Abstract
Aims: The Swiss national registry on percutaneous mitral valve interventions (MitraSwiss) was established in 2011 to monitor safety/efficacy of percutaneous mitral valve repair (PMVR) with the MitraClip device. The aim of this analysis was to report the outcome after PMVR in a real-world, all-comers population and its predictors after inclusion of more than 1,200 patients, stratifying the results according to mitral regurgitation (MR) aetiology. Here we report the in-hospital, short and midterm outcomes of all patients prospectively enrolled.
Methods and results: Since 2011, MitraSwiss has enrolled 1,212 patients with moderate and severe MR of functional (FMR) or degenerative (DMR) aetiology treated with PMVR in 10 centres. Pre-specified endpoints included clinical, echocardiographic and functional parameters with follow-up planned up to five years. Outcomes are compared according to MR aetiology. Acute procedural success was achieved in 91.5% of cases, with no differences between FMR and DMR and sustained good midterm results. NYHA class and pulmonary pressure improved significantly in both cohorts. Cumulative probability of death at five years was 54% (95% CI: 45-63) in FMR and 45% (95% CI: 37-54) in DMR (HR 1.15, p=0.009). Age, anaemia, impaired renal function and reduced left ventricular ejection fraction resulted in being independent predictors of death at five years.
Conclusions: In a large contemporary cohort of non-surgical patients with severe MR, the safety and effectiveness of PMVR have been confirmed. At midterm follow-up, mortality and MACE were lower in DMR patients, though MR aetiology was not directly and independently associated with outcome.
Introduction
With a prevalence of 10% in individuals aged ≥75 years, mitral regurgitation (MR) is the most common valvular disease1,2 with a substantial impact on morbidity and mortality3,4. The gold standard treatment in eligible patients with degenerative MR (DMR) is surgical mitral valve repair, based on its superior long-term results compared to mitral valve replacement or medical therapy5. Nonetheless, an increasing number of patients with severe MR, who have been denied surgical mitral valve interventions in the past6, are currently treated by percutaneous mitral valve repair (PMVR) using the MitraClip® system (Abbott Vascular, Santa Clara, CA, USA), based on the surgical “double-orifice” technique7. Initially tested in selected, low-risk, US patients, predominantly with DMR, PMVR proved to be non-inferior to surgical repair8 in the randomised EVEREST II trial, yielding, however, a higher rate of recurrence in the mid to long term9.
Indications for PMVR expanded to patients at high surgical risk presenting with functional MR (FMR) and it is considered an additional tool in the treatment of chronic heart failure. Regardless of MR aetiology, it has rapidly shown a significant impact on patients’ symptoms and quality of life at short-term/midterm follow-up10,11,12. To support the adoption of PMVR further in the setting of FMR, the MITRA-FR13 and COAPT14 trials were conducted. Surprisingly, despite similar study designs, the two trials reported discordant results, with the first not showing any impact on incidence of death or unplanned hospitalisation for heart failure at one year while the latter demonstrated a survival benefit of PMVR, opening, rather than closing the discussion.
In Switzerland, PMVR has been performed since 2009 and, from November 2011, PMVR patients receiving the MitraClip device have been prospectively included in the national MitraSwiss registry. Follow-up up to five years was planned from its conception.
The aim of this analysis was to report the outcome after PMVR in a real-world, all-comers population and its predictors after inclusion of more than 1,200 patients, stratifying the results according to MR aetiology.
Methods
From September 2011, we aimed to include all patients undergoing PMVR using the MitraClip NT/NTR in a prospective multicentre longitudinal observational study. To date, 10 Swiss centres are actively participating in the registry. Local institutional boards approved the study protocol, and all patients provided consent for treatment and data collection. According to protocol, the case report form was designed at conception of the study and data quality was constantly ascertained by external monitoring.
MitraSwiss enrols elective patients presenting with moderate (3+) or severe (4+) FMR or DMR with indications for percutaneous treatment15,16. DMR was defined as MR secondary to a diseased mitral valve, while FMR was defined as MR secondary to a diseased left ventricle with an anatomically intact valve. Patients were considered for PMVR after Heart Team evaluation had confirmed suitability for a percutaneous approach. Surgical risk was estimated by the European System for Cardiac Operative Risk Evaluation (EuroSCORE and EuroSCORE II), Society of Thoracic Surgeons Risk Model (STS score), and clinical judgement.
