Abstract
Aims: The aim of this meta-analysis was to compare general anaesthesia (GA) and deep sedation (DS) with regard to safety and length of intensive care unit (ICU) stay in patients undergoing percutaneous edge-to-edge mitral valve repair (PMVR).
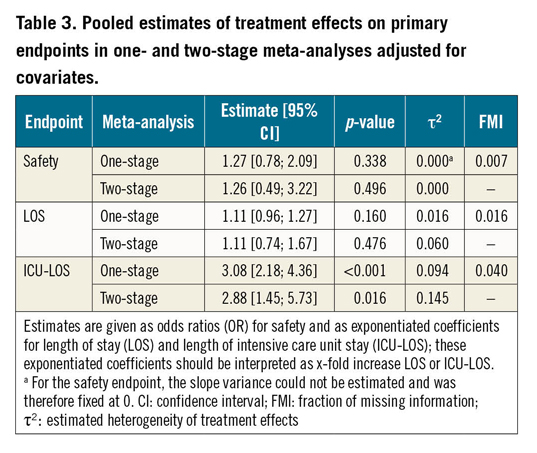
Methods and results: Four studies comparing GA and DS in patients undergoing PMVR were included in an individual patient data meta-analysis. Data were pooled after multiple imputation. The composite safety endpoint of all-cause death, stroke, pneumonia, or major to life-threatening bleeding occurred in 87 of 626 (13.9%) patients with no difference between patients treated with DS as compared to GA (56 and 31 events in 420 and 206 patients, respectively). In this regard, the odds ratio (OR) was 1.27 (95% confidence interval [CI]: 0.78 to 2.09; p=0.338) and 1.26 (95% CI: 0.49 to 3.22; p=0.496) following the one-stage and two-stage approach, respectively. Length of ICU stay was longer after GA as compared to DS (ratio of days 3.08, 95% CI: 2.18 to 4.36, p<0.001, and 2.88, 95% CI: 1.45 to 5.73, p=0.016, following the one-stage and two-stage approach, respectively).
Conclusions: Both DS and GA might offer a similar safety profile. However, ICU stay seems to be shorter after DS.
Introduction
Several trials have shown the role and potential efficacy of percutaneous edge-to-edge repair for both degenerative and functional mitral regurgitation (MR) as compared to optimal medical treatment in patients with increased surgical risk1,2,3. In the beginning, the vast majority of procedures were performed under general anaesthesia (GA)4. However, GA itself carries a considerable risk in patients deemed to be inoperable (e.g., haemodynamic instability, prolonged need for invasive ventilation)5. Further, GA may be associated with a longer stay in the intensive care unit (ICU), which again influences clinical outcome as well as human resources and financial expense6,7,8. Deep sedation (DS) arose as a potential alternative strategy to facilitate percutaneous edge-to-edge mitral valve repair (PMVR)9. In most circumstances, local experience drives the decision on the anaesthetic strategy chosen. Data supporting either strategy are sparse. Therefore, the primary objective of this meta-analysis is to summarise and pool data of all available studies investigating the feasibility and safety of the MitraClip® (Abbott Vascular, Santa Clara, CA, USA) procedure under DS in comparison to GA.
Methods
The methods are described in detail in Supplementary Appendix 1.
