Abstract
Aims: To evaluate the outcomes of mitral valve surgery in octogenarians with severe symptomatic mitral regurgitation (MR).
Methods and results: We performed a systematic review and meta-analysis of data on octogenarians who underwent mitral valve replacement (MVR) or mitral valve repair (MVRpr). Our search yielded 16 retrospective studies. Using Bayesian hierarchical models, we estimated the pooled proportion of 30-day mortality, postoperative stroke, and long-term survival. The pooled proportion of 30-day postoperative mortality was 13% following MVR (10 studies, 3,105 patients, 95% credible interval [CI] 9-18%), and 7% following MVRpr (six studies, 2,642 patients, 95% CI: 3-12%). Furthermore, pooled proportions of postoperative stroke were 4% (six studies, 2,945 patients, 95% CI: 3-7%) and 3% (three studies, 348 patients, 95% CI: 1-8%) for patients undergoing MVR and MVRpr, respectively. Pooled survival rates at one and five years following MVR (four studies, 250 patients) were 67% (95% CI: 50-80%) and 29% (95% CI: 16-47%), and following MVRpr (three studies, 333 patients) were 69% (95% CI: 50-83%) and 23% (95% CI: 12-39%), respectively.
Conclusions: Surgical treatment of MR in octogenarians is associated with high perioperative mortality and poor long-term survival with an uncertain benefit on quality of life. These data highlight the importance of patient selection for operative intervention and suggest that future transcatheter mitral valve therapies such as transcatheter mitral valve repair (TMVr) and/or transcatheter mitral valve implantation (TMVI), may provide an alternative therapeutic approach in selected high-risk elderly patients.
Abbreviations
CABG: coronary artery bypass grafting
CI: credible interval
CVA: cerebrovascular accident
MR: mitral regurgitation
MVR: mitral valve replacement
MVRpr: mitral valve repair
NYHA: New York Heart Association
TMVI: transcatheter mitral valve implantation
TMVr: transcatheter mitral valve repair
Introduction
Mitral regurgitation (MR) is the second most common valvular heart disease in developed countries1. Recent epidemiological studies suggest that the incidence of moderate to severe MR rises from 2.4% in patients in their 60’s to >10% in those in their 80’s2. The gold standard treatment for severe symptomatic MR is mitral valve surgery3. However, only a small percentage of octogenarian patients are referred to surgery given the higher operative risks associated with advanced age, the increased concomitant prevalence of comorbid conditions, and the uncertain benefit on quality of life and life expectancy with such treatment4. The increasing incidence of symptomatic MR with advancing age and the uncertainty regarding the optimal treatment strategy for MR in this patient population has generated considerable interest in the development of minimally invasive techniques, including transcatheter mitral valve therapies.
Despite the increased attention to management of MR in the elderly, the optimal management of this valvular condition in octogenarians remains unclear and has not been the focus of attention in any of the various valvular heart disease guidelines. There is a paucity of data regarding outcomes of mitral valve surgery in patients above 80 years of age who are the fastest growing portion of our population.
The goal of this systematic review and meta-analysis was to evaluate the outcomes of mitral valve surgery in octogenarians. This information may help clinical decision making in elderly patients with significant MR and can be used as a future benchmark in the field of transcatheter mitral valve interventions.
Methods
This systematic review and meta-analysis was performed in accordance with the Cochrane Handbook for Systematic Reviews5. We performed an English language literature review of the MEDLINE, EMBASE, and SCOPUS electronic databases through December 2012. We searched for studies that evaluated outcomes of patients over 80 years old undergoing mitral valve surgery for MR. The combined keywords used in the search were: (mitral valve replacement or mitral valve repair or valve surgery) and (octogenarian or “aged, 80 and over”). In addition, reference lists of all pertinent studies were hand-searched for additional relevant work.
We selected studies for analysis that were published in the English language as full-length articles and that reported on surgical outcomes of patients over 80 years of age undergoing mitral valve surgery. Studies that identified surgical outcomes of octogenarians undergoing other valve surgeries were excluded unless they also reported on the outcomes of mitral valve surgeries separately or in combination with coronary artery bypass grafting (CABG), tricuspid annuloplasty, or atrial fibrillation ablation surgery. Foreign language studies, unpublished data, and abstracts were excluded from analysis. Furthermore, we excluded any study with a patient sample size less than 10.