According to the registry design, a set of pre-specified clinical endpoints including all-cause mortality, hospitalisations for heart failure and mitral valve surgery due to failure of PMVR or redo PMVR was defined. These were grouped into a major adverse clinical events (MACE) endpoint. Events were reviewed by a blinded clinical events adjudication committee and disagreement solved by consensus. Echocardiographic parameters included left ventricular ejection fraction (LVEF), MR grade, LV volumes and diameters, LA dimension and estimate of pulmonary pressure. NYHA class assessment was recorded in all patients, and six-minute walking tests (6MWT) were performed in suitable patients. The primary endpoint of the present analysis was all cause-mortality at five years, while MACE was set as a secondary endpoint.
Transthoracic echocardiography (TTE) was performed at screening, baseline and follow-up visits and MR graded according to current recommendations17. LV volumes and function (LVEF) were assessed. Left ventricular end-diastolic (LVEDD) and end-systolic diameters (LVESD) and left atrial (LA) dimensions were measured. Systolic pulmonary pressures were estimated from pressure gradients between the right ventricle and the atrium in systole. Transoesophageal echocardiography (TEE) was used during PMVR to guide the procedure and to assess procedural success. The clip implantation procedure has been widely described in detail in previous reports8,9,10,18,19.
Acute procedural success (APS) was defined as placement of one or more clips resulting in a post-interventional MR severity of ≤2+ according to the EVEREST I protocol8.
STATISTICAL ANALYSIS
Data are described as median and 25 th-75th percentiles if continuous, counts and percentages if categorical. Data distribution was assessed graphically with the q-q plot. Given the presence of skewed distribution and/or outliers, non-parametric methods were used. Comparisons between FMR and DMR were performed using Mann-Whitney U and Fisher’s exact tests. Cumulative and event-free survival was described with the Kaplan-Meier estimator. Comparisons were made with Cox regression models, and hazard ratios (HR) and 95% confidence intervals (95% CI) were computed. To adjust for potential confounders, a multivariable model including MR aetiology, age, gender, cardiac function procedure and laboratory findings was fitted. Huber-White robust