Introduction
The gold standard for the treatment of mitral regurgitation (MR) is cardiac surgery. The mitral valve is a complex functional apparatus made up of leaflets, annulus, chordae, papillary muscle and left ventricle. The surgeon is able to use many appropriate techniques to repair or replace the mitral valve and data are available from many years of follow-up. Despite this, about 50% of patients with symptomatic severe MR do not receive any surgical treatment because of absolute contraindications or high surgical risk due to the presence of many comorbidities. Since optimal medical therapy could be ineffective in controlling the symptoms and patients on medical therapy have a worse prognosis when compared to those who receive surgical treatment, percutaneous repair techniques open up new alternative solutions in selected patients.
Percutaneous mitral repair devices
Percutaneous replacement is still in the development phase and many issues still have to be overcome. On the other hand, CE-mark approved percutaneous mitral repair devices, aiming to simulate surgical repair, permit a complete percutaneous repair.
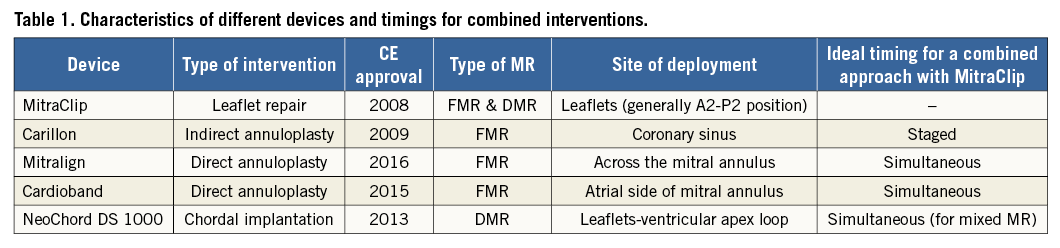
CE-mark approved devices are: the MitraClip® System (Abbott Vascular, Santa Clara, CA, USA) (approved in 2008) for leaflet edge-to-edge repair; the Carillon® Mitral Contour System® (Cardiac Dimensions Inc., Kirkland, WA, USA) (approved in 2009) for indirect annuloplasty; the Cardioband® (Valtech Cardio, Or Yehuda, Israel) and Mitralign (Mitralign Inc., Tewksbury, MA, USA) (approved in 2015 and 2016, respectively) for direct annuloplasty; and the NeoChord (NeoChord Inc., St. Louis Park, MN, USA) (approved in 2013) for transapical chordae implantation (Figure 1).
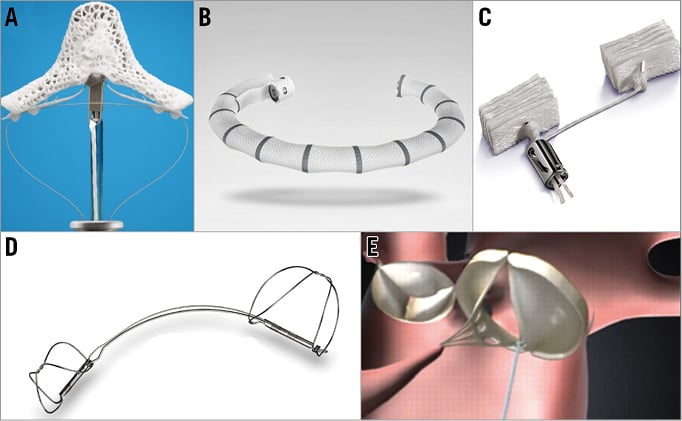
Figure 1. CE-mark approved devices for MR treatment. A) MitraClip NT; B) Cardioband; C) Mitralign; D) Carillon; E) NeoChord.
The most studied device is the MitraClip, with more than 30,000 patients treated worldwide. This device reproduces the surgical edge-to-edge technique, creating a double orifice and providing an immediate and consistent reduction of MR both in functional mitral regurgitation (FMR) and degenerative mitral regurgitation (DMR). In the surgical edge-to-edge series there have been concerns about duration when not associated with annuloplasty. Using the MitraClip System, the leaflets are deeply inserted into the clip and the width of the implant is greater, even using more than one clip if needed, than surgical edge-to-edge stitch. This provides a larger amount of grasped tissue, which could lead to better long-term durability. Still, we have seen that the results at follow-up (FU) are affected by annular dimension and LV size.