STATISTICAL ANALYSIS
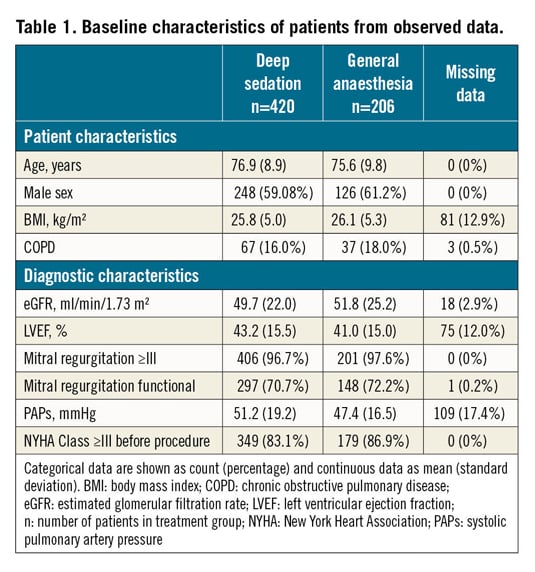
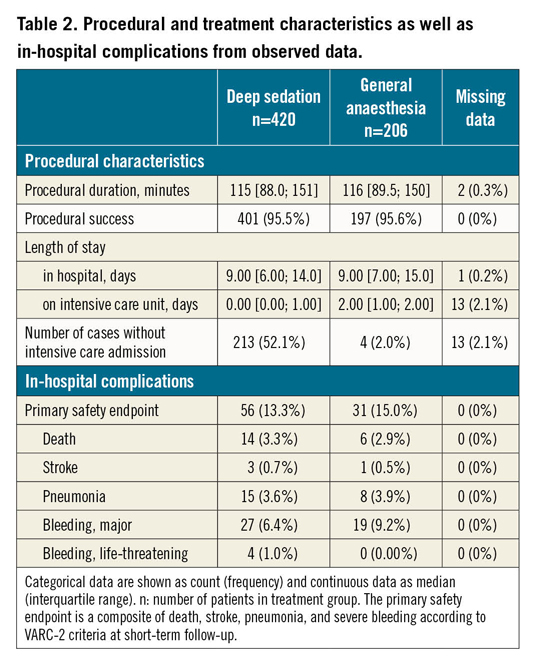
We calculated summary statistics for patient characteristics, preprocedural diagnostics, procedural characteristics, and outcomes stratified by anaesthesia group as mean and standard deviation (SD), or if skewed (as judged by inspection of histograms) as median and interquartile range (IQR). We used frequencies and percentages to summarise categorical variables. All descriptive statistics were derived from observed data. Numbers and distribution of missing values are depicted per study and in total.
Missing data were handled with multiple imputation using chained equations10.
We conducted one-stage and two-stage meta-analyses to estimate pooled effects of PMVR performed under DS in comparison to GA (Supplementary Figure 1, Supplementary Figure 2). In both approaches, we adjusted regression models for the following confounders: age, sex, body mass index, New York Heart Association (NYHA) functional Class ≥III, presence of chronic pulmonary disease, estimated glomerular filtration rate, left ventricular ejection fraction (LVEF), systolic pulmonary artery pressure, and procedure duration.
Primary efficacy and safety outcomes were analysed by means of logistic regression models (logit link). The number of days for length of hospital stay as well as length of ICU stay were analysed by means of Poisson regression models (log link). The resulting regression coefficients are on the log scale. Exponentiation of these regression coefficients provides estimates of the treatment effect on a multiplicative scale (i.e., a ratio or factor). For this reason, we refer to these treatment effects as a ratio throughout the text, in Tables, and in Figures.
All p-values were two-sided and judged as significant if less than 0.05. All analyses were conducted using R version 3.4.0 (R Foundation for Statistical Computing, Vienna, Austria) and used predominantly the following packages: mice for multiple imputation of missing data, lme4 for one-step meta-analysis, meta for two-step meta-analyses, and mitml for pooling estimates according to Rubin’s rules.
