n this issue of EuroIntervention, Sürder et al report the outcomes of percutaneous mitral valve repair (PMVR) by means of the MitraClip® (Abbott Vascular, Santa Clara, CA, USA) within the Swiss national registry1.
Outcomes were compared according to mitral regurgitation (MR) aetiology – 652 (53.8%) primary (degenerative) versus 560 (46.2%) secondary (functional) MR patients. Acute procedural success was similar in the two groups (>90%). Although the five-year cumulative probabilities of death and major adverse clinical events (MACE) were significantly higher in secondary MR, only age, haemoglobin level, creatinine level, and left ventricular ejection fraction (LVEF%) were independent predictors of death/MACE. The authors conclude that MR aetiology is not directly and independently associated with outcomes.
There are many lessons we can derive from the Swiss and from other national and supranational PMVR registries.
1. The Swiss registry investigators have confirmed that, at this stage, we are able to repair, percutaneously and by means of the MitraClip, both primary and secondary MR.
The investigators have presented only the final results of a long decisional process that started at the time of referral for treatment, and possibly even before, involving multiple actors and institutions. This process, that sees the interventionist as one of the many professionals involved, has evolved over the years (since 2011 in this case) and has included, in due time, updated clinical notions and technological improvements. From the present report we cannot derive the structure of the treatment selection criteria, the importance of the institutional cumulative experience, and the institutional learning curves. Although this extraordinary organisational effort has resulted in a large amount of information, making causal inferences starting from observational data can be even more challenging.
2. Primary MR and secondary MR are two completely different entities. The “regurgitation of blood through the leaking valve” is just the same epiphenomenon of two different and complex aetiopathogenic processes. Although it is very satisfying to see that acutely we can repair both types of MR using the same technology (i.e., MitraClip) and with the same efficacy, it may be out of place to investigate follow-up outcome differences between primary and secondary MR. In the surgical arena, it is widely accepted that surgical treatment of those two entities will lead to different follow-up results and, as a matter of fact, follow-up outcomes are hardly compared. Although some analytical strategies can trick us into believing that adjustments can be made so as to compare “almost similar patients with different clinical conditions”, this is not always the case. Moreover, variables concerning cardiac function and ventricular geometry are highly correlated with one another and with the occurrence of secondary MR. In fact, secondary MR is a systemic disease of cardiac origin where ventricular dilatation and cardiac dysfunction are actually part of the very same definition of secondary MR. As a result of this multicollinearity, the effect of each correlated variable on any regression model becomes less precise and difficult to establish, whenever those variables are inserted simultaneously within the same regression model.
3. The Swiss registry confirms that long-term follow-up mortality and adverse event rates after PMVR are not negligible, even within the premises of a well-structured healthcare system.
The actual time frame in which most of the subjects have had the defined event or have remained under observation is where the Kaplan-Meier estimates are most reliable. A short median follow-up time (in this case 13 months) will impact upon the stability of the Kaplan-Meier estimates on long-term follow-up, especially when only a small number of subjects have reached the desired follow-up duration (in this case five years). Moreover, any regression analysis that includes time-dependent variables, such as MR degree and recurrence of MR, will be greatly impacted by follow-up duration.
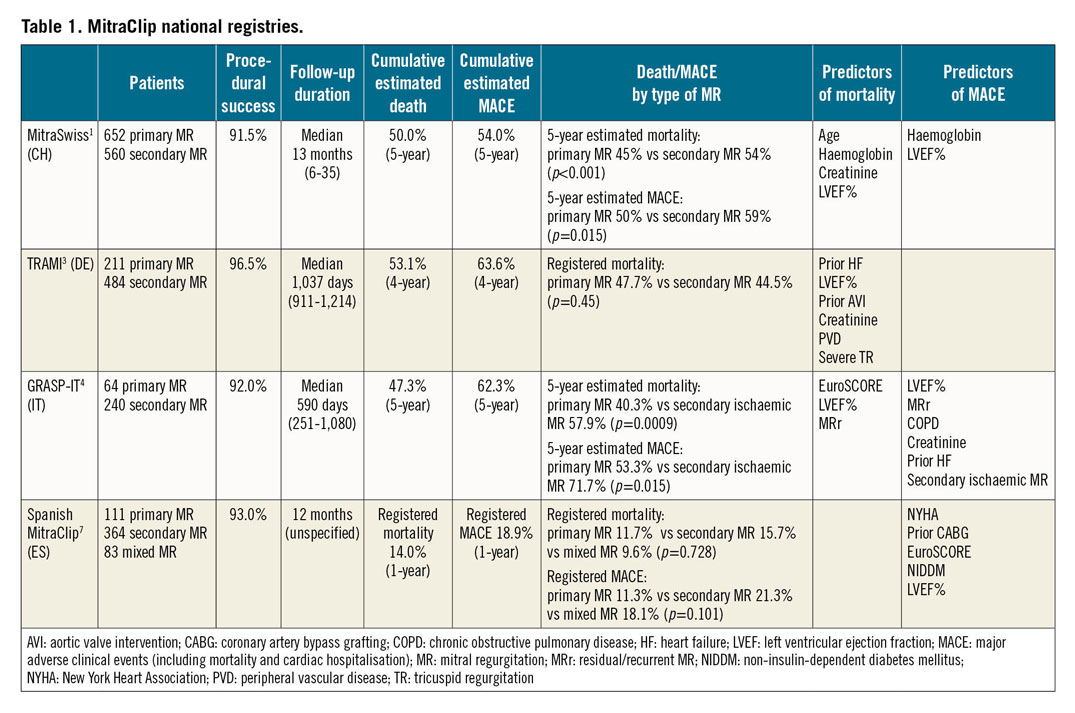
