Since its inception in 2003, percutaneous edge-to-edge mitral valve repair (PMVR) for mitral regurgitation has experienced explosive growth, with >100,000 procedures performed globally to date. The vast majority of these procedures have long been performed with the patient under general anaesthesia (GA); only a disproportionate fraction of patients is being treated under deep sedation (DS).
In this issue of EuroIntervention, Jobs and colleagues present findings from an individual patient data meta-analysis that compared procedural success rate, in-hospital complications, length of hospital stay, and length of intensive care unit (ICU) stay in patients who received either GA or DS during PMVR1.
The authors conclude that both the procedural success rate and safety profile were similar between the GA and DS groups. Although the length of overall hospitalisation was similar between groups, length of ICU stay was significantly shorter after DS. The authors suggest that the choice of anaesthetic approach (GA versus DS) should be based on the expertise of the site and the operators.
Despite the rigorous statistical methodology applied, all four studies included in the meta-analysis were observational studies and therefore the generalisability is limited. The decision to proceed with DS versus GA in the four studies analysed was not random. Some patients may have received GA because they were high-risk or had other clinical features. The authors have made commendable efforts in an attempt to account for a potential selection bias but, despite the finesse of their applied statistical techniques, the risk of confounding still remains. To date, no appropriately sized randomised controlled study has compared GA and DS use during PMVR.
As the authors noted, GA offers several advantages when compared to DS for PMVR. These include an immobilised patient, ability to hold ventilation during key procedural steps, and the potential for an expedited conversion to bail-out surgery. While the latter is exceedingly rare, there are a number of other relevant advantages that GA offers. First, having a member of the anaesthesia team provide the anaesthetics permits the interventional echocardiographer to focus entirely on procedural image guidance during PMVR. Expert echocardiographic guidance is a highly demanding task that involves continuous image interpretations and real-time communication with the implanter. With the expansion of PMVR indications to include mitral valve pathologies such as extensive leaflet prolapse, large coaptation gap, commissural disease, and failed surgical repair, the undivided attention of the echocardiographer during the procedure is more important than ever. In addition, technological advances in transcatheter device system and echocardiographic imaging capability require both the implanter and imager to pay the closest attention to detail at all times. Second, imaging with transoesophageal echocardiography (TEE) is greatly facilitated in an immobilised patient under GA. Not only can the imager achieve a more stable TEE probe position by minimising probe manipulations but multi-beat high temporal resolution images may be acquired during 3D TEE (colour) imaging with minimal respiratory interference. Third, intraprocedural TEE in a patient under GA may result in fewer TEE-related injuries, apart from procedural complications, compared to TEE manipulation in a sedated patient who may be uncomfortable, potentially moves, coughs or gags. A recent study demonstrated that most patients undergoing structural cardiac interventions show some form of oesophageal or gastric injury associated with TEE, with longer procedural time and poor or suboptimal image quality associated with an increased risk2. It should also be noted that patients with difficult airways, inability to lie flat during the procedure, obstructive sleep apnoea, or high baseline pain medication requirements are typically selected to receive GA.
When discussing the potential advantages or disadvantages of DS, it is essential to obtain a clear definition of DS, since the level of sedation is a continuum rather than a distinct state and patients can experience a wide range of depths of anaesthesia - from simple anxiolysis to GA (Figure 1),3. Administering midazolam or an infusion of propofol without continuously assessing the effects of the sedative or analgesic medications on the level of consciousness and on cardiopulmonary function may result in hugely variable effects on the individual patient. In fact, societal guidelines have advocated for dedicated personnel to monitor the patient and not be involved in the diagnostic or therapeutic procedure itself3. Assuming that a sedation-only approach to PMVR is safe, potential advantages include the demonstrated safety feasibility, the avoidance of potential complications associated with GA and the opportunity to reduce overall cost. Disadvantages associated with performing the PMVR under sedation only include the potential for an unprotected airway and the risk of aspiration and undesired patient movements.
