Abstract
Aims: The European Association of Percutaneous Coronary Interventions (EAPCI) assessed the current status of transcatheter valve therapy in Europe through a web-based survey. Our aim here was to report the results of that survey regarding trends in percutaneous mitral valve repair (PMVR) therapy.
Methods and results: Among 301 European centres participating in the overall EAPCI survey, 246 (81.7%) responded to the PMVR section questions. A total of 176 (71.5%) have been undertaking a PMVR programme. Among responding centres (n=129), 58.1%, 15.5% and 26.4% performed ≤10, >10-40 and >40 PMVR procedures, respectively, in 2014. The majority of centres performing >40 PMVR procedures in 2014 were in Germany (82.4%). MitraClip was the most commonly performed technique (used in 91.8% of centres) followed by the valve-in-ring or valve-in-valve for failed surgical prostheses using transcatheter aortic valve devices (41.5%). Of those centres not performing PMVR (n=70), 41.4% were not considering initiating a programme, mostly for economic reasons (69.0%), or because of limited data available (20.7%) or no interest (10.3%).
Conclusions: The second part of this EAPCI survey documents the limited PMVR penetration in Europe, despite an increasing interest. Possible reasons for this include economic, regulatory and logistic issues, challenging techniques, along with a lack of compelling studies and clear indications.
Introduction
There is widespread interest in percutaneous therapy for valvular heart disease, which is expected to have an exponential increase in the near future. Both transcatheter aortic valve implantation (TAVI) and percutaneous mitral valve repair (PMVR) were launched in Europe a few years ago, the latter in 2008.
While the latest European Society of Cardiology Guidelines on Valvular Heart Disease and, more recently, the American ones1,2 recognised TAVI as safe and effective in inoperable and high surgical risk patients, implantation of the MitraClip® (Abbott Vascular, Santa Clara, CA, USA), the most frequently used device for PMVR procedures, received very limited indications, mainly for degenerative valve disease (class IIb recommendation).
A few months ago, the European Association of Percutaneous Coronary Interventions (EAPCI) evaluated the current status of percutaneous valve therapy in Europe through a web-based survey, with the results focusing on TAVI being published recently3. The present paper will examine the second part of the EAPCI survey concerning the section on PMVR.
Methods
The sample population comprised a list of interventional European centres performing structural valve procedures, obtained through intersecting information from each National Society or Working group in Interventional Cardiology, from each National TAVI Registry and from the mailing list of EuroIntervention, the official journal of the EAPCI. Overall, 490 centres were invited to participate. The survey was carried out between November 2015 and January 2016.
The methodology of the questionnaire has already been described in a previous paper3. The questionnaire was divided into two sections with a total of 39 questions. The PMVR section was shorter and built with nine questions concerning centre organisation and PMVR programme, and aimed to investigate the willingness to increase or initiate any mitral valve percutaneous procedure.
The questionnaire was drafted by the EAPCI Database and Registry Committee and subsequently approved by the EAPCI Board. The survey was undertaken using a free web-based survey tool (SurveyMonkey, Palo Alto, CA, USA) and comprised multiple-choice questions, including the possibility to add comments if required. It was mandatory to reply to the entire survey. The survey could be filled in anonymously, but each centre had the opportunity to provide its address in order to receive a summary of the information collected after completion of the survey.
The results were reported as descriptive statistics.
Results
CENTRE DESCRIPTION
A total of 301 (61.4%) European centres performing TAVI participated in the EAPCI survey, of which 246 (81.7%) completed fully or partially the section regarding PMVR. Individuals (n=246) who responded to the PMVR section were: 223 (90.6%) interventional cardiologists, 15 (6.1%) cardiac surgeons, and eight (3.3%) clinical cardiologists. Among the participanting centres (n=246), 126 (51.2%) were university hospitals, 84 (34.1%) were community hospitals and 36 (14.6%) were private hospitals.