Results
We identified 24 reports of interest for this meta-analysis. After screening titles and abstracts, four reports of monocentric observational studies remained11,12,13,14. All of these studies were judged eligible after evaluation of the full text in detail and all principal investigators agreed to provide individual patient data. The study of Rassaf et al randomised patients in a non-blinded fashion to either DS or GA. Patients were also included in the overall observational study of Horn and co-workers leading to exclusion of this trial13,15. Therefore, four studies enrolling 626 patients in total were included in the meta-analysis. Baseline characteristics and procedural characteristics are summarised in Table 1 and Table 2, respectively. Data regarding in-hospital complications were complete for all patients. In the studies included, sedation was achieved with midazolam and propofol in the DS group. Sedation was guided and titrated by the cardiologist performing transoesophageal echocardiography. An anaesthesia team performed GA with endotracheal intubation in the GA group (Supplementary Table 1). The risk of bias assessment is described in Supplementary Appendix 2 and Supplementary Table 2.
MISSING DATA AND MULTIPLE IMPUTATION
In the merged data set containing observed data from all studies as provided by the study investigators, a total of 303 data points (3.0%) were missing. The proportion of missing data per variable ranged from 0 to 17.4% (Table 2, Table 3, Supplementary Table 3). In 232 of 626 (37.1%) patients, at least one value was missing. Performing a traditional complete case analysis would have substantially reduced the sample size (by 37.1%). Instead, we used multiple imputation, which provided the basis for the statistical analyses. The validity of the imputation procedure was assessed by investigating convergence plots and by comparing the distribution of the imputed data to the observed data (Supplementary Figure 3). However, the additional uncertainty introduced by missing data was only modest, as indicated by the relatively low proportion of missing data per variable and the small fraction of missing information (FMI) estimated for the results of the meta-analyses.
META-ANALYSIS
Procedural success rates were very high, irrespective of the assigned treatment group (i.e., in 401 of 420 patients [95.5%] for DS and in 197 of 206 patients [95.6%] for GA). The low number of procedures without procedural success precluded reliable regression models. Therefore, we did not perform formal meta-analyses for the primary efficacy endpoint.
The distribution of outcome variables in the observed data set is depicted in Table 2 and Figure 1 (both show plain summary statistics without weighting). The one- and two-stage meta-analyses based on the imputed data revealed that the length of hospital stay did not differ significantly between patients undergoing PMVR with GA or DS (Table 3, Figure 2A). In contrast, the length of ICU stay was longer in patients undergoing general anaesthesia as compared to deep sedation (Table 3, Figure 2B). For example, according to the one-stage meta-analysis, the length of ICU stay was 3.08 times longer in patients treated with GA versus DS.
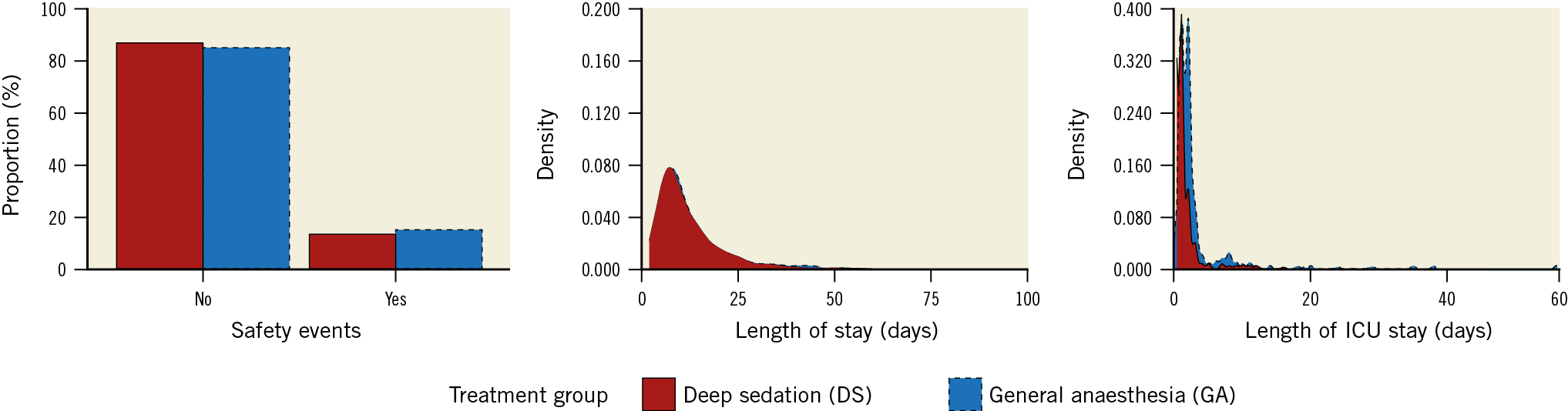
Figure 1. Distribution of outcome variables in observed data. The number of safety events relative to the number of patients by treatment group (left) as well as the density distribution of length of total hospital stay (middle) and length of ICU stay (right) are shown.