standard errors were computed to account for clustering within centre. Regression models (linear, logistic or ordinal logistic, depending on the variable) for repeated measures were used to assess changes over time. Robust standard errors were computed to account for intra-patient correlation of measures. Interaction of MR type and time was tested to assess whether FMR and DMR had different behaviours over time. Stata 15.1 (StataCorp, College Station, TX, USA) was used for computation. A two-sided p-value <0.05 was considered statistically significant. As this is a national registry designed to enrol all-comer subjects who underwent MitraClip implant over a long period of time, no sample size was computed a priori. A posteriori calculation showed that the power for the univariable comparison of survival rates between DMR and FMR was 0.87 (with a two-sided alpha of 5%).
Results
PATIENT SAMPLE AND BASELINE CHARACTERISTICS
Between September 2011 and December 2018, 1,265 patients were enrolled. Baseline, procedural and short-term follow-up data completeness was ascertained in 1,212 patients (95.8%). The rate of recruitment per year is shown in Figure 1. Baseline clinical characteristics by MR aetiology are available in Table 1, while Supplementary Figure 1 reports the patient flow. MR was functional in 560 (46.2%) and degenerative in 652 (53.8%) patients. FMR patients were younger, more frequently male, with a higher body mass index (BMI) and higher burden of coronary artery disease than DMR patients. While baseline haemoglobin was equal in FMR and DMR patients, renal function was significantly lower in FMR patients.

Figure 1. Frequency of patient recruitment in the MitraSwiss registry per year (2011-2018).
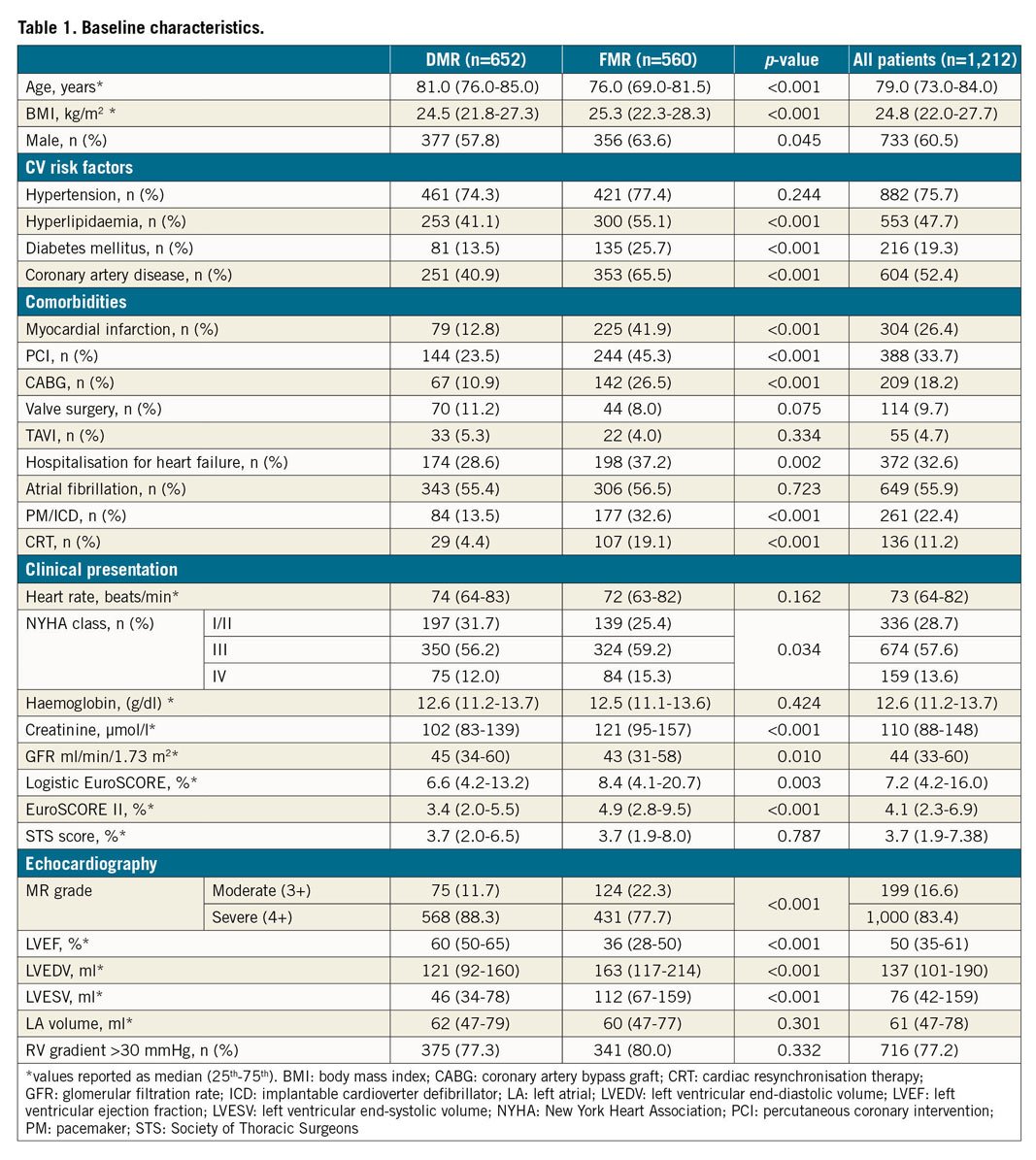
At echocardiography, patients with FMR showed a moderate to severe degree of left ventricular dysfunction, significantly lower than in DMR patients (p<0.001).
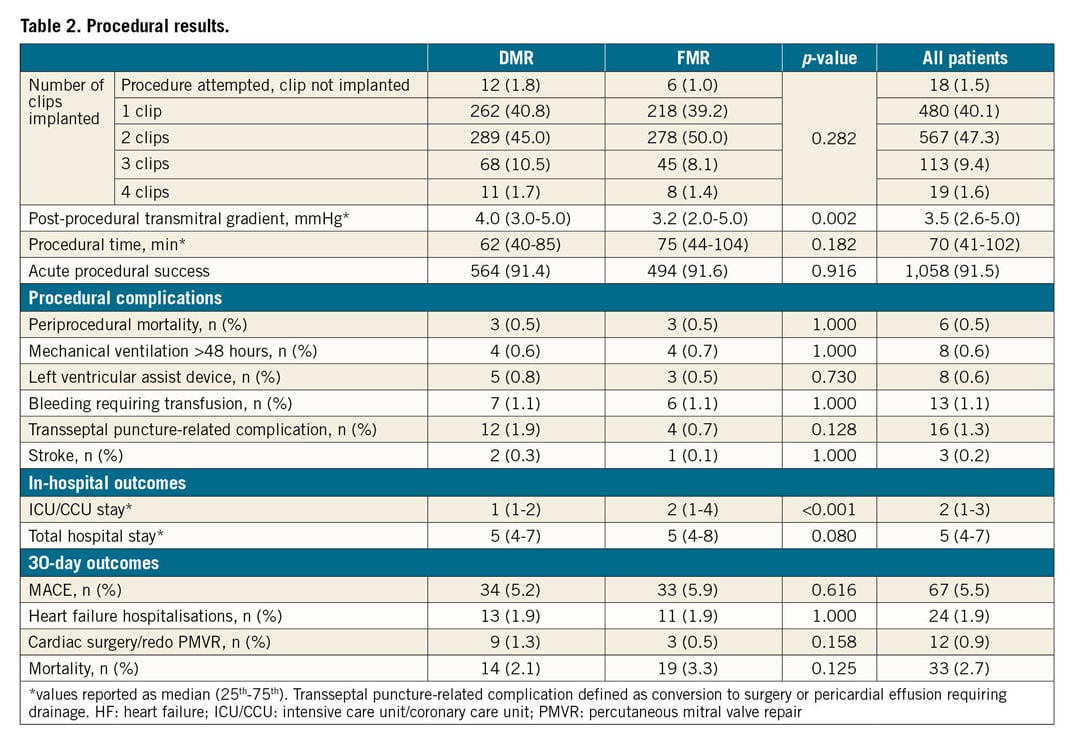
PROCEDURAL RESULTS
Acute procedural success was achieved in 91.5% of cases, without differences between FMR and DMR patients (Table 2). The number of clips implanted per patient did not differ according to aetiology. While no significant differences between FMR and DMR patients within the periprocedural measurements were observed, patients with FMR had a significantly lower median transmitral gradient at discharge (3.2 vs 4.0 mmHg; p=0.002).
