Introduction
Acute mitral regurgitation (MR) may develop in the setting of an acute myocardial infarction (AMI) as a result of papillary muscle dysfunction or rupture. Acute ischaemic MR without papillary muscular rupture may induce severe MR due to leaflet tethering produced by the sudden onset of regional or global left ventricular dysfunction. This can lead to pulmonary oedema or cardiogenic shock during the acute or subacute phase of the MI1. Although previous experience with the MitraClip® (Abbott Vascular, Santa Clara, CA, USA) for correcting MR following AMI has been reported2, data on consecutive patients treated for this condition are lacking and the issue remains understudied. The aim of this registry was to collect the largest experience of acute MR following AMI treated with the MitraClip in Europe.
Methods
This is a prospective registry of all consecutive patients with severe MR which developed early after an acute transmural myocardial infarction who underwent percutaneous mitral valve repair (PMVR) at 11 centres across Europe between January 2016 and December 2018. The main exclusion criterion was low probability of success with the device. Clinical condition did not contraindicate the procedure. Detailed inclusion and exclusion criteria and more information regarding methods are shown in Supplementary Appendix 1.
Results
Between January 2016 and December 2018, 883 cases were treated with the MitraClip in the recruiting centres. Among them, 44 (5%) patients (63.6% male, mean age 70.0±10.8 years) were included in the study. Median time from MI to treatment was 18 days (13-36.8 days) and from diagnosis of MR to treatment 12.5 days (4.5-18 days).
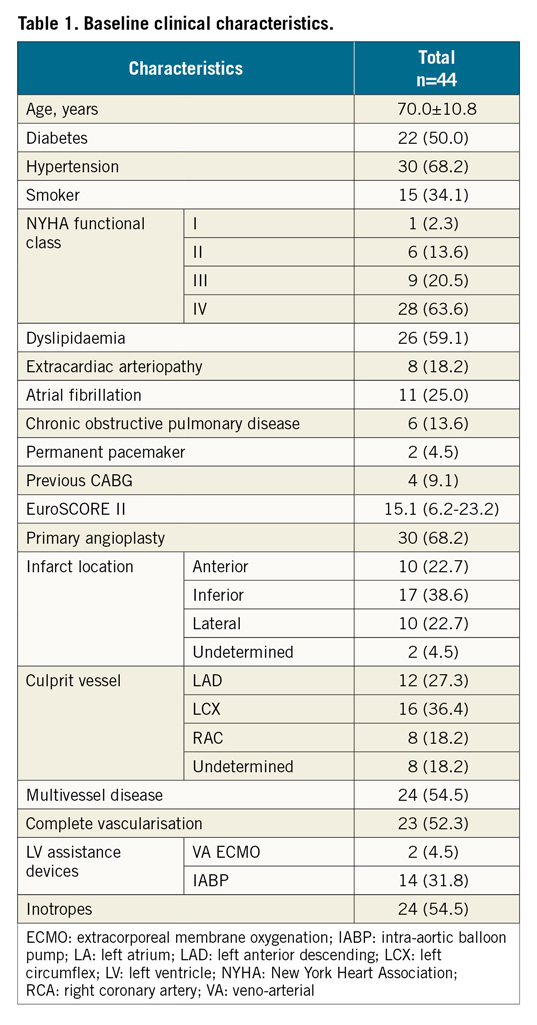
BASELINE CHARACTERISTICS
The baseline characteristics of the entire population are presented in Table 1. Surgical risk was extremely high, with a median EuroSCORE II of 15.1 (6.2-23.2). Baseline echo characteristics are shown in Supplementary Table 1.
PROCEDURE AND 30-DAY FOLLOW-UP
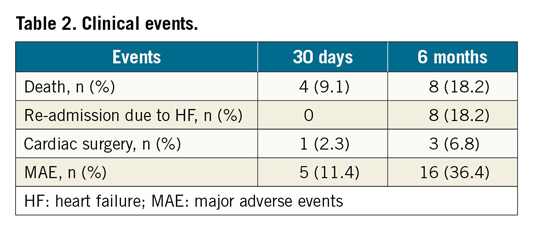
Technical success was obtained in 86.6% of cases with a median of two clips per case (range 1-2). The median gradient post clip was 3 mmHg (2-4) and the median length of stay of patients after the procedure was 16 (8-27) days. Clinical events at 30 days are shown in Table 2. None of the extracorporeal membrane oxygenation (ECMO) patients died during hospitalisation.