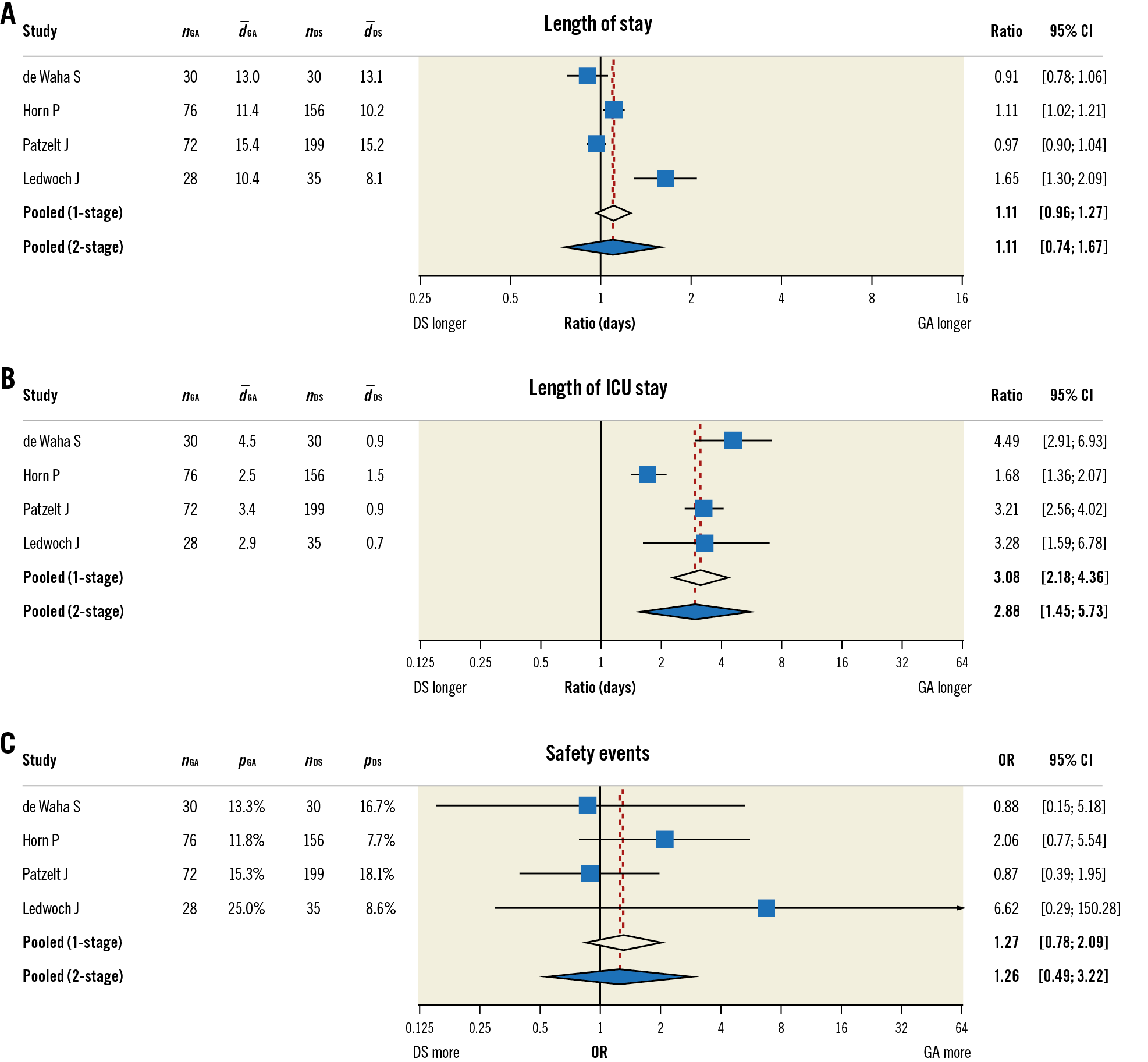
Figure 2. Forest plot showing treatment effect estimates and 95% confidence intervals for individual studies and the pooled treatment effects in the one- and two-stage meta-analyses for (A) length of hospital stay, (B) length of intensive care unit stay, and (C) the primary safety endpoint alongside the number of patients per group (nGA, nDS), the mean length of stay per group in days (d_GA, d_DS; only A & B), and the proportion of patients with safety event per group (pGA, pDS; only C). The point estimates and 95% confidence intervals for individual studies were based on the two-stage meta-analyses. The size of the blue-coloured squares corresponds to the relative weight of the respective study in the two-stage meta-analyses. “Ratio” denotes the exponentiated coefficients of the treatment effect, which can be interpreted as the factor (i.e., x-fold) by which the length of stay is prolonged due to treatment strategy. DS: deep sedation; GA: general anaesthesia; OR: odds ratio
The frequency of safety events in the observed data set is depicted in Table 2 and Figure 1. In addition, Table 2 depicts the frequency of single outcome events which – when summed up – compose the primary safety outcome. Neither treatment strategy was associated with a significant increase in the risk for safety events, as indicated by the estimates of the treatment effects and their 95% confidence intervals (CIs) in the one- and two-stage meta-analyses (Table 3, Figure 2C). However, for all endpoints, the CIs were relatively wide, especially in the two-stage meta-analyses, indicating substantial uncertainty about the point estimates. The FMI was low in all one-stage meta-analyses, indicating that the missing data introduced only little uncertainty in these estimates.
