Abstract
Aims: The number of percutaneous edge-to-edge mitral regurgitation valve repairs with MitraClip implantation has increased during recent years. Published studies showed promising safety outcomes in relatively small cohorts, while results from large samples are sparse. Thus, we aimed to evaluate trends and safety outcomes in the German nationwide in-patient sample.
Methods and results: We analysed data on patients’ characteristics and in-hospital safety outcomes for all percutaneous mitral valve repairs using the MitraClip technique in Germany between 2011 and 2015. Overall, 13,575 in-patients were included. The annual number of MitraClip implantations increased from 815 in 2011 to 4,432 in 2015 (β 1.00 [95% CI: 0.96-1.03], p<0.001). The in-hospital mortality (p=0.193) and major adverse cardiac and cerebrovascular events (MACCE) (p=0.183) rate remained unchanged. Important independent predictors of in-hospital mortality were heart failure (OR 1.91 [95% CI: 1.43-2.54], p<0.001), transfusion of erythrocyte concentrates (OR 9.04 [95% CI: 7.45-10.96], p<0.001), stroke (OR 6.82 [95% CI: 4.34-10.72], p<0.001), endocarditis (OR 19.52 [95% CI: 9.04-42.14], p<0.001), pulmonary embolism (OR 7.61 [95% CI: 3.44-16.81], p<0.001), pericardial tamponade (OR 14.08 [95% CI: 7.09-27.96], p<0.001) and pericardial effusion (OR 2.59 [95% CI: 1.66-4.04], p<0.001).
Conclusions: MitraClip implantations increased markedly (5.4-fold) between 2011 and 2015, with a constant in-hospital mortality and MACCE rate. Our data indicate that edge-to-edge mitral valve repair using the MitraClip technique has acceptable in-hospital safety outcomes in a real-world scenario.
Abbreviations
ACC: American College of Cardiology
AF: atrial fibrillation/flutter
AHA: American Heart Association
DMR: degenerative mitral valve regurgitation
EACTS: European Association for Cardio-Thoracic Surgery
ESC: European Society of Cardiology
FMR: functional mitral valve regurgitation
G-DRG: German diagnosis-related groups
HF: heart failure
ICB: intracerebral bleeding
ICD-10-GM: International Classification of Diseases and Related Health Problems, 10th Revision with German Modification
LA: left atrial
LV: left ventricular
MACCE: major adverse cardiac and cerebrovascular events
MI: myocardial infarction
MR: mitral valve regurgitation
NYHA: New York Heart Association
OPS: Operationen- und Prozedurenschlüssel (surgery and procedures codes)
TRAMI: transcatheter mitral valve interventions
VHD: valvular heart disease
Introduction
Mitral valve regurgitation (MR) is the most common heart valve disease in Europe and the USA1-3. Its prevalence increases with age and it affects approximately 9-10% of individuals aged 75 years and older4,5. MR is a frequent valve disorder referred for surgical or interventional correction2,6,7. Significant MR is accompanied by substantial morbidity and mortality3,4,6,8,9.
The aetiology of MR is heterogeneous with regard to the underlying pathophysiology and pathoanatomy2,3. In chronic primary degenerative MR (DMR), pathology of the valve leaflets is present and a subsequent correction of the MR is mostly curative. In secondary functional MR (FMR), the mitral leaflets are anatomically normal and severe left ventricular (LV)/left atrial (LA) dysfunction with LV volume/pressure overload and LV/LA enlargement, annular mitral valve dilatation and/or severe leaflet tethering prevents mitral leaflet coaptation, resulting in MR2,7,10. Thus, FMR is only one component of the different aspects of the disease and restoring MR itself might be beneficial, but is not the singular curative treatment approach7,10.
Although surgical mitral valve repair is the approach recommended by the guidelines for the majority of patients with severe DMR (who are at low surgical risk), surgical treatment for high-risk patients is problematic. The treatment of FMR is still under debate because of a significant rate of recurrence and lack of clear evidence of clinical benefit11. Transcatheter repair for FMR patients at high surgical risk is currently under investigation in four randomised controlled trials including 288 to 749 patients each (transcatheter mitral valve interventions [TRAMI], Sentinel-EU, MITRA-FR, COAPT-US and RESHAPE-2)5,12-17.