SIX-MONTH FOLLOW-UP
MR grade ≤2+ and New York Heart Association (NYHA) functional class are shown in Figure 1. Clinical events at six months are shown in Table 2. Median follow-up was 4.0 (1-7) months. Kaplan-Meier survival curves of freedom from mortality and major adverse events (MAE) are shown in Figure 2.
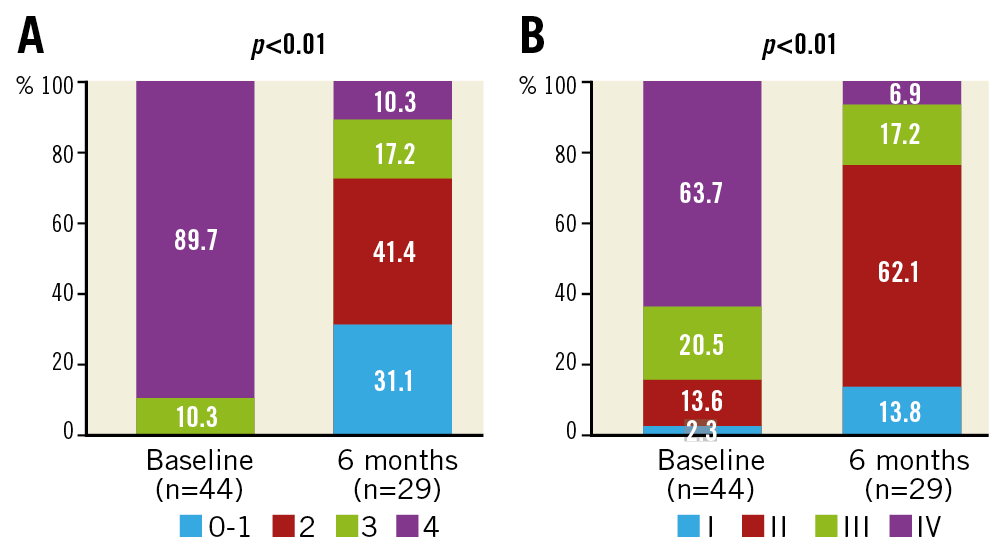
Figure 1. MR reduction and NYHA functional class improvement from baseline to six-month follow-up. A) MR reduction. B) NYHA functional class improvement.
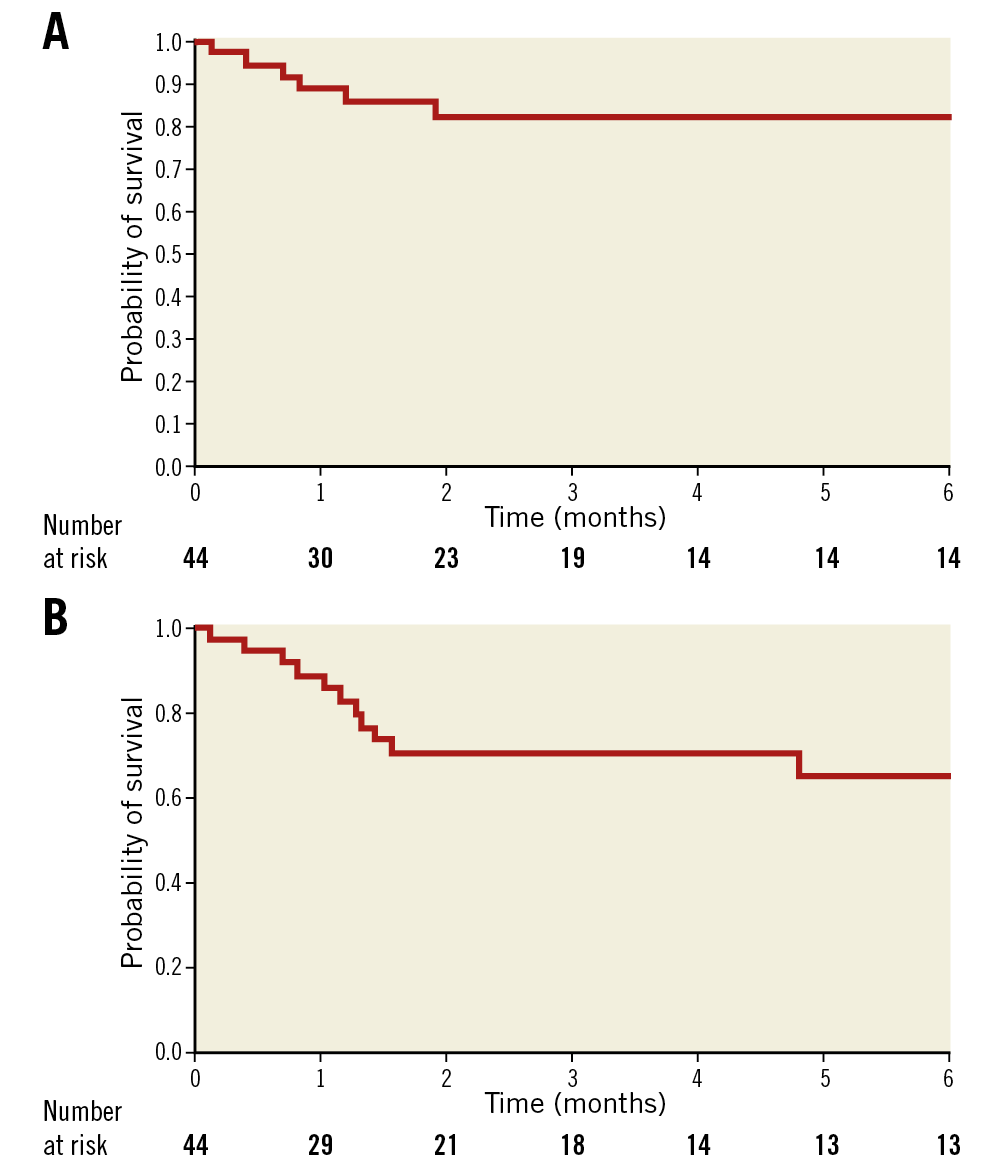
Figure 2. Kaplan-Meier probability of survival free from mortality (A) and major adverse events (MAE) (B).
Discussion
Acute MR after MI is a serious complication that may occur in roughly 3% of cases. Regarding the treatment of this condition (excluding complete papillary muscle rupture), it has been reported that revascularisation by means of primary percutaneous coronary intervention (PCI) can significantly improve the degree of MR and should therefore be the first line of treatment3. However, even after successful percutaneous revascularisation, the degree of MR may worsen, and further treatment may be required. Until recently, cardiac surgery was the only option available for the treatment of such a condition. In a recent review of all published series, the pooled 30-day mortality was 19%, with some of them showing mortalities of around 39%4.
Notwithstanding, in recent years, PMVR has been extensively developed and the MitraClip is the device with the largest experience so far. There are several potential advantages to this therapy. First, there is the rapid decrease in left ventricular (LV), left atrial and pulmonary artery pressures and the increase in cardiac output observed after a successful correction of the