One investigator (A.A.) performed the literature search and identified articles that would potentially report data on the proposed topic. Two investigators (A.A., and S.M.) independently reviewed potentially relevant studies. The studies that did not meet inclusion criteria were not considered for analysis (Figure 1). Data on study period, country of study, study design, study size, types of surgery, patient demographics, operative characteristics, operative mortality and morbidity, and long-term survival were collected and compiled. Disagreements on reporting were clarified by consensus among three authors (A.A., S.M., and N.P.).
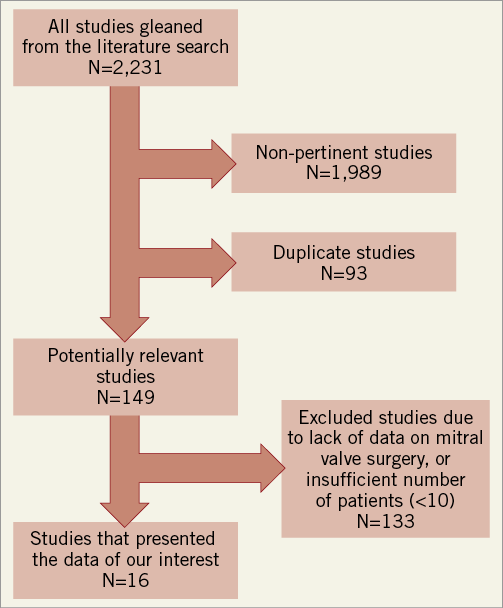
Figure 1. Flow chart of the literature search.
In each individual study we noted the proportion of 30-day hospital mortality following mitral valve replacement (MVR) and mitral valve repair (MVRpr), if available. Also, the proportion of patients who suffered from postoperative cerebrovascular accidents (CVA) and the proportion of long-term survival after one year and after five years were noted following both types of mitral valve surgery. If not directly presented, when feasible, the proportions were calculated from the exact number of patients in each group. The 95% credible intervals for each proportion were estimated using the Wilson score interval method6.
We used Bayesian hierarchical models to estimate the pooled proportion of 30-day mortality, CVA, and long-term survival following the two interventions across studies. In each model, we used non-informative prior distributions for the logit of the pooled proportion and the between-study variance in the logit proportions so as to let the observed data dominate the results. From these analyses we reported the median pooled proportions and their 95% equal-tailed credible intervals (CI). We also reported the 95% CI of the predicted proportion in a new study to estimate the heterogeneity between studies. We depicted the results using forest plots.
For the proportion of patients who died within 30 days of mitral valve surgery, we performed meta-regression models to investigate if the year of study publication explained the heterogeneity in the proportions between studies. For the regression coefficient associated with the covariate, we estimated the median and the corresponding 95% CI as well as the probability that the coefficient was greater than zero. It is acknowledged that the choice of prior distribution over between-study variance can impact on the resulting prior distribution, especially in cases where limited data are available. As a check of robustness, we carried out a sensitivity analysis where we considered different prior distributions proposed in the literature for the between-study variability7. Analyses were carried out using R and WinBUGS software packages8,9.