In order to check a possible impact of confounder adjustment on the results, we repeated all meta-analyses without adjusting for covariates. However, these analyses led to very similar results (Supplementary Table 4) and will thus not be considered in detail.
The estimated between-study variance indicated substantial heterogeneity in the true effect sizes across studies for both length of stay (two-stage τ2 = 0.060, I2 = 86.8%, 95% CI [68.3%; 94.5%]) and length of ICU stay (two-stage τ2 = 0.145, I2 = 88.4%, 95% CI [72.9%; 95.1%]) but not for the safety endpoint (two-stage τ2 = 0.000, I2 = 0%, 95% CI [0%; 84.6%]) (Table 2).
Several subgroup analyses were pre-specified to study possible sources of heterogeneity. These are reported in Supplementary Appendix 3 and Supplementary Figure 4-Supplementary Figure 6.
Discussion
This meta-analysis pooled individual patient data of 626 patients who were enrolled in four prospective observational studies. As a result, this meta-analysis comprises a sample of similar size to well-known registries such as the Transcatheter Valve Treatment Sentinel Pilot (n=628)16 and the Transcatheter Mitral Valve Interventions registry (n=643 to 828 depending on the report)17,18,19. Our study focused on the impact of the chosen anaesthetic method on procedural success, procedural safety, length of hospital stay, and length of ICU stay. The main finding was that DS appears to be a safe and effective alternative to GA in patients undergoing PMVR. Moreover, DS was associated with shorter length of ICU stay but with a similar overall length of hospital stay as compared with GA.