IN-HOSPITAL OUTCOMES
Periprocedural death was 0.5% for both DMR and FMR patients (one device-related and five non-device-related deaths). No differences were observed for non-fatal procedure-related complications.
Intensive care unit (ICU)/coronary care unit (CCU) stay was longer for FMR patients (p<0.001), while the length of hospitalisation was comparable among the groups.
MR grade 3+ or 4+ decreased from 99% at baseline to about 18% at discharge. A similar proportion of patients, 64% with FMR and 59% with DMR, was discharged with MR grade 1+.
30-DAY OUTCOMES
Thirty-day mortality was 2.1% (95% CI: 1.2-3.6) in DMR and 3.3% (95% CI: 2.0-5.2; p=0.125) in FMR patients. The rate of mitral surgical intervention/redo PMVR within 30 days was 1.3% (95% CI: 0.6-2.6) and 0.5% (95% CI: 0.1-1.5; p=0.158), rehospitalisation for heart failure occurred in 1.9% (95% CI: 1.0-3.3) and 1.9% (95% CI: 1.0-3.5; p=1.00), respectively. The rate of MACE was 5.2% (95% CI: 3.6-7.2) in DMR and 5.9% (95% CI: 4.0-8.1; p=0.616) in FMR patients.
FUNCTIONAL CHANGES OVER LONG-TERM FOLLOW-UP
As shown in Figure 2 (upper panels), MR grade decreased markedly at discharge and with minimal changes thereafter (p<0.001 for both FMR and DMR); at six months, 50% of the FMR patients and 43% of the DMR patients still had MR grade 1+. Although the rate of MR 3+ and 4+ was slightly higher in DMR than in FMR patients over the entire follow-up, no