The current guidelines of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)7 as well as of the American Heart Association (AHA) and the American College of Cardiology (ACC)8 recommend consideration of percutaneous edge-to-edge procedure in high-risk patients with severe symptomatic MR and DMR in the USA, and both primary and secondary MR in most other parts of the world. Patients are eligible if they have mitral valve morphology suitable for MitraClip® (Abbott Vascular, Santa Clara, CA, USA) implantation, are judged not suitable for surgery by a “Heart Team” and have a reasonable life expectancy7,8.
Although several studies showed promising safety outcome data in cohorts smaller than 1,000 treated patients5,13-15, results from a real-world nationwide sample are missing. To fill this gap, we investigated trends and safety outcomes of the transcatheter-based treatment of patients with MR in the German nationwide in-patient sample.
Material and methods
DATA SOURCE
The analyses were performed on our behalf by the Research Data Center of the Federal Statistical Office and the Statistical Offices of the federal states in Wiesbaden, Germany (DRG Statistics 2011-2015, own calculations). The aggregated statistical results were provided on the basis of SPSS codes (SPSS® software, Version 20.0; IBM Corp., Armonk, NY, USA), which we sent to the Research Data Center. For this analysis, we selected all hospitalised patients who were coded with a MitraClip procedure between 2011 and 2015.
DIAGNOSES, PROCEDURAL CODES, AND DEFINITIONS
Diagnoses are coded according to the International Classification of Diseases and Related Health Problems, 10th Revision with German Modification (ICD-10-GM) and surgical or interventional procedures according to the German Procedure Classification (Operationen- und Prozedurenschlüssel [OPS] – surgery and procedures codes). All DRG diagnoses of in-patients are collected and evaluated by the Federal Statistical Office of Germany (Statistisches Bundesamt). Thereby, we identified all hospitalised patients who were relevant for our analysis, based on the OPS code for transvenous MitraClip procedures (OPS code 5-35a.41).
STUDY SAFETY OUTCOMES
The measured safety outcomes of this study were death from any cause during the hospital stay (in-hospital death), major adverse cardiac and cerebrovascular events (MACCE, including in-hospital death, myocardial infarction [MI; ICD-code I21] and/or ischaemic stroke [ICD-code I63]), and clinically relevant bleeding events such as haemopericardium (ICD-code I31.2), intracerebral bleeding (ICB; ICD-code I61) and the need for transfusion of erythrocyte concentrates (OPS code 8-800).
ETHICAL ASPECTS
Since this study did not involve direct access to data of individual patients by the investigators, approval by an ethics committee and informed consent were not required, in accordance with German law.
STATISTICAL METHODS
Statistical analyses are described in Supplementary Appendix 1.
Results
BASELINE CHARACTERISTICS
The nationwide sample included 13,575 in-patients undergoing percutaneous mitral valve repair using the edge-to-edge MitraClip technique in Germany between 2011 and 2015. The calculated prevalence for the performance of edge-to-edge clip implantation was 3.35 per 100,000 citizens per year (over this five-year time frame). The majority of patients were male (60.0%) and the mean age was 77 years, comparable to published registry data (Supplementary Table 1, Supplementary Table 2). Among these patients, 87.6% presented with dyspnoea in New York Heart Association (NYHA) Classes III/IV. Additionally, 67.3% were diagnosed with coronary artery disease, 46.0% with renal insufficiency, 30.8% with diabetes mellitus and 15.0% with chronic obstructive pulmonary disease (COPD).
NON-SURVIVORS VERSUS SURVIVORS
Comparisons of non-survivors and survivors are described in Supplementary Appendix 2 and Supplementary Table 1.