Procedural success, defined as successful placement of at least one clip and reduction of mitral regurgitation to ≤II°, was very high (i.e., >95%) irrespective of the anaesthetic method used. This success rate is in line with reports of other registries16,18,20.
Our composite primary safety endpoint comprised in-hospital complications (i.e., death, stroke, pneumonia, and major or life-threatening bleeding) and occurred in 87 of the 626 (13.9%) patients. Most of these safety events were bleedings (50 of 87 safety events [57.5%] and 50 of 626 patients [8.0%]). The bleeding rate in our population was comparable to the bleeding rate of 7.4% reported for the TRAMI registry which used a similar bleeding definition17. Fortunately, more devastating events such as deaths or strokes were rare and occurred at similar rates to other registries (e.g., TRAMI 2.2% and 0.9%, respectively17).
The issue of procedural safety as a function of the anaesthetic method is of clinical relevance but has not been addressed by other registries so far. As a matter of fact, the majority or nearly all patients in other registries have been treated with GA16,18,20. A national consensus paper from Germany also recommended performing PMVR under GA4. Theoretically, GA offers advantages over DS such as a patient lying still, pausing ventilation for critical steps during the procedure, and the possibility for quick conversion to bail-out surgery, which might facilitate a safer procedure. Patients treated with DS with an unprotected airway are supposed to be at risk for aspiration with subsequent pneumonia. However, GA itself carries a risk of adverse events. Among patients with heart failure, the risk of adverse perioperative events might be higher in patients with severely reduced ejection fraction21. In our meta-analysis, neither anaesthetic method was associated with a higher risk of in-hospital complications in the total sample. Naturally, this finding does not preclude the possibility that such a difference might still exist, especially given the limited number of studies and the resulting uncertainty in the estimated treatment effects. However, this finding was consistent across meta-analytic approaches and with the findings of the individual studies included in our meta-analysis, thus providing more robust evidence due to the larger sample size (n=626 in our meta-analysis versus n=60 to 271 in individual studies). Moreover, the individual patient data approach allowed us to adjust analyses for patient level confounders known to be associated with procedural success and adverse events.
While length of ICU stay was shorter with DS as compared to GA, this was not the case for the overall length of stay. This might be counterintuitive at first glance. However, the length of stay was quite long with a median of nine days. This suggests that most procedures were performed after stabilisation following admission for acute decompensated heart failure and not electively. However, a shorter length of hospital stay is probably beneficial from an economic point of view. Since organisation and workflow differ considerably between hospitals, the need for an anaesthesia care team for GA might be a challenge or an organisational bottleneck in one hospital but not in another. Moreover, organisation and workflow within a hospital may evolve in parallel to increasing experience with PMVR, leading to some kind of “fast track” GA with extubation immediately on the operating table without the need for ICU admission. In contrast, the shorter ICU stay with DS as compared to GA in the studied population was driven primarily by the fact that patients were not admitted to the ICU at all (i.e., zero days on ICU) in a considerable proportion of patients treated with DS. Therefore, the difference in length of ICU stay may not be present in contemporary populations.
We used a multiple imputation strategy that accounted for the hierarchical structure of the data as well as between-study heterogeneity. The key advantage of multiple imputation in general is that it allows using all of the available data and making inferences under the assumption that the data are missing at random (MAR) given the observed data on outcomes and covariates22. This is in contrast to complete-case analyses, which can lead to a severe loss of information and operate under much stricter assumptions as compared with multiple imputation23. Moreover, a complete case analysis uses only a subset of the available observations, thus reducing the power to detect statistically significant differences. In the case of our meta-analysis, a complete case analysis of the adjusted mixed regression model for in-hospital complications would have discarded 37.1% of the patients.
The individual patient data approach also allowed us to perform subgroup analyses on the patient level. The most conspicuous finding here suggests that patients with reduced ejection fraction might suffer more in-hospital complications when undergoing GA as compared to DS, whereas patients with preserved ejection fraction might not. However, subgroup analyses were not adjusted for multiple testing and therefore should be interpreted with caution until further evidence from additional studies becomes available.