significant difference was shown (test for interaction p=0.507). A similar behaviour was observed for NYHA class (Figure 2, lower panels), with a marked reduction at discharge and minimal changes thereafter (p<0.001 for both). While more than 70% of patients were in NYHA Class III/IV before treatment in both cohorts, the rate remained consistently below 35%, with no difference between cohorts at follow-up (test for interaction p=0.963). Figure 3 reports changes in echocardiographic parameters over time (additional data in Supplementary Appendix 1).
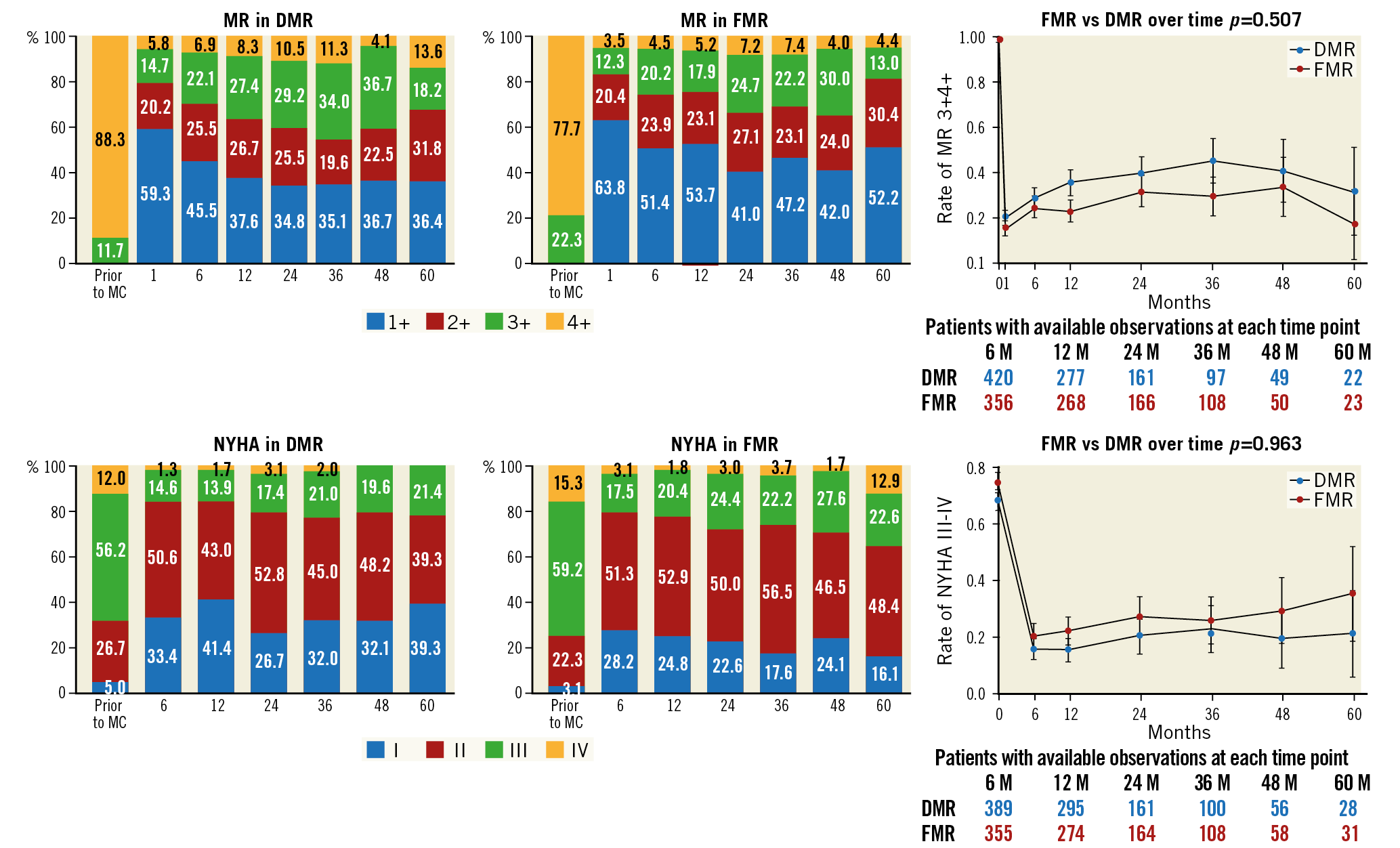
Figure 2. Evolution of MR class and NYHA grade after PMVR at follow-up according to MR aetiology.
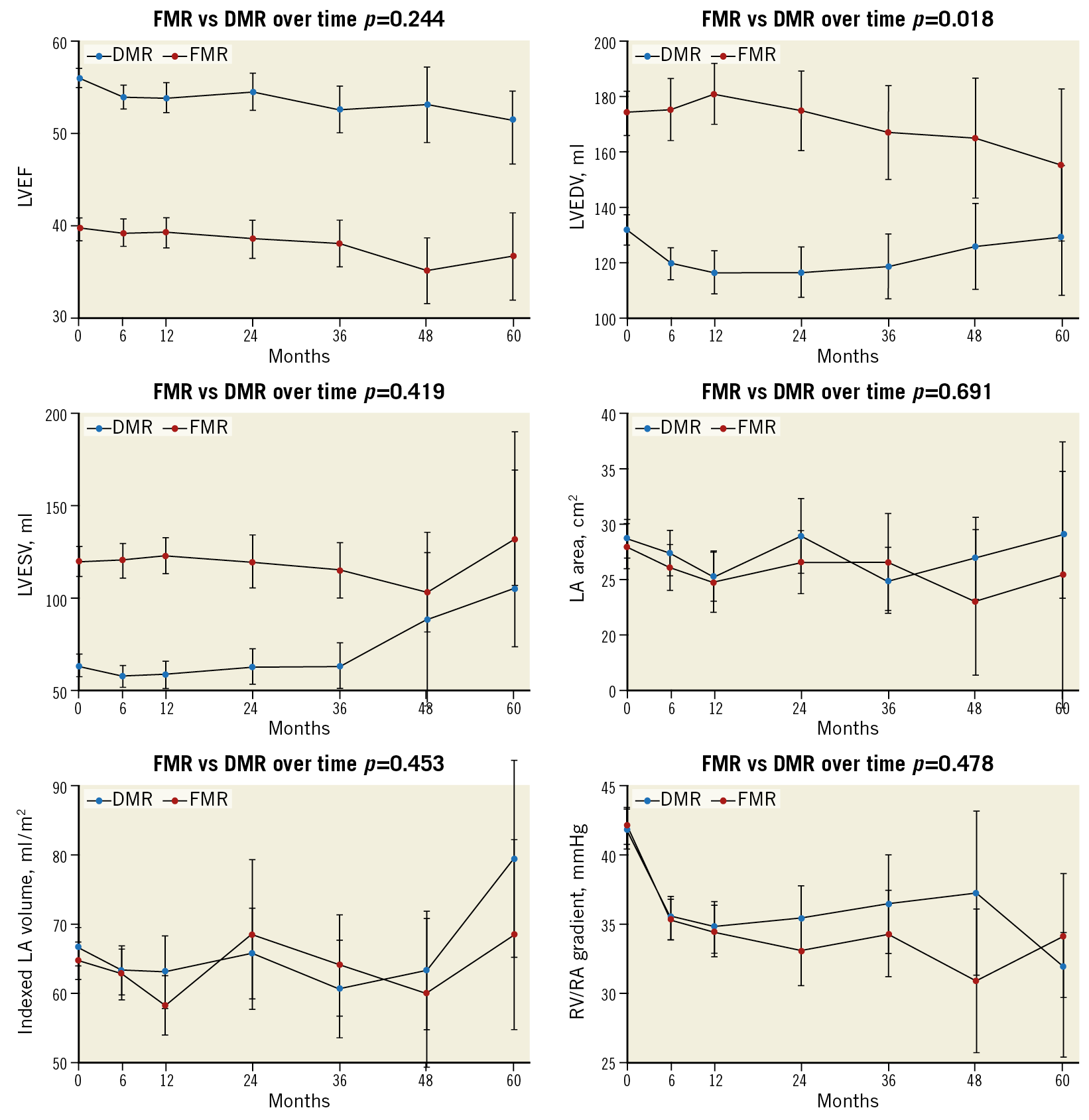
Figure 3. Evolution of echocardiographic parameters at follow-up according to MR aetiology.
CLINICAL FOLLOW-UP
Follow-up was available in 1,153 patients (95.1%) with a median duration of 13 months (25th-75th percentile 6-35). A total of 265 patients died and 310 experienced MACE, corresponding to a cumulative probability of death of 50% (95% CI: 44-57) and MACE of 54% (95% CI: 47-61) at five years.
One hundred and thirty-nine (139) patients died in the FMR cohort and 126 in the DMR cohort, corresponding to a mortality of 18 (95% CI: 15-21) and 15 per 100 person-years (95% CI: 13-18), respectively. The cumulative probability of death at five years was 54% (95% CI: 45-63) in the FMR cohort, and 45% (95% CI: 37-54) in the DMR cohort (p<0.001).