4. We should be cautious before concluding that MR aetiology does not impact upon long-term outcomes of PMVR. Differences in terms of one-year outcomes after PMVR in patients with primary and secondary MR have been investigated in a meta-analysis including nine studies and 2,615 patients2. At the time of referral, patients with secondary MR were significantly more symptomatic and had a more severe degree of MR accompanied by a severe reduction of cardiac function and derangement of ventricular geometries2. Although at follow-up the one-year mortality rate was not different between the two groups (primary MR 14% vs secondary MR 18%; p=0.18), the secondary MR group had a significantly higher rate of patients in New York Heart Association (NYHA) Class III/IV (16% vs 8%; p<0.01) and a higher rate of re-hospitalisation for heart failure (HF) (23% vs 14%; p=0.03)2. More recently, five-year follow-up outcomes of PMVR have been investigated in other national registries (Table 1),3,4. The German TRAMI registry has shown no differences in terms of four-year follow-up outcomes in patients categorised by MR aetiology3. Variables correlated with secondary MR, such as prior HF episodes and LVEF% <30% were predictive of long-term mortality3. In the Italian GRASP-IT registry, the estimated rates of mortality and MACE had a significantly different distribution according to MR aetiology and were significantly higher among patients with ischaemic secondary MR4. A multivariable model tested for collinearity of variables confirmed that LVEF% <30% was associated with all-cause mortality. Furthermore, ischaemic aetiology of secondary MR, prior HF episodes, and LVEF% <30% were among the five-year composite endpoint predictors4.
5. We should ponder rationally about the impact of residual/recurrent MR. In the Swiss registry even a post-PMVR residual/recurrent MR III-IV did not seem to impact on follow-up outcomes. With a median follow-up of 13 months, the effects of residual/recurrent MR possibly did not have time to manifest themselves. Moreover, considering the high mortality in these patients, the true incidence of recurrent MR and its consequent impact may be obscured. In the GRASP-IT registry, recurrent MR within two years (time-based MR evaluation) was associated with a significantly increased relative risk of five-year mortality and MACE4. A previous report of the US TVT registry including 2,952 patients (94.8% primary MR) has documented that residual MR greater than grade II is independently associated with one-year mortality and re-hospitalisation5.
6. The Swiss registry documents an increase in primary MR patients referred for PMVR and a 40% rate of MR III-IV at 24 months after PMVR for primary MR1. These rates should be reinterpreted in light of the complexity of the treated pathology and the single-centre experiences5. In our personal institutional experience that includes over 1,000 PMVR procedures, we are also witnessing a progressive change in the referral pattern that now includes patients with more advanced and generalised cardiac involvement and even more complex structural mitral valve pathologies, ranging from fibroelastic deficiency to diffuse myxomatous disease.
The different phenotypes of primary MR include different degrees of pathological involvement of the MV leaflets, the subvalvular apparatus and the MV annulus, and, for this reason, require escalating degrees of surgical and percutaneous skills. Annular involvement in primary MR, and especially in diffuse myxomatous disease, is intrinsic to the degenerative disease of the annular tissue. Differently from secondary ischaemic MR where the MV annulus is mainly enlarged in its anteroposterior geometry, primary MR, and particularly myxomatous disease, results in a marked intercommissural annular enlargement6.
Primary MR is not a homogenous pathology. For this reason, we must adopt a structured and experience-based selection and treatment strategy, as we navigate from fibroelastic deficiency to diffuse myxomatous disease. The “natural evolution” in the referral pattern may impact not only upon the pathology we treat but also upon the results we achieve.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.