PREDICTORS OF IN-HOSPITAL MORTALITY
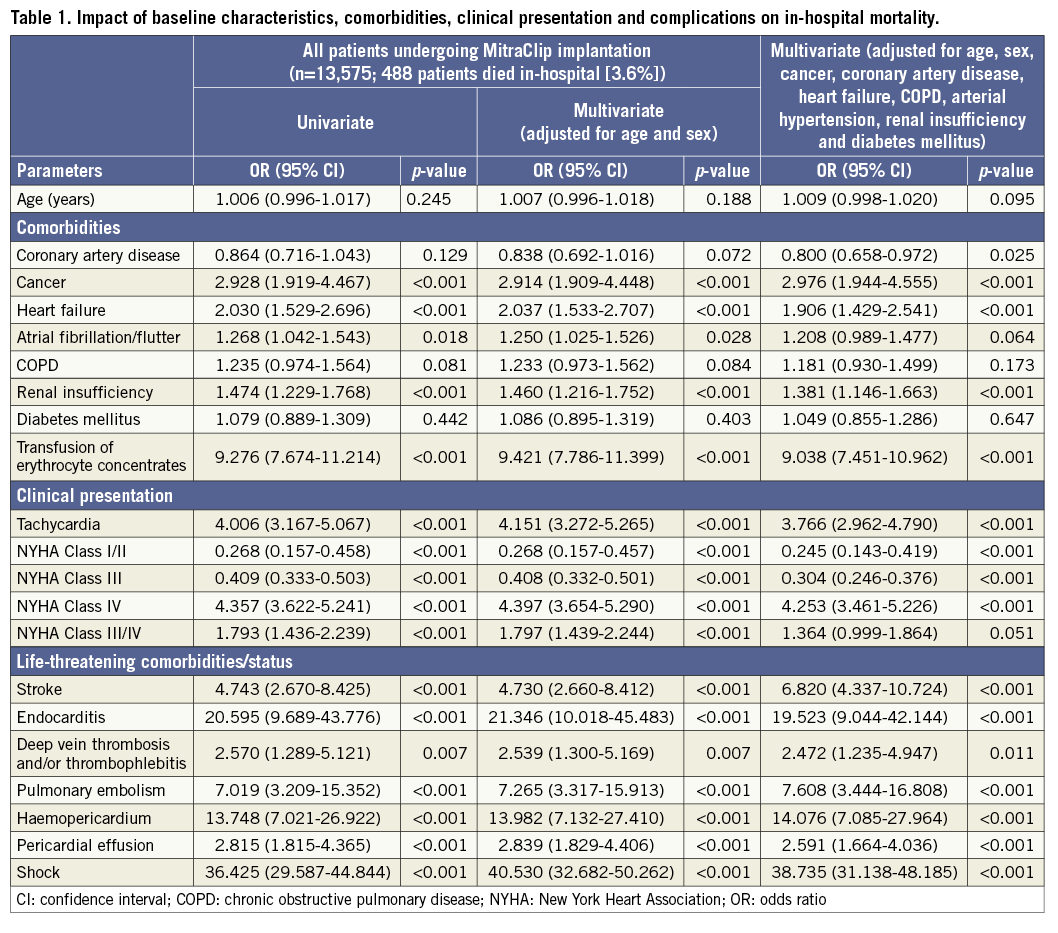
Independent predictors of in-hospital mortality in a multivariate analysis (adjusted for sex, age and comorbidities) with an OR >1.5 were cancer, heart failure (HF), transfusion of erythrocyte concentrates, tachycardia, NYHA Class IV, stroke, endocarditis, pulmonary embolism, haemopericardium, pericardial effusion, and shock (Table 1).