One hundred and sixty-six (166) patients experienced MACE in the FMR cohort and 144 in the DMR cohort. The MACE rate was 25 (95% CI: 21-29) and 20 per 100 person-years (95% CI: 17-23), respectively, and MACE probability at five years was 59% (95% CI: 49-69) and 50% (95% CI: 41-60, p=0.015), respectively.
As shown in Figure 4 and Supplementary Table 1, FMR patients had a 15% excess risk for death and 28% for MACE (HR 1.15, 95% CI: 1.04-1.28; p=0.009, and HR 1.28, 95% CI: 1.05-1.66; p=0.015) versus DMR patients. However, after adjustment in a multivariable Cox model for age, gender, preoperative cardiac function, laboratory and procedural findings, death and MACE excess risk for FMR was not confirmed. Independent predictors of death at five years were age (HR 1.04, 95% CI: 1.02-1.07; p=0.001), lower haemoglobin (HR 0.81, 95% CI: 0.74-0.89; p<0.001), impaired renal function (log creatinine, HR 1.45, 95% CI: 1.10-1.93; p=0.009), and reduced LVEF (HR 0.98, 95% CI: 0.97-0.99; p=0.009). NYHA Class III-IV resulted in being marginally non-significant (HR 1.38, 95% CI: 0.95-1.99; p=0.083). Independent predictors of five-year MACE were lower haemoglobin (HR 0.87, 95% CI: 0.80-0.95; p=0.002) and reduced LVEF (HR 0.97, 95% CI: 0.96-0.98; p<0.001), while NYHA Class III-IV was marginally not significant (HR 1.37, 95% CI: 0.98-1.92; p=0.067).
