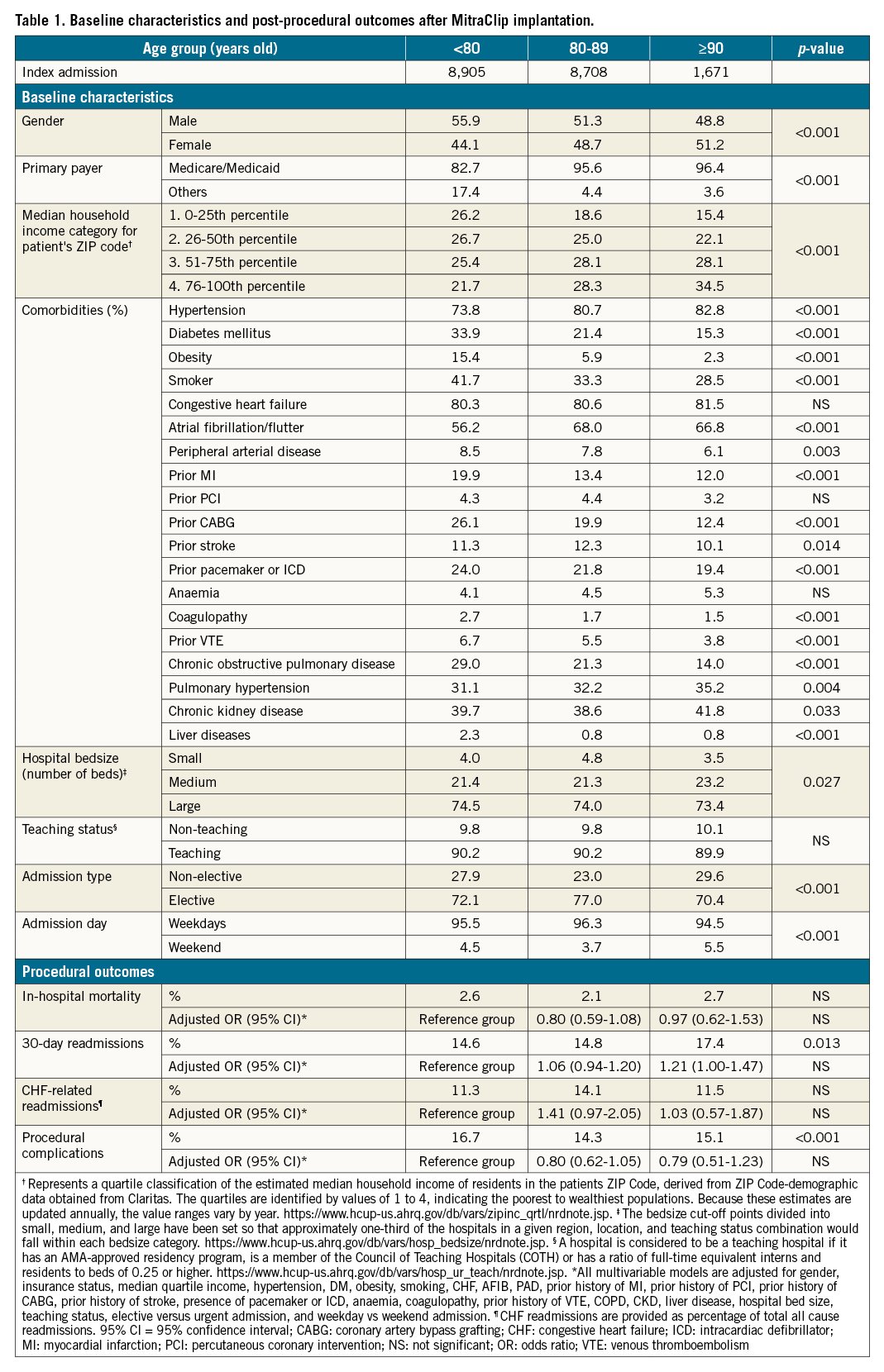
Compared to patients <80 years of age, we noted no difference in in-hospital mortality or CHF-related 30-day readmissions among nonagenarians and octogenarians on univariate or multivariable models. On univariate comparison, nonagenarians appear to have had a high all-cause 30-day readmission rate. However, this difference was not seen with multivariate analysis. Similarly, post-procedural complications did not differ among comparative cohorts with multivariate analysis (Table 1). Increased institutional experience (>5 MitraClip/year) was associated with improved survival, fewer 30-day and CHF-related readmissions and a reduction in procedural complications in elderly patients (≥80 years). In patients <80 years of age, increased institutional experience was associated with improved survival and fewer procedural complications, without any statistically significant effect on readmissions (Supplementary Table 1).
Discussion
Our findings suggest that the safety and procedural outcomes of MitraClip implantation in elderly cohorts are comparable to those in younger patients. Additionally, the mortality among elderly patients who underwent the MitraClip procedure in our study was considerably lower (2.1 % in octogenarians and 2.7% in nonagenarians), compared to mitral valve surgery in this elderly patient population, which has been reported to be as high as 14% in previous studies5. Better outcomes in the elderly cohort could be the result of better patient selection, improvement in procedural technique, and greater operator experience. The noted higher socioeconomic profile of elderly patients in our study may also be a contributing factor to better outcomes. Additionally, the better outcomes associated with centres with higher annual volumes suggests that, in addition to careful patient selection, centres with high institutional experience are pivotal in improving outcomes among very elderly patients.
Limitations
Our study has a few limitations, including the observational nature of the dataset, the lack of imaging data and the unavailability of data related to the mechanism of MR. Also, due to the limitation of the database, we could not evaluate the impact of operator volume on outcomes.
Conclusions
Many elderly patients, including nonagenarians, enjoy a good quality of life and deserve the opportunity to maintain this quality of life. Our results demonstrate that, in well-selected patients, advanced age alone should not be a limiting factor for edge-to-edge repair with the MitraClip.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.