Results
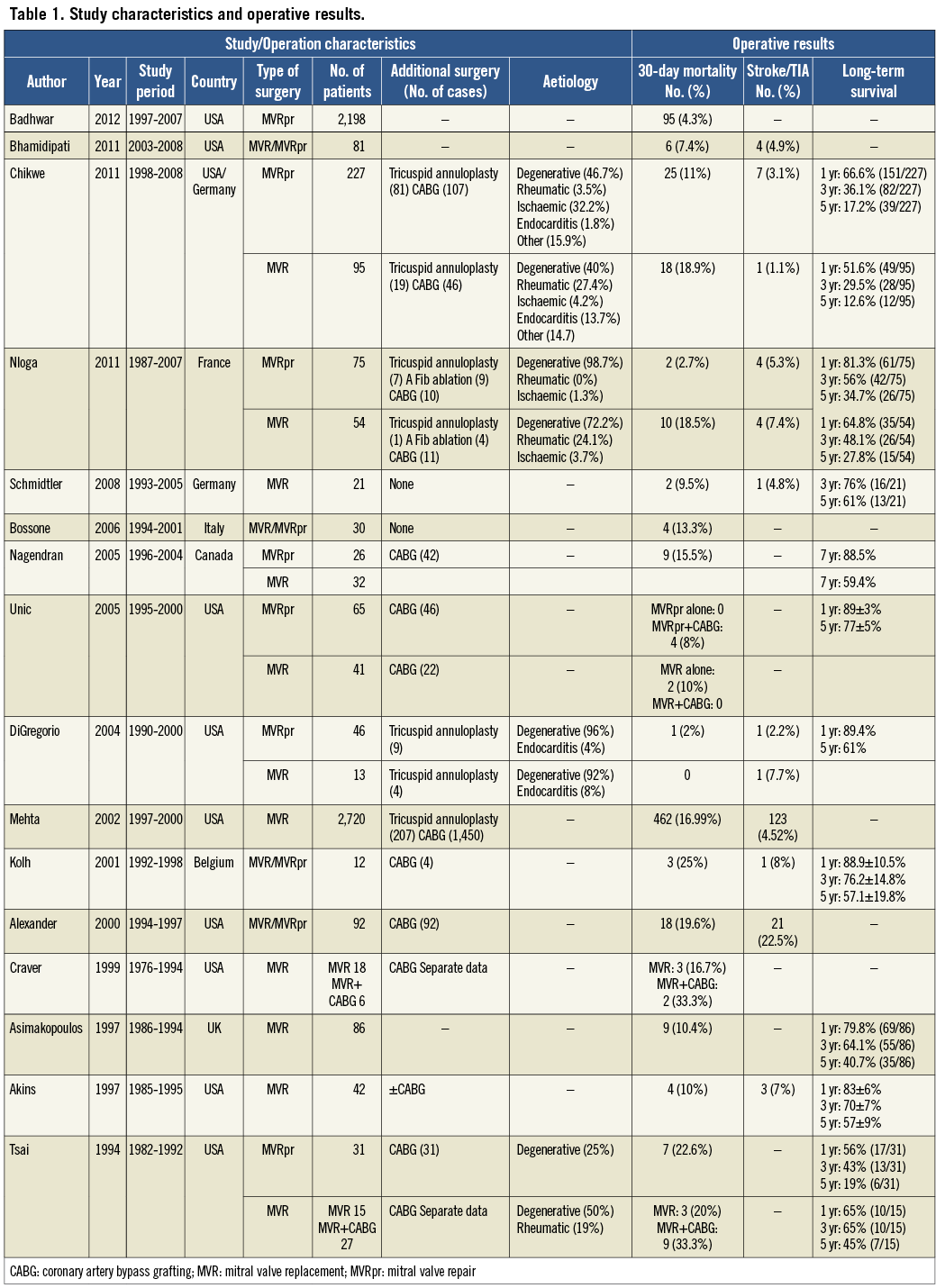
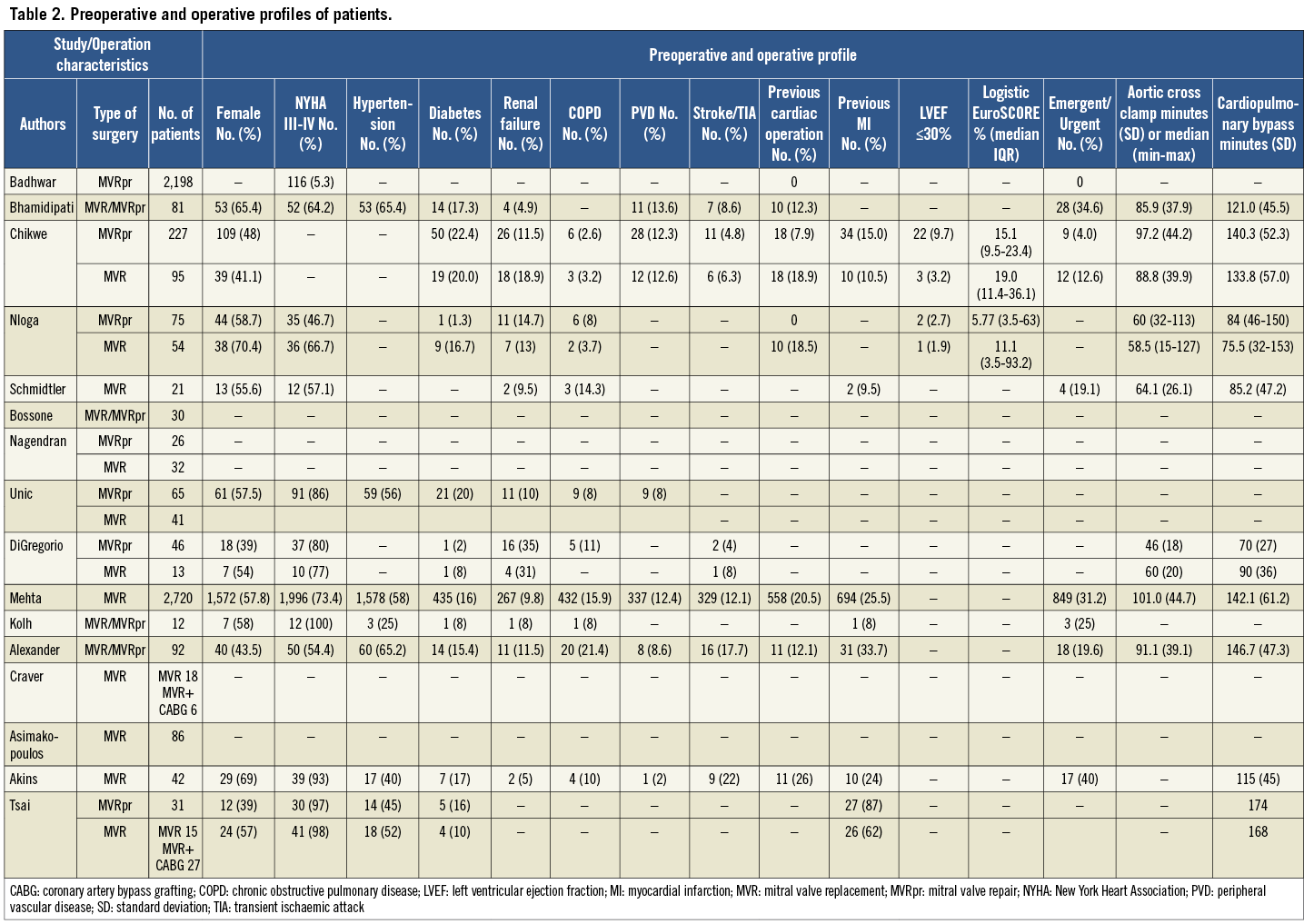
The literature search resulted in a total of 2,231 articles. Of these, 1,989 were not pertinent to our study question and 93 were found to be duplicate studies (Figure 1). We closely analysed 149 studies. Sixteen articles10-25 reported data of interest and fulfilled the inclusion criteria. All studies were retrospective. Table 1 summarises the study characteristics of these sixteen publications as well as information retrieved on the operative results including operative mortality, postoperative CVA, and long-term survival if available. Table 2 summarises the preoperative and operative profiles of the patients in the studies when available.
OPERATIVE MORTALITY
The 30-day operative mortality results of each study are shown in Table 1. Forest plots of operative mortality following MVR and MVRpr are shown in Figure 2 and Figure 3, respectively. The pooled proportions of postoperative 30-day mortality associated with MVR and MVRpr were calculated to be 13% (10 studies, 3,015 patients, 95% CI: 9-18%) and 6% (6 studies, 2,642 patients, 95% CI: 3-12%), respectively. We repeated the analysis after removing the studies that had less than 50 patients undergoing mitral valve surgery, and the pooled proportions of operative mortality associated with MVR and MVRpr were 16% (4 studies, 2,955 patients, 95% CI: 10-25%) and 6% (4 studies, 2,565 patients, 95% CI: 3-11%), respectively. Comparisons of these pooled proportions with the predicted proportions of postoperative mortality following MVR and MVRpr are indicative of significant heterogeneity among the various studies (Table 3).
