Abstract
The MitraClip procedure has shown promising results in patients with high surgical risk. However, data concerning outcomes of open mitral valve surgery for failed MitraClip procedures are sparse. In a retrospective clinical investigation, baseline characteristics, intraoperative and histopathological findings, surgical indications and results of patients who required surgery after a failed MitraClip procedure were collected. Between March 2010 and May 2016, 25 patients presented at our department with severe mitral valve regurgitation following a failed MitraClip procedure. Leaflet destruction or severe adhesions between leaflets and the implanted clip were the commonest intraoperative findings. Upon surgery, the mitral valve was either repaired (n=5, 20%) or replaced (n=20, 80%) with a biological prosthesis. Four patients who had presented in cardiogenic shock prior to the operation died within the first 30 days. In the majority of cases, mitral valve replacement is preferred over repair due to severe leaflet damage following the MitraClip procedure. Only those patients who present in cardiogenic shock are at extremely high risk for in-hospital mortality.
Introduction
Surgical mitral valve repair remains the gold standard treatment for patients with mitral regurgitation (MR) due to degenerative disease. Previous studies demonstrated the benefit in outcomes of surgical repair over replacement for this patient group1. For functional mitral regurgitation, the superiority of either repair or replacement remains controversial2.
However, some patients present with a prohibitive risk for surgery due to severe comorbidities such as heart failure, chronic obstructive pulmonary disease or renal failure. In these cases, medical therapy exhibits no benefit. In contrast, the MitraClip® device (Abbott Vascular, Santa Clara, CA, USA) has shown excellent results in reducing the severity of MR with improvement of patient functional outcome and quality of life. However, in about 4.8-9.5% of cases the MitraClip procedure may fail due to inadequate indications, technical problems or unfavourable anatomy3-4. In these cases, the MitraClip has to be removed surgically and the mitral valve either repaired or replaced. To date, only a few case reports and case series have described the outcomes of patients who underwent a surgical mitral valve procedure after a failed MitraClip approach5-6. These current results may have particular importance for patient information prior to the interventional procedure.
Methods
PATIENT DATA SELECTION
Between March 2010 and May 2016, 25 patients with severe mitral valve regurgitation after MitraClip application were referred for surgery. The preoperative data including indication for primary mitral clipping, baseline and echocardiographic data, intraoperative outcomes and histopathological findings were collected for all patients.
SURGICAL PROCEDURE
Median sternotomy or anterolateral thoracotomy was chosen depending on concomitant procedures and the comorbidities of each patient. The anterolateral access was chosen for patients who were scheduled for either isolated mitral valve surgery or additional tricuspid valve repair. Median sternotomy was performed in patients with peripheral vascular diseases, for patients who underwent a concomitant procedure, e.g., coronary artery bypass graft (CABG), aortic valve replacement or who had an emergent indication for surgery. The mitral valve was exposed through the left atrium which was opened directly or through the atrial septum. Valve analysis was performed in each case to examine the possibility of mitral valve repair. Valve replacement was performed in cases of severe leaflet destruction or if the clip harvesting was not possible without extensive resection of leaflets and chords.
FOLLOW-UP
The mortality data were obtained from our local database. Procedural complications were followed up in the hospital or by telephone.
STATISTICS
Continuous variables were presented as means±standard deviation. Categorical variables were expressed as frequency percentages. All data were analysed with SPSS software (version 18 for Windows; SPSS Inc., Chicago, IL, USA).
Results
BASELINE CHARACTERISTICS
Twenty-five patients (age 72±8 years) underwent mitral valve surgery after a failed MitraClip procedure. In all, 11 patients (44%) were female.
INDICATIONS FOR SURGERY
The indication for surgery and the access used are summarised in Table 1. Three patients (12%) underwent anterolateral thoracotomy. Five patients (20%) underwent successful mitral valve repair and 20 patients underwent mitral valve replacement. Five patients (20%) underwent concomitant CABG procedures and nine patients (36%) underwent additional tricuspid valve repair.