MR5 that may lead to a fast recovery. Second is the avoidance of the LV damage induced by the systemic inflammatory response, free radical injury and myocardial oxidative stress associated with cardiopulmonary bypass6. Moreover, the MitraClip may also avert the restraint of the mitral annular motion caused by mitral rings or prosthesis and the development of abnormal septal motion that may negatively impact on LV performance. In addition, acute MR usually develops in a previously normal mitral valve, which usually translates into optimal leaflet tissue and coaptation for device therapy. Furthermore, use of the MitraClip does not preclude delayed cardiac surgery in case the device fails.
Limitations
First, the sample size was small and our results should be interpreted with caution. Second, echo follow-up was not complete. However, our aim was to prove effectiveness in the clinical setting, not to show the positive effects on LV parameters. Third, the procedures were performed at very experienced centres.
Conclusion
In selected patients with acute mitral regurgitation following myocardial infarction, edge-to-edge mitral valve repair with the MitraClip is feasible. Further investigation in this setting may be warranted.
|
Impact on daily practice Acute mitral regurgitation after myocardial infarction is associated with high mortality and morbidity. Treatment with the MitraClip is associated with MR reduction and low 30-day mortality. This represents a valid alternative for selected patients. |
Funding
This work has been supported by a grant from Abbott Vascular.
Conflict of interest statement
R. Estévez-Loureiro, D. Arzamendi, P. Denti, X. Freixa, B. Melica, and L. Nombela-Franco are consultants for Abbott. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.