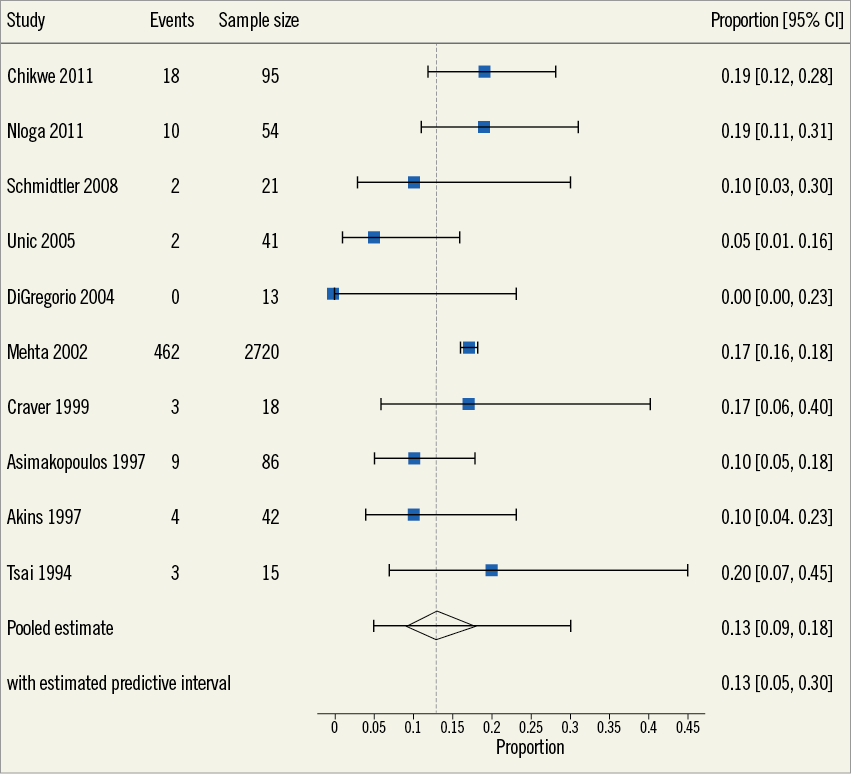
Figure 2. Forest plot of 30-day operative mortality following mitral valve replacement in octogenarians.
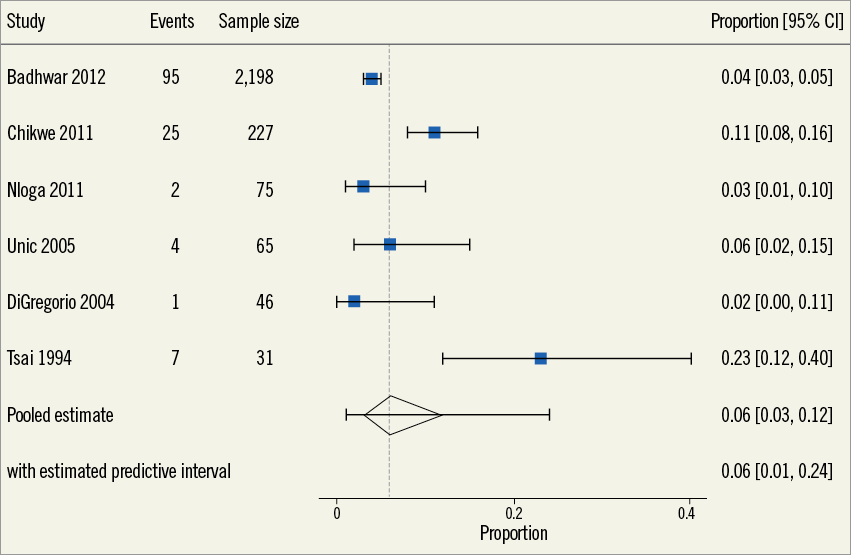
Figure 3. Forest plot of 30-day operative mortality following mitral valve repair in octogenarians.
In addition, a meta-regression analysis was performed to detect an association between the year of publication and the 30-day operative mortality following MVR and MVRpr. No association was found between the year of publication and the mortality outcome following MVR. The median and 95% CI for the regression coefficient associated with the year of study was –0.01 (–0.07 to 0.05) for MVR with the 34% probability that the regression coefficient is greater than zero. However, in the case of MVRpr, the regression coefficient median estimate was 0.07 (–0.03 to 0.12) with a 90% probability of the regression coefficient being greater than zero, suggesting a potential effect of year of publication in this case. However, this significant association would disappear if the results of one study by Tsai et al were disregarded with the regression coefficient median estimate changing to –0.06 (95% CI: –0.3 to 0.15) and the probability of the coefficient being greater than zero being changed to 30%.