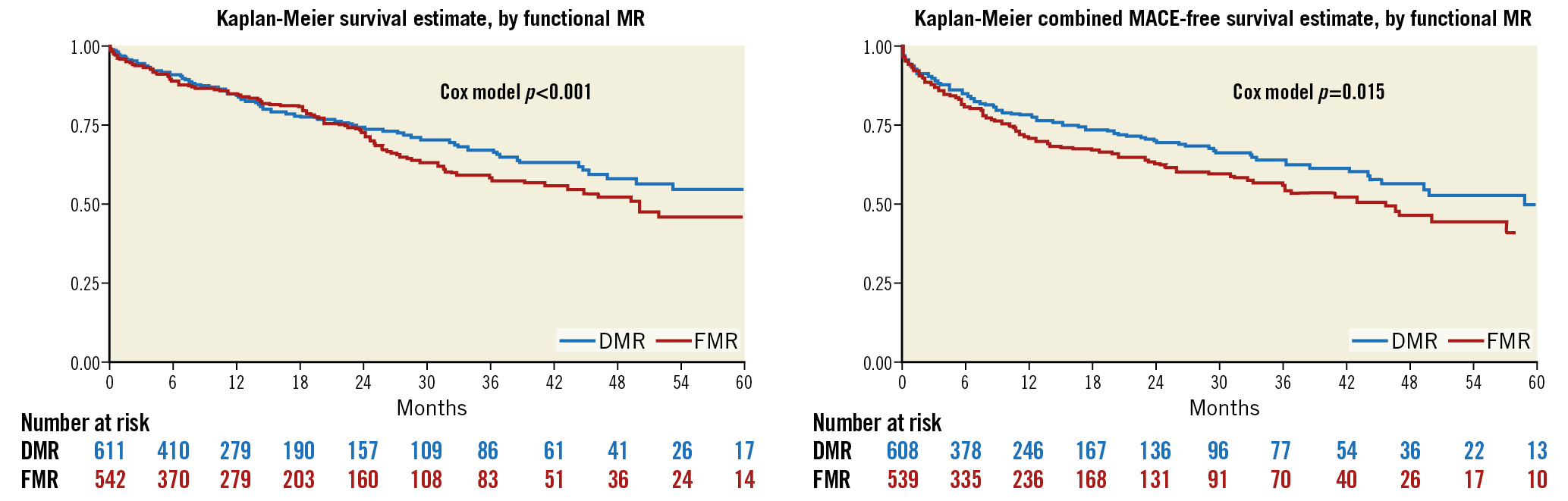
Figure 4. Kaplan-Meier survival estimates for mortality and MACE by MR aetiology.
Discussion
This analysis derived from the MitraSwiss registry is, to the best of our knowledge, the largest prospective cohort of PMVR patients with clinical and echocardiographic midterm follow-up stratified according to MR aetiology.
The main findings are the following. 1) FMR and DMR represent two entities with peculiar characteristics. In our cohort, DMR patients were older but substantially healthier than FMR patients. Conversely, in younger FMR patients, the presence of MR mirrored the valvular involvement of congestive heart failure, a disease with systemic implications. 2) Procedural safety and short-term outcomes are excellent in FMR and DMR patients, with APS exceeding 90% in both groups and a low rate of procedural complications. Reduction of MR is associated with haemodynamic consequences such as a significant and stable decrease of pulmonary pressure with a beneficial impact on symptoms and functional capacity. 3) While midterm outcomes in DMR are different from FMR, MR aetiology per se is not an independent predictor of mortality or MACE, both being driven by markers of systemic involvement such as anaemia and impaired renal function.
So far, only the EVEREST trial and long-term analysis of the TRAMI registry have reported long-term data about safety and efficacy after PMVR with a pooled numerosity well below 1,000 patients. Our data add to this knowledge by confirming previous findings and opening new perspectives.
Overall, the baseline characteristics of MitraSwiss patients are comparable to the TRAMI population in terms of age and sex distribution, while they are significantly older than in the EVEREST trial. Moreover, the distribution between FMR and DMR groups in our registry is well balanced as compared to TRAMI (FMR 69.3%) or EVEREST II (DMR 73%), allowing comparisons between groups to be sustained.
Patients with FMR showed a greater burden of comorbidities with cardiac and systemic implications as compared to those with DMR. Conversely, DMR patients were older, clearly highlighting the intrinsic differences between the functional aetiology (mirroring the mitral involvement in a systemic disease) and the degenerative aetiology, a marker of valvular disease with cardiac, but often without systemic, involvement.
Despite baseline differences, the safety of PMVR was confirmed with the risk of procedural mortality or complications well below 1%, in line with previous reports8,9,11,12,13,14,18,19,20. An extremely low periprocedural (0.5%) and 30-day (2.7%) mortality, and a low rate of periprocedural complications, and immediate and deferred surgical conversion were observed.
Efficacy was confirmed, with APS of >90%, in line with TRAMI registry data19. The beneficial effect at midterm follow-up and the functional benefit of PMVR, as demonstrated by the improvement in the NYHA class and 6MWT and by the reduction in pulmonary pressure, were maintained in both groups. A relative decrease in LVEF, already evident in the EVEREST II21 population was seen in our DMR patients, associated with an increase in left ventricular end-systolic volume (LVESV). This finding is probably justified by a significant reduction in left ventricular preload and increased afterload after MR reduction22.