SURGICAL TECHNIQUES
The intraoperative findings are summarised in Table 1. Severe leaflet perforation and destruction were the most common causes of mitral insufficiency. In addition, we observed severe adhesions between the clip and the subvalvular apparatus in cases where the initial implantation of the clip had been performed more than two months prior to surgery (Figure 1).
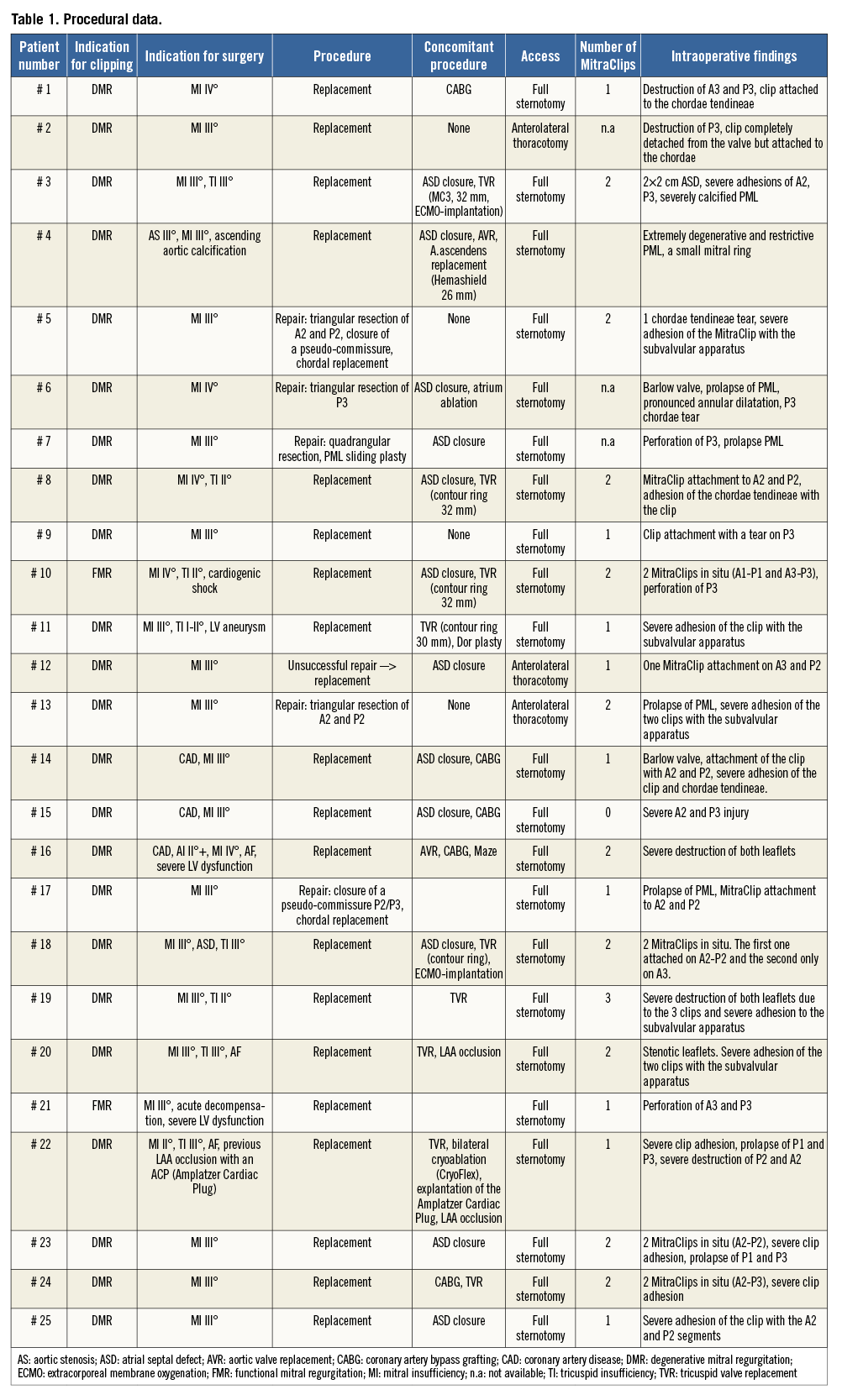
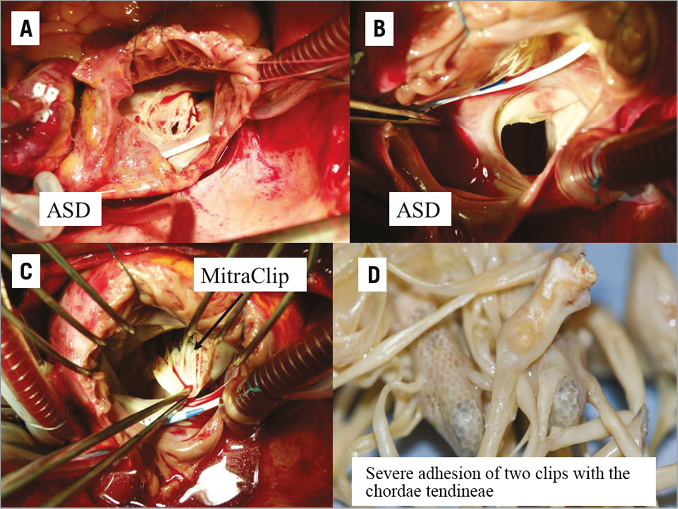
Figure 1. Intraoperative findings: ASD (A & B) and severe adhesion of the clips with the chordae tendineae (C & D). ASD: atrial septal defect
The mechanisms of observed destruction included:
1. Destruction of the leaflets
– injury of the leaflets
– perforation of the leaflets
2. Severe adhesion of the clip with the leaflets
3. Severe adhesion with the subvalvular apparatus and/or chordae tendineae
An atrial septal defect (ASD) closure was undertaken in the majority of these patients.
SURGICAL OUTCOMES
There was no intraoperative death. However, four patients were operated in cardiogenic shock due to severe mitral regurgitation immediately after the clip procedure. Two of these patients died on the first postoperative day due to a low output syndrome which was treated with an extracorporeal membrane oxygenation (ECMO) support. The third patient had developed septicaemia and acute kidney injury with the need for dialysis. This patient died on the fifth postoperative day. All of them presented with a logistic EuroSCORE >30% and severe LV dysfunction. The fourth patient died on the 16th postoperative day. This patient had presented in cardiogenic shock after the failed MitraClip procedure and had been put on intra-aortic balloon pump support immediately after the clip deployment. A fifth patient died two months after surgery. He had presented preoperatively with a high logistic EuroSCORE of 58% and severe LV dysfunction following a previous myocardial infarction with a subsequent anterior wall aneurysm.
Discussion
The most important findings of this study were as follows. 1) The majority of patients undergoing a surgical mitral replacement/repair after a failed MitraClip procedure exhibited low postoperative morbidity and mortality. 2) Emergent cases who presented in cardiogenic shock and severe mitral regurgitation are at extremely high risk for in-hospital mortality. 3) The majority of patients received a valve replacement rather than mitral repair after the failed MitraClip procedure.
Percutaneous mitral valve repair with the MitraClip has been shown to reduce mitral regurgitation and improve symptoms and quality of life in patients at high risk for surgery.
According to the European and American guidelines on the management of valvular heart disease from 2012/20147,8, percutaneous mitral valve repair may be considered in patients with severe degenerative MR who are not candidates for surgical therapy (Class IIb).
In patients with secondary mitral regurgitation, however, experience from a limited number of patients in the EVEREST trials and from observational studies suggests that percutaneous edge-to-edge mitral valve repair is feasible at low procedural risk and may provide short-term improvement in functional condition and LV function9. In the ESC/EACTS guidelines from 2012, the MitraClip procedure is a Class IIb recommendation for patients with secondary MR in the absence of severe tethering8. In contrast, in the American guidelines, there is no recommendation for the interventional treatment of secondary MR7.