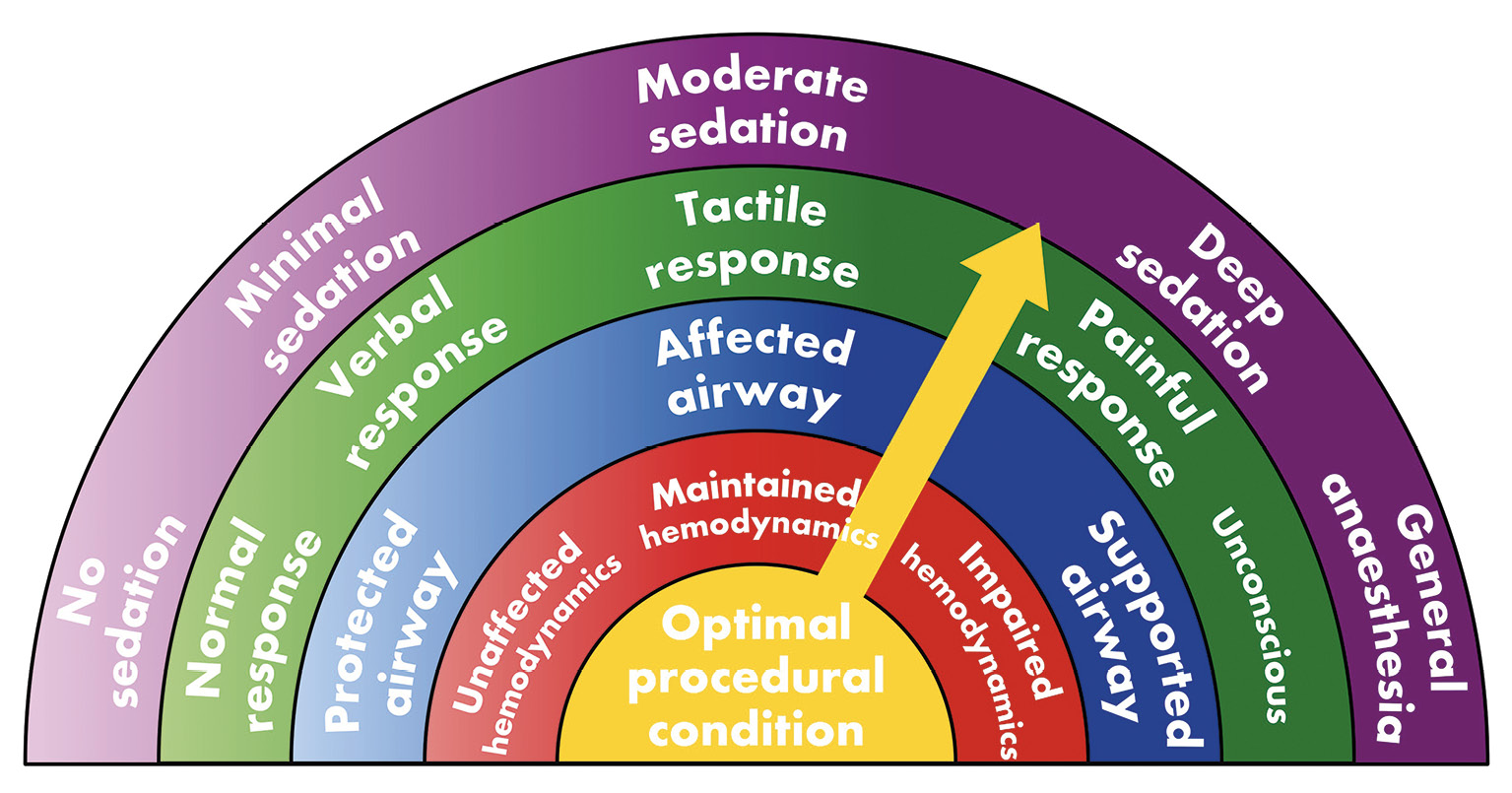
Figure 1. Wheel of factors characterising the spectrum of sedation. Achieving the optimal procedural condition is multifactorial and probably site- and operator-specific.
What are the possible next steps regarding the choice of anaesthetic management for the evolving field of PMVR? If the experience with transcatheter aortic valve replacement (TAVR) can provide guidance, the number of PMVRs performed under sedation will probably only increase over time. However, without any large-scale prospective evidence, comparative effectiveness research or formal implementation research to delineate characteristics of the optimal care model, we may ultimately be guided by considerations of cost-effectiveness and convenience. Considering the diversity of perspectives raised here and in the work by Jobs and colleagues, we are embracing an exciting new era that moves away from simply managing or avoiding risk towards a true systematic approach that defines, measures and modulates drivers of value when treating structural heart disease. In the future, alternative strategies include performing the PMVR under conscious sedation only and adopting alternative imaging tools such as intracardiac echocardiography or smaller footprint TEE transducers may become reality. However, 3D imaging capability and equivalent image quality compared to standard TEE probes should not be sacrificed.
Conflict of interest statement
G.B. Mackensen reports unpaid advisory work and contributions to a Japan/Asia advisory board organised by Abbott Structural Heart Solutions. R. Sheu has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.