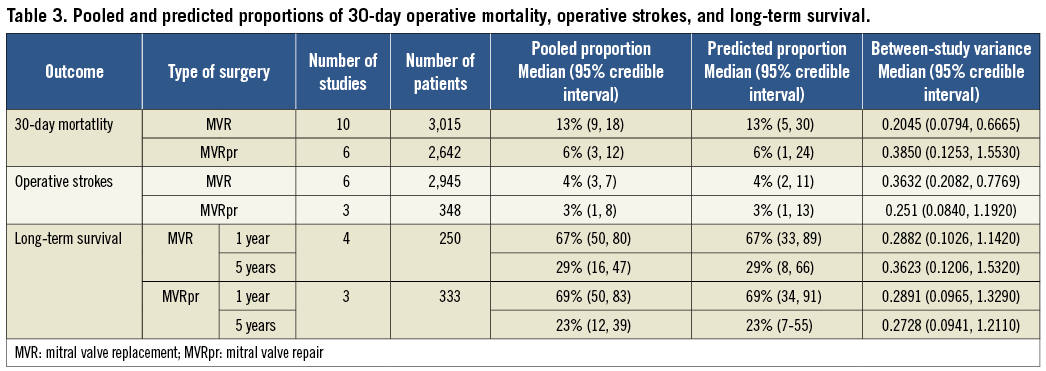
OPERATIVE STROKES AND LONG-TERM SURVIVAL
Pooled proportions of postoperative CVA associated with MVR and MVRpr were found to be 4% (6 studies, 2,945 patients, 95% CI: 3-7%) and 3% (3 studies, 348 patients, 95% CI: 1-8%), respectively. In addition, pooled survival rates at one and five years following MVR (4 studies, 250 patients) were 67% (95% CI: 50-80%) and 29% (95% CI: 16-47%) and following MVRpr (3 studies, 333 patients) were 69% (95% CI: 50-83%) and 23% (95% CI: 12-39%), respectively (Table 3).
Discussion
In the current study we performed a systematic review and meta-analysis of data on octogenarians who underwent mitral valve surgery for MR. The pooled estimate for 30-day operative mortality in octogenarians following MVR was 13% (95% CI: of 9-18%) and that for MVRpr was 6% (95% CI: of 3-12%).
The surgical management of mitral valve disease in octogenarians is a unique and challenging task. These patients often present to surgery in a decompensated state of health and often have numerous comorbidities. Most comorbid conditions including hypertension, diabetes, renal failure, myocardial infarction, and peripheral and cerebrovascular disease increase with age19, and therefore put octogenarians at a higher operative mortality risk compared to younger patients. The 30-day operative mortality rates observed in the present study appear to be 2.3x and 3.8x higher than those reported for the general adult population undergoing MVR (5.7%) and MVRpr (1.6%)26. Our findings lend credence to the expected higher operative mortality of elderly patients undergoing mitral valve surgery compared to the general population.
It is important to note that the aetiology of MR should be taken into consideration in its management strategy. Overall, degenerative mitral valve disease is the most common cause of MR in the elderly27. MVRpr could potentially provide the most suitable surgical option for this kind of valve disease. However, the presence of significant mitral annular calcification in the elderly often makes valve replacement the only feasible invasive treatment option. Furthermore, functional MR due to ischaemic cardiomyopathy is another common pathology in the elderly and its optimal surgical treatment strategy (MVR vs. MVRpr) is the focus of much debate, despite accumulating evidence on the survival advantage of MVRpr over MVR in this context28. Given the above, surgical management of MR in octogenarians should be highly individualised.
The current study also provides important information on the rate of postoperative CVA and long-term survival after mitral valve surgery in an octogenarian population. The pooled proportions of postoperative CVA were calculated to be 4% (95% CI: 2-8) following MVR and 3% (95% CI: 1-8) following MVRpr. These could be compared with postoperative CVA rates of 2.1% and 1.4% observed in the STS database of patients undergoing MVR and MVRpr, respectively26. The higher operative mortality rates, the aforementioned rates of postoperative CVA, and the relatively low five-year survival rates of 29% (95% CI: 16-47) and 23% (95% CI: 12-39) following MVR and MVRpr, respectively, should be taken into consideration when planning for surgical management of an octogenarian patient with significant MR. Identifying the predictors of surgical outcome in this group of patients would be helpful to choose the suitable elderly candidate for mitral valve surgery.