TRENDS BETWEEN 2011 AND 2015 AND ACROSS AGE GROUPS IN GERMANY
Total numbers of edge-to-edge MitraClip implantations increased over the five-year period (β 1.00 [95% CI: 0.96 to 1.03], p<0.001). The in-hospital mortality rate remained roughly constant at 3.1% in 2011 and 3.6% in 2015 (β 0.07 [95% CI: −0.04 to 0.19], p=0.193) (Figure 1A, Supplementary Table 3), as did the MACCE rate (ß 0.06 [95% CI: −0.03 to 0.14], p=0.183) at 5.6% in 2011 and 6.8% in 2015, while age at the procedure increased significantly during this period (ß 0.06 [95% CI: 0.01-0.01], p<0.001) (Figure 1B, Supplementary Table 3). Regarding age group distribution, the majority of MitraClip implantations (79.2%) were performed in patients aged between 70 and 89 years, with the lowest in-hospital mortality being between 70 and 79 years (3.1%) (Figure 1C). The number of patients in NYHA Classes III/IV (ß 0.03 [95% CI: 0.04 to 0.13], p<0.001) (Figure 2A) increased. In-hospital stay remained unchanged at 10 days in 2011 and 10 days in 2015 (p=0.271) (Figure 1B, Supplementary Table 3). While shock was more prevalent in age decades six and seven, the prevalence of renal insufficiency and the need for transfusion of erythrocyte concentrates increased with growing age (Supplementary Figure 1). Of note, the transfusion of erythrocyte concentrates decreased considerably from 2011 (23.6%) to 2015 (14.7%) (ß −0.06 [95% CI: −0.25 to −0.14], p<0.001) (Supplementary Table 3), whereas the rate of the safety outcomes endocarditis and stroke remained similar over the reported time frame (Figure 2B, Supplementary Table 3).
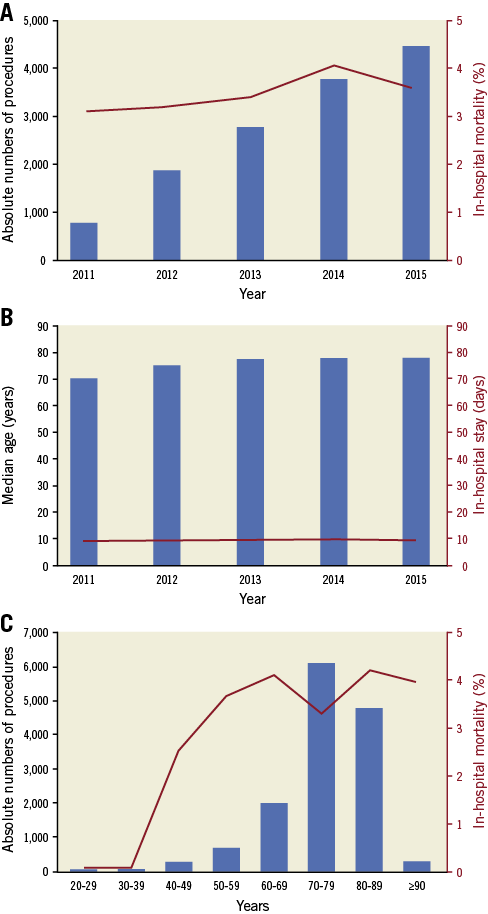
Figure 1. Absolute annual numbers and in-hospital mortality after MitraClip implantation. A) From 2011 to 2015. B) Median age and median in-hospital stay in the years 2011-2015. C) Stratified by age group.