In addition, the EVEREST II trial evaluated the safety and efficacy of edge-to-edge percutaneous mitral valve repair using the MitraClip device versus open heart surgery9. The one- and five-year results supported the durability of MR reduction observed after MV clipping and the resulting symptom alleviation. A device implant failure occurred in 9.5% of cases, 6.3% had a single leaflet device attachment (SLDA). Of note, the EVEREST II trial was performed at an earlier moment during the first experiences with this new technology and both the acute procedural success rates and SLDA rates have improved significantly in recently reported registry experiences3,10.
In the current study, we describe the surgical revision in 25 patients after a failed MitraClip procedure. Primarily, the indication for surgery was attributed to severe mitral regurgitation due to single leaflet device attachment, leaflet perforation or severe clip adhesions with the subvalvular apparatus. These intraoperative findings make the operative repair more challenging. In our study, valve repair was possible in five of 25 patients (20%). In previous studies, valve repair had been performed in nine of 33 patients (27.2%)6.
Authors advocating MitraClip therapy reported that the use and subsequent failure of the MitraClip does not preclude later surgical repair11. However, in the current study, we observed severe leaflet injury with remarkable chordal tears and subvalvular apparatus adhesions, which make mitral repair challenging. In addition, the number of implanted clips impacts on the potential repair procedure as stated by Geidel at al12. Deployment of more than two clips to achieve acceptable results may minimise the chance to perform subsequent surgical repair. Hence, the placement of more than two clips should be considered with caution to avoid a potential mitral stenosis or extensive damage. A previous report suggested that the time between clipping and surgery may be decisive for the possibility of performing a successful repair. Argenziano et al reported a successful repair in the majority of patients after the MitraClip procedure when the repair was performed within 18 months after clip implantation5. In the same study, clip detachment (72%) was the most common indication for surgery. Possible explanations for clip detachment could be the substantial tension on the repaired leaflet, which predisposes to leaflet tears and later regurgitation secondary to progressive annular dilatation or valve disruption. The recent study of Geidel et al evaluated predictors of survival after an open mitral valve surgery for a failed mitral clipping in 33 consecutive patients6. In their results, 30-day mortality was 9.1% and predictors of mortality were a EuroSCORE II (p=0.0022), preoperative left ventricular end-diastolic dimension (p=0.0052), left ventricular ejection fraction (p=0.0249), coronary artery disease (p=0.0385) and severe pulmonary hypertension (p=0.0431). The authors concluded that valve replacement is more reasonable than a complex repair6.
In the present study, the postoperative course of the patients who underwent surgical revision after a failed mitral clipping is noteworthy. We observed four early deaths (16%) within the first 30 days postoperatively. Four of these patients presented with a preoperative logistic EuroSCORE of more than 30% and severe LV dysfunction (EF <30%) with preoperative cardiogenic shock. Thus, those patients with severe circulatory compromise prior to the operation are at extremely high risk for postoperative mortality.
In summary, the indication for an edge-to-edge therapy with a MitraClip in patients with severe mitral valve regurgitation should be discussed by a multidisciplinary Heart Team including a cardiologist, a cardiac surgeon and an anaesthesiologist. Suitable candidates for surgery, especially those with degenerative mitral regurgitation, should undergo a surgical repair if the risk is acceptable. Physicians should be aware that a previous MitraClip procedure reduces the probability of valve repair and increases the risk of valve replacement.
LIMITATION
The baseline characteristics of all patients are heterogeneous. Thus we could not make any conclusion with regard to predictors of MitraClip failure. The statistical analysis did not compare outcomes of those who underwent mitral repair versus replacement.
Conclusion
In the majority of cases mitral valve replacement is preferred over repair due to severe leaflet damage following the MitraClip procedure. Patients who present in cardiogenic shock are at high risk for in-hospital mortality.
Conflict of interest statement
The authors have no conflicts of interest to declare.