The Cardioband provides a surgical-like annuloplasty from trigone to trigone and has demonstrated, even if this is in a small series of patients, up to 30% of annular size reduction with a high success rate and sustained results.
The Mitralign is a system for direct annuloplasty with intra-annular insertion of a couple of pledgets for annulus plication and concomitant annular reduction. The results are good in just 50% of patients.
The Carillon system offers an indirect annuloplasty with a nitinol device anchored into the coronary sinus to reduce annulus dimensions. It is safe and easy but only provides a modest reduction in MR. All the systems for annuloplasty, direct or indirect, work only in FMR patients and, as of today, taking all these systems into consideration, around 1,000 patients have been treated.
The NeoChord DS 1000 is not truly percutaneous since the intervention is performed by the transapical approach; however, as it is a mini-invasive device, it can be included in the percutaneous family.
Combined transcatheter mitral valve repair techniques
The combination of different devices could have a synergic effect and improve percutaneous repair results. While annuloplasty helps to reduce the tension on the leaflets, edge-to-edge improves the coaptation and the results. Nevertheless, the experience concerning the combined use of different devices is limited to isolated case reports.
Unlike surgery, percutaneous interventions provide the possibility of a staged approach. Probably the best approach could be to perform the annuloplasty first and then the edge-to-edge. Since annuloplasty devices work in different ways, they can give different results even in combination with a MitraClip or other device. For example, the Carillon device does not give an immediate reduction in MR so one should wait at least six months to assess the results and in order to decide whether or not to implant a MitraClip. Potential benefits of this staged approach therefore include the possibility of closely evaluating midterm results following the first procedure and optimising results with a second and complementary intervention only if truly needed. Optimisation of results is indeed crucial in this group of patients since the degree of residual MR has been identified as an independent predictor of adverse outcomes at follow-up.
On the other hand, the Cardioband device provides an immediate MR reduction so that the need of an additional edge-to-edge repair can be evaluated immediately. This simultaneous “double shot” could be useful in order to reduce costs resulting from a second hospitalisation. Similarly to surgical rings, the Cardioband could also serve as a support for TAVI devices in the mitral position for mitral valve replacement.
In an extreme hypothetical treatment scenario, a combination of percutaneous annuloplasty, edge-to-edge and chordae implantation can give a fully percutaneous repair. Table 1 summarises the basic characteristics of the available devices and also includes the ideal timing of intervention for a combined percutaneous approach.
However, we have to take into account the drawbacks of combined percutaneous interventions. First, the selection of patients is crucial in order to choose the right device to implant and the right timing. Actually, not all patients are technically operable with all devices: whether the repair is to be done with one device or using multiple devices in a single or in staged procedures should be assessed in each patient. In this last option the complexity of the procedure could prolong its duration and raise the risk of complications. Second, the use of multiple devices requires experienced echocardiographers and interventionalists very skilled in the use of all devices. Last but not least, the economic impact is not negligible. In many countries the elevated price of percutaneous devices raises many issues in terms of reimbursement and limits the number of patients who can be treated. Using more devices together will raise the costs in an unsustainable way for the majority of healthcare systems.
Until now, the issue of a combined percutaneous approach using different techniques for the treatment of mitral valve disease has been poorly explored in the literature. Indeed, there are only a few cases or small case series that have been previously reported concerning this topic. In a previous report, our group showed that MitraClip implantation was feasible and effective in a patient with prior percutaneous annuloplasty using the Carillon system. Similarly, MitraClip implantation was feasible in six patients with failed surgical annuloplasty.
Conclusions
Nowadays, a double/triple shot to the mitral valve is already technically feasible and could improve acute results and long-term durability of the percutaneous treatment of MR. Despite technical feasibility, we have to consider the increased risk and complexity of a combined procedure. Moreover, the actual costs of the devices make this approach limited to selected patients but, in the near future, with increasing operator experience with the devices and lower costs, this could become the standard percutaneous approach in high surgical risk patients.
Conflict of interest statement
C. Grasso is a proctor for Abbott Vascular.