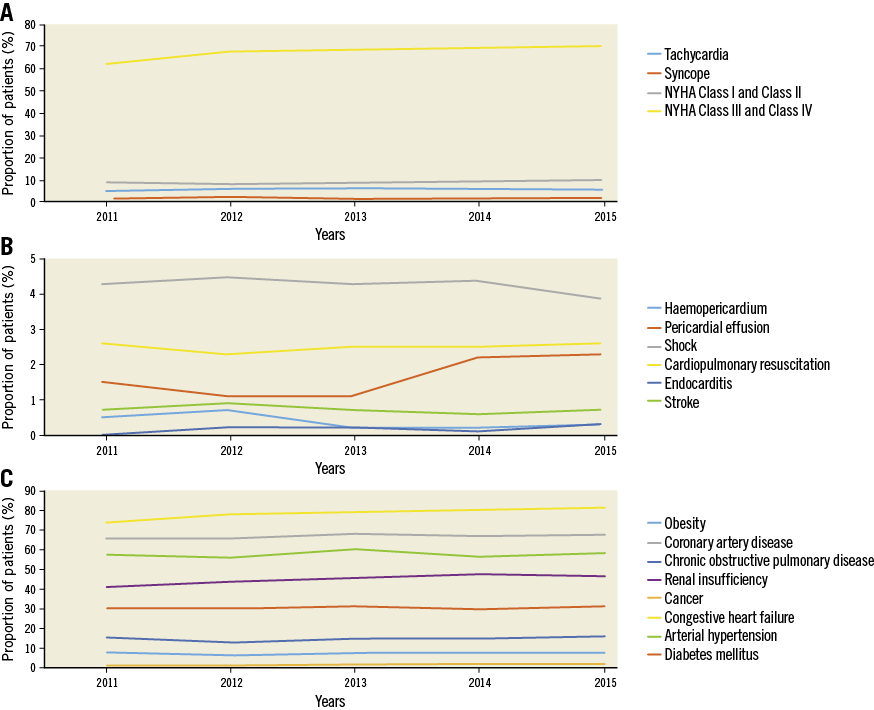
Figure 2. Trends regarding comorbidities, clinical parameters/signs of haemodynamic compromise and more severe mitral valve regurgitation (end-stage disease), and complications from 2011-2015. A) Clinical parameters/signs of haemodynamic compromise and more severe mitral valve regurgitation (end-stage disease). B) Complications. C) Comorbidities.
The comorbidities of treated patients changed only slightly over time. We observed a small increase in the frequency of cancer, HF, atrial fibrillation/flutter (AF), COPD, renal insufficiency and peripheral artery disease over the five-year period (Figure 2C, Supplementary Table 3).
Discussion
This large nationwide study included more than 13,500 MR patients treated with edge-to-edge mitral valve repair using the MitraClip technique. Previously published reports included much smaller populations, with the largest investigating 1,064 subjects5,13-16.
It is unknown whether the aging population and improved diagnostic and treatment methods are associated with changes in the incidence, shift of patient characteristics, age and trends in safety outcomes of patients undergoing MitraClip procedures over time. A unique focus of the present study was to investigate temporal trends in prevalence, in-hospital stay, patient characteristics, safety outcomes and complications of MitraClip procedures over the five-year period between 2011 and 2015.
The key findings of our study comprise the following. 1) We observed a marked increase in the annual numbers of MitraClip procedures over this five-year period. 2) Patient characteristics shifted towards older age and a higher prevalence of HF with higher NYHA class from 2011 to 2015. 3) In-hospital mortality and the MACCE rate remained stable over time. 4) Important predictors of in-hospital death were HF, need for transfusion of erythrocyte concentrates, stroke, endocarditis, pulmonary embolism, pericardial effusion and haemopericardium, and shock. 5) The MitraClip procedures were predominantly performed in the age group between 70 and 89 years.
In a large European survey, it was shown that approximately half of the patients with severe MR were not referred for surgery18. Patient characteristics which were independently associated with a decision not to operate the MR were lower LV ejection fraction, non-ischaemic aetiology, older age, higher Charlson comorbidity index, and grade three MR18. Correspondingly, our results confirm a marked increase of the annual numbers of MitraClip procedures as a less invasive method for MR repair has become available for these high-risk patients (Figure 1A). Thus, in future it has to be expected that the procedural number of percutaneous edge-to-edge valve repairs will increase markedly.