The association of procedural safety and the chosen anaesthetic method was not modified by either preprocedural systolic pulmonary pressure or age. Tigges et al studied the implication of pulmonary hypertension in patients undergoing PMVR based on the TRAMI population19. They found that increased values of preprocedural systolic pulmonary pressure are associated with an increased risk of post-discharge mortality at one year but not with periprocedural complications. Together, this suggests that PMVR is safe in patients with elevated systolic pulmonary pressure irrespective of the anaesthetic methods.
DS was achieved by continuous application of propofol and repeated bolus applications of midazolam in all studies. No strict targets for the depth of sedation were defined prospectively. The physician performing transoesophageal echocardiography monitored the depth of sedations clinically to ensure that the patient tolerated all aspects of the procedure while maintaining spontaneous breathing. In all studies, GA was performed by an anaesthetist. Propofol was used as hypnotic drug in combination with an opiate for this purpose. Both approaches are standard of care in most institutions.
Limitations
The following limitations should be acknowledged. First, the studies included in our meta-analysis were prospective but observational. Large-scale randomised controlled trials investigating the optimal anaesthetic procedure are currently lacking. To work on methodical shortcoming by pooling data from observational studies, we adjusted our analyses for known risk factors for procedure-related complications and/or an unfavourable short-term outcome. Probably due to the fact that GA and DS were historical comparisons in most included studies, the observed patient characteristics were quite well balanced between groups. However, we were unable to control for unobserved confounders, for which randomisation would be the reference standard. Therefore, all findings of our meta-analysis should be interpreted with caution because such studies cannot replace evidence from large-scale randomised trials. The choice between GA and DS was not a historical comparison but rather based on the Heart Team consensus in the study of Patzelt et al14. Therefore, patient selection might have influenced the result on length of ICU stay in this study. However, the direction of the effect is not different in the other studies (Figure 2B). The patients’ health status seems, therefore, unlikely to explain the observed difference in length of ICU stay between GA and DS. Second, we were unable to adjust subgroup analyses for confounders as we did for the main analyses due to statistical problems with model convergence and total separation. This is a frequent issue with fitting some regression and mixed-effects models24. The total sample size of our meta-analysis is an improvement compared to the individual studies but is still rather small from a statistical point of view. This is most likely the cause of the problems encountered during fitting mixed-effects regression models. Having more studies would probably avoid these issues and allow an even more thorough investigation into the effects of DS versus GA. Assessment of the primary efficacy endpoint and safety endpoint (i.e., clinical events of in-hospital complications) followed standard operating procedures of the local institutions and were not assessed by means of a core echocardiography laboratory or independent clinical events committee, respectively. Therefore, we cannot fully exclude detection or attribution bias that may be inherent in the included studies. Third, the Mitral Valve Academic Research Consortium introduced the updated MVARC bleeding scale in 2015, which is a modified version of the VARC-2 bleeding scale25. Bleeding events were prospectively adjudicated according to the VARC-2 bleeding scale in all included studies. Unfortunately, data were not recorded in such detail that the bleeding scale could be updated reliably in retrospect. However, comparing both scales (Supplementary Table 5) reveals that only minor discrepancies exist. One relevant discrepancy is that fatal bleeding is separated from life-threatening bleeding as a distinct entity in the MVARC bleeding scale.
Conclusions
In conclusion, our meta-analysis suggests that PMVR is feasible using either deep sedation or general anaesthesia, length of ICU stay may be shorter with deep sedation as compared to general anaesthesia, and procedural safety may not be different between these two anaesthetic techniques.
|
Impact on daily practice Transcatheter mitral valve repair can be performed under deep sedation or general anaesthesia. The results of this meta-analysis suggest that either method may be safe, and the choice should be based on the expertise of the centre and operators. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.