It is well known from real-time left ventricular pressure-volume loops recorded during PMVR that an improvement in haemodynamics after PMVR results in reverse LV remodelling by reducing LV preload while preserving contractility23.
Overall five-year mortality was 50%, comparable to TRAMI (53.8% at four years)23 but significantly higher than in the EVEREST II trial (32%)18, confirming the clinical significance of MR as a marker of poor long-term prognosis in a real-life scenario. Interestingly, five-year mortality in our cohort is in line with that observed in patients with congestive heart failure24, further supporting the concept that MR is just one aspect of a more complex picture. Of note, despite an older age and its independent association with outcome, the five-year survival of DMR patients was significantly higher than in FMR patients, pointing up once more the intrinsic differences between the two aetiologies.
Concerning prognostic factors associated with outcome, our data do not support previous findings derived from the EVEREST II trial in which functional aetiology was independently associated with long-term mortality together with chronic obstructive pulmonary disease (COPD), diabetes, peripheral artery disease and age. In line with TRAMI and the Spanish MitraClip registry, aetiology did not show any prognostic role25. In our population, independent predictors of five-year mortality and MACE substantially reflect the clinical conditions at the time of repair, which are ultimately among the factors that led to the decision to prefer PMVR over surgery. Interestingly, a good procedural result, which predicted one-year and two-year mortality26, lost its significance in our population at a longer follow-up, as observed in other cohorts18,19. This might be justified as a hierarchical role of age, anaemia or renal impairment resulting in their being determinants of long-term prognosis, nonetheless with a minor impact on short-term outcomes.
Obviously, our data do not add adjunctive evidence to solve the debate derived from the publication of the MITRA-FR and COAPT trials. While confirming the benefit in terms of symptoms, the MITRA-FR study failed to show any impact on survival in advanced disease13. In patients at an earlier disease stage, with more pronounced MR and a less dilated LV, an impressive benefit over medical treatment was seen in the COAPT trial14, leaving open the question as to which patient with FMR should be selected for PMVR. Concerning the nature of our registry data, the lack of a comparator does not allow us to draw any conclusion about the prognostic impact of PMVR. Reassuringly, the median left ventricular end-diastolic volume (LVEDV) in our FMR population is 163 ml, indicating patients with clinically significant MR but smaller ventricles when compared to the MITRA-FR and COAPT trials. This places our FMR population in the newly defined group of “disproportionate” or “tertiary” mitral regurgitation27,28, in which the amount of MR exceeds the degree of left ventricular dysfunction, a class of patients in which PMVR proved to reduce the risk of death and hospitalisation for heart failure according to the COAPT results14.
Limitations
Data are derived from an observational registry, thus intrinsic inaccuracies in the data set apply. Moreover, as a limitation of all dynamic cohorts, five-year follow-up is available only for a limited percentage of patients. Although a critical events committee reviewed all events at 30 days, the risk of under-reporting of later events remains. While clinical and echocardiographic follow-up was a condition required in this registry, representing a unique feature of the present analysis, echocardiographic data were site-reported and not core lab adjudicated. Finally, no data are available regarding the evolution of medical treatment over time.
Conclusions
Our data confirm the midterm safety and efficacy of PMVR using the MitraClip system in an all-comers population. Treatment leads to significant reduction of MR and to several significant clinical and functional benefits in a high proportion of the patients. Although patients with DMR and FMR are intrinsically distinct populations, short-term outcomes do not differ. Mortality and MACE are lower at midterm follow-up in DMR patients; nonetheless, the aetiology of MR is not associated with outcome.
|
Impact on daily practice PMVR with the MitraClip is a valuable therapeutic option both in FMR and in DMR patients not suitable for surgery and is able to provide symptomatic benefit and functional improvements. Midterm outcomes are worse in FMR than in DMR patients. Nonetheless, MR aetiology is not associated with five-year mortality, while significant associations were evident with markers of systemic involvement such as anaemia, renal impairment and left ventricular ejection fraction, highlighting the clinical and prognostic interdependence between MR and congestive heart failure. |
Appendix. Study collaborators
Moreno Curti, MD; Service of Clinical Epidemiology & Biometry, Policlinico San Matteo, Pavia, Italy. Igal Moarof, MD; Division of Cardiology, Kantonsspital Aarau, Aarau, Switzerland. Olivier Muller, MD; Division of Cardiology, Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland.
Funding
The MitraSwiss registry is an investigator-initiated multicentre registry. Funding is provided by the Swiss Society of Cardiology and unrestricted grants from Abbott.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.