COMPARISON OF TRAMI AND TCVT WITH THE GERMAN NATIONWIDE SAMPLE – BASELINE AND COMORBIDITIES
The TRAMI registry represents the largest previously reported cohort of patients treated with MitraClip5. Patient age and days of in-hospital stay are comparable to the German nationwide in-patient sample. Acute kidney injury is known to be a predictor of subsequent mortality after a transcatheter valve repair, which could be based on contrast- or drug-induced nephropathy, atheroemboli or renal hypofusion19. The TRAMI registry5 showed more renal insufficiency (65.5%) compared to the TCVT registry15 (30.5%) and the German nationwide sample (46.0%) (Supplementary Table 2). Notably, renal insufficiency was identified as a predictor (OR 1.38 [95% CI: 1.15-1.66], p<0.001) of in-hospital death in our study5. Rudolph et al showed that patients in NYHA Class IV had considerably higher mortality than patients in lower NYHA classes20. NYHA Classes III/IV were present in 89.0% of all patients in TRAMI and 85.5% in the TCVT registry and therefore comparable with the German nationwide sample with 87.6%. NYHA Class IV was found to be an important predictor of in-hospital mortality in our study. Both the TRAMI registry and the German nationwide sample showed that patients undergoing MitraClip implantation in real-world practice are older and sicker than in the selected EVEREST trial cohort, with German nationwide sample patients having older age and with more being in NYHA Classes III/IV5,12-14.
PREDICTORS OF IN-HOSPITAL MORTALITY IN THE GERMAN NATIONWIDE SAMPLE
The rate of MACCE is higher in the German nationwide in-patient sample compared to TRAMI (Supplementary Table 2)5. These differences were possibly driven by including patients from only high-volume centres in TRAMI. The German nationwide sample represents a real-world sample, which includes MitraClip implantations from every high-volume as well as low-volume centre in Germany.
The current guidelines recommend the use of antithrombotic and antiplatelet treatment after MitraClip implantation due to a possible risk of thrombus formation with embolic risk of stroke7,21. Studies have reported a stroke rate of 1.1% after transcatheter MitraClip implantation13,22, which was higher compared with the TRAMI registry (0.8%)5 and the German nationwide sample (0.7%). Stroke was found to be a strong predictor of in-hospital death in our cohort. It is well known that bleeding and blood transfusion after transcatheter valve procedures have been strongly associated with mortality23. Our study showed a higher bleeding and transfusion rate compared to the EVERST-II cohort24, the ACCESS-EU study14, the TCVT registry15 and the TRAMI registry5. We demonstrated that transfusion of blood constitutes a strong predictor of in-hospital death. This is the first nationwide study sample reporting predictors of in-hospital safety outcomes and thus a head-to-head comparison of our results to other studies is not feasible. However, predictors of in-hospital mortality were tested in a multivariable analysis and were in line with one-year mortality predictors from the TRAMI registry5. Cancer and tachycardia were identified as predictors of in-hospital mortality in our study. Periprocedural and post-procedural conditions such as pericardial effusion, haemopericardium, endocarditis and shock were also identified as strong predictors of in-hospital mortality. In our study, AF was not an independent predictor of in-hospital mortality, which is in accordance with the study of Velu et al25; the authors reported that AF was also not an independent predictor of long-term mortality25.
TRENDS IN MITRACLIP IMPLANTATION
While the current study revealed a marked increase in MitraClip implantations over this five-year period, the in-hospital mortality and the MACCE rate remained stable.
There was a significant shift towards higher age and higher prevalence of HF with higher NYHA class from 2011 to 2015 (Supplementary Table 3). This might indicate an increasing number of patients with FMR since HF as well as NYHA Class IV are typical attributes of FMR. We can only speculate about this coherence, since we could not distinguish between FMR and DMR aetiology in the nationwide sample data. Among patients with HF and FMR, two large trials reported divergent results. While the MITRA-FR trial12 indicated that FMR patients with HF revealed no significant prognostic benefit as a result of MitraClip implantation additional to optimal drug therapy compared to optimal drug therapy alone after one-year follow-up, the larger COAPT-US trial17 reported a significant benefit of additional MitraClip implantation in addition to optimal drug therapy regarding hospitalisation for HF and all-cause mortality after a two-year follow-up.
Germany is one of the leading countries regarding MitraClip implantations worldwide and, in contrast to other European countries, the German health insurance system provided reimbursement for both DMR and FMR following the ESC VHD guidelines of 2012 and 2017. Over recent years, experience with the MitraClip system has increased markedly, and both younger and more critical patients with severe MR have been treated with MitraClip, resulting in distinctly increased numbers of MitraClip implantations. In particular, the number of MitraClip procedures in old patients at high surgical risk has increased substantially.