Multiple studies have identified perioperative variables associated with cardiac operative mortality in octogenarians. Kolh et al identified New York Heart Association (NYHA) functional Class IV, urgent procedure, and prolonged extracorporeal circulation as independent predictors of early mortality20. Aortic atheromatous disease and preoperative myocardial infarction were also identified as predictors of postoperative stroke and prolonged hospital stay, respectively. In a similar study, Bossone et al recognised NYHA functional Class IV, diabetes, hypertension, renal insufficiency, rheumatic aetiology, and left ventricular ejection fraction (<45%) as independent risk factors of 30-day postoperative mortality16. In addition, requirement for concomitant CABG operation has been identified as a predictor of operative mortality in elderly patients19. Identifying these predictors in an octogenarian patient with multiple comorbid conditions and the uncertainty regarding the optimal approach to such a patient could pave the way for a role of evolving minimally invasive techniques.
In recent years, enthusiasm and encouraging results with transcatheter aortic valve implantations have directed attention towards the potential treatment of MR using minimally invasive technologies such as transcatheter mitral valve repair (TMVr) and/or transcatheter mitral valve implantation (TMVI)29. Multiple different strategies are currently being explored by various companies including creation of a double-orifice mitral valve using percutaneous edge-to-edge techniques30,31, indirect remodelling of the mitral valve annulus via a coronary sinus device32, direct remodelling of the mitral valve annulus using suture-based techniques, thermal annular remodelling, or mitral ring annuloplasty33, and implantation of artificial cords34,35. Furthermore, the only transcatheter mitral valve repair device that has been implanted in more than 8,000 patients is the MitraClip (Abbott Vascular, Santa Clara, CA, USA), a catheter-based extension of the surgical edge-to edge repair technique36,37.
This technique has been the subject of various studies including the recent randomised trial EVEREST II, where mitral valve surgery was found to be superior to MitraClip for the 12-month primary combined efficacy endpoint, despite having a better safety profile at 30 days38. Since the conclusion of the EVEREST II trial, multiple observational studies have been completed including the recently published study by Conradi et al39 where MitraClip has been compared with surgical MVRpr. In all these studies, while surgery is consistently found to be more effective than MitraClip in reducing MR, a selected group of patients is found to benefit from the transcatheter approach, leading to the conclusion that the success of transcatheter valve therapies relies on an appropriate patient selection process40. In particular, elderly patients with reduced left ventricular function and multiple comorbidities could benefit from the transcatheter mitral repair approach41. In addition, the prospect of TMVI involving the transcatheter delivery and implantation of a bioprosthetic valve in the mitral valve position via a transseptal, transatrial or transapical approach is on the horizon42-47.
Limitations
Finally, it should be noted that our study has several limitations. Other than two large observational retrospective studies10,19, most publications included in the meta-analysis were relatively small in size with the inherent biases of retrospective studies. Also, given the small number of articles included in the meta-analysis, the possibility of publication bias should be taken into account when considering the results. Another limitation of our report is that most studies used in the analysis did not provide separate data on the surgical outcomes of MVR or MVRpr alone. These surgeries were often in conjunction with additional operations such as CABG, tricuspid annuloplasty, or atrial fibrillation ablation (Table 1). Nevertheless, these additional surgeries are often necessary when an octogenarian undergoes a surgical treatment of symptomatic severe MR and should therefore be considered as part of the risk assessment strategy of these patients. In addition, it should be noted that the data of the published work on the operative results following mitral valve surgery in octogenarians could be subject to the preoperative selection bias. Also, the significant heterogeneity that exists across studies as evidenced by comparison of the pooled and the predicted proportions (Table 3) should be taken into consideration while evaluating these results.
Additionally, our meta-regression analysis did not reveal a significant association between the year of publication and operative mortality results following MVR. On the other hand, even though our result shows a potentially significant association between year of publication and surgical mortality outcomes after MVRpr, the significance of this association disappears if the study by Tsai et al25 is disregarded. The absence of such an association despite the recent advances in surgical care is surprising. While the limited number of studies should be taken into consideration, this finding could indicate the complexity of mitral valve surgeries in an increasingly morbid ageing population.
Conclusion
In conclusion, surgical treatment of MR in octogenarians is associated with high perioperative mortality and poor long-term survival. These data highlight the importance of patient selection for operative intervention and suggest that future transcatheter mitral valve therapies such as transcatheter mitral valve repair (TMVr) and/or transcatheter mitral valve implantation (TMVI) may provide an alternative therapeutic approach in selected high-risk elderly patients.
Conflict of interest statement
R. Lange and N. Piazza are consultants to Medtronic, CardiAQ and Highlife. The other authors have no conflicts of interest to declare.