In-hospital mortality and MACCE rates did not decrease, probably due to patients of a higher age and with more comorbidities being treated. MitraClip procedures were predominantly performed in the age group between 70 and 89 years, whereas patients <70 years still remain in the minority. While shock was more prevalent in age decades six and seven, the prevalence of important comorbidities increased with advancing age (Supplementary Figure 1).
Limitations
There are limitations to our study that require consideration. The analysis is based on ICD discharge codes, which might have led to incomplete data due to underreporting/undercoding. As mentioned above, we could not distinguish between FMR and DMR aetiology. Therefore, the focus of our study was on clear endpoints such as in-hospital death and complications (MACCE among others) which are very unlikely to be miscoded or not coded. This study includes in-hospital results and cannot address long-term outcomes.
Conclusions
The use of MitraClip implantation increased 5.4-fold from 2011 to 2015, with a constant in-hospital mortality and MACCE rate despite increasing patient age and frequency of comorbid conditions. Our data indicate that MitraClip implantations have acceptable in-hospital safety outcomes in a real-world scenario.
| Impact on daily practice Our data indicate that MitraClip procedures have acceptable in-hospital safety outcomes in a real-world scenario. Moreover, our study underlines that periprocedural haemopericardium, and also pericardial effusion and transfusion of erythrocyte concentrates have to be considered as independent predictors of in-hospital death. |
Acknowledgements
We thank the Federal Statistical Office of Germany (Statistisches Bundesamt, DEStatis) for providing the data/results and giving their kind permission to publish these results (source: RDC of the Federal Statistical Office and the Statistical Offices of the Federal States, DRG Statistics 2005-2015, own calculations).
Funding
This work was supported by the German Federal Ministry of Education and Research (BMBF 01EO1503). The authors are responsible for the contents of this publication.
Conflict of interest statement
R.S. von Bardeleben reports having received consultancy and lecture honoraria from Abbott Structural Heart, Boehringer Ingelheim, Cardiac Dimensions, Edwards Lifesciences, GE Health Systems and Philips Healthcare. L. Hobohm reports having received lecture honoraria from MSD. F. Kreidel reports having received consultancy and lecture honoraria from Abbott, Cardiac Implants, and Edwards Lifesciences. E. Schulz reports lecture honoraria from Edwards Lifesciences and Medtronic. S. Konstantinides reports having received consultancy and lecture honoraria from Bayer, Boehringer Ingelheim, Daiichi Sankyo, MSD and Pfizer – Bristol-Myers Squibb, and institutional grants from Actelion, Bayer, Boehringer Ingelheim, Daiichi Sankyo and Pfizer – Bristol-Myers Squibb. M. Lankeit reports having received consultancy and lecture honoraria from Actelion, Bayer, Daiichi Sankyo, MSD and Pfizer – Bristol-Myers Squibb, and research funding from B.R.A.H.M.S./Thermo Fisher Scientific. T. Feldman reports research grants and honoraria from Abbott, BSC and Edwards Lifesciences. T. Münzel is PI of the DZHK (German Center for Cardiovascular Research), partner site Rhine-Main, Germany. The other authors have no conflicts of interest to declare.
Supplementary data
Supplementary Appendix 1. Statistical methods.
Supplementary Appendix 2. Supplementary results.
Supplementary Figure 1. Trends in baseline comorbidities and complications across age groups.
Supplementary Table 1. Baseline characteristics, medical history and presentation of the patients undergoing percutaneous mitral valve repair using edge-to-edge MitraClip implantation.
Supplementary Table 2. Comparison across the TRAMI registry, the TCVT registry and the German nationwide in-patient sample.
Supplementary Table 3. Trends in total numbers of MitraClip procedures, patient characteristics, complications and safety outcomes over the five-year period.
To read the full content of this article, please download the PDF.