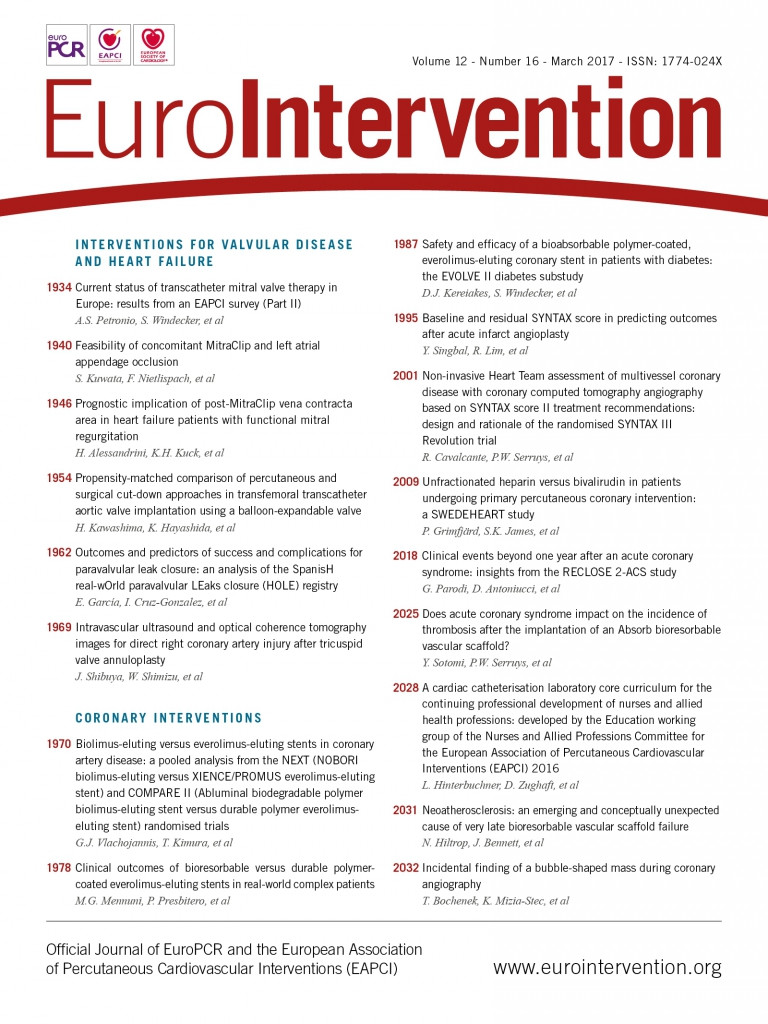
A total of 176 centres (71.5%) were running a PMVR programme (Figure 1). The European country distribution of the 246 responding centres and of those centres already performing PMVR is represented in Table 1. Among responding centres (n=129), the number of PMVR procedures performed in 2014 was less than 10, >10-40 or more than 40, in 58.1%, 15.5%, and 26.4%, respectively (Figure 2). The majority of centres that performed more than 40 PMVR procedures in 2014 were from Germany (n=28, 82.4%); the remaining centres were from Italy (n=3), Switzerland (n=2) and France (n=1) (Figure 3). Centres not running a PMVR programme often had a limited experience with TAVI, having performed fewer than 200 TAVI at the time of the survey in 71.4% of cases, compared with 11.1% and 8.8% among centres performing >10 PMVR and >40 PMVR, respectively. Among centres having performed at least 500 TAVI procedures, 89.8% also had a PMVR programme. Moreover, the 16% of centres performing PMVR had started a TAVI programme before or in 2007, while no centres without a PMVR programme had started to perform TAVI before 2007, and 97.1% had started after or in 2008.
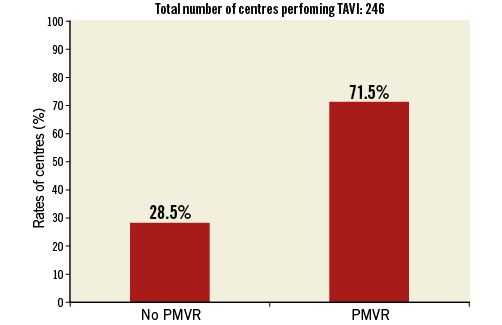
Figure 1. Rates of transcatheter aortic valve implantation (TAVI) centres (n=246) also performing percutaneous mitral valve repair procedures (PMVR).
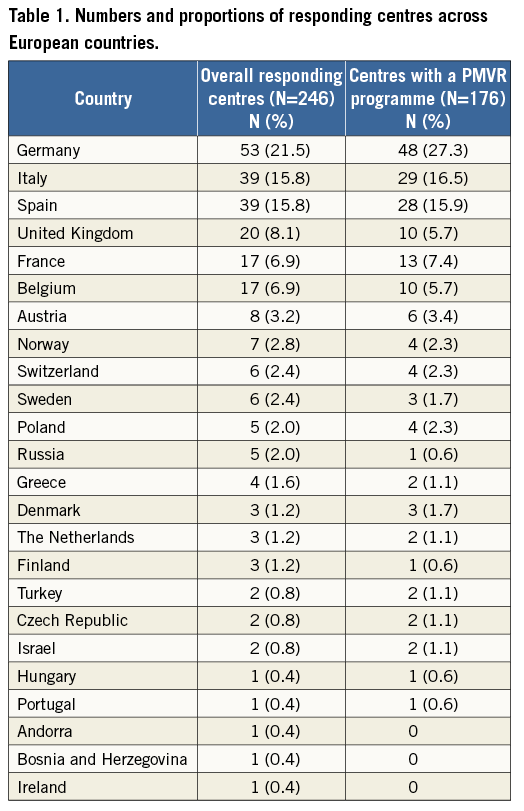
Figure 2. Rates of centres performing ≤10, 10-40 and >40 percutaneous mitral valve repair (PMVR) procedures during one year (2014). The 176 centres with a PMVR programme are distributed according to the number of procedures performed.
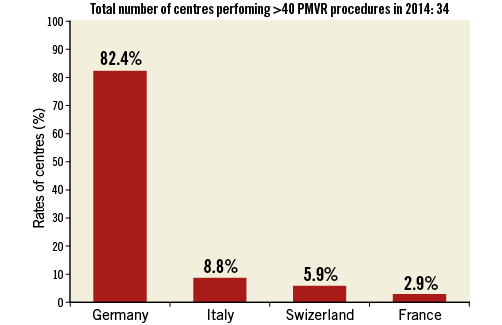
Figure 3. Country distribution of centres (n=34) performing >40 PMVR procedures in 2014.
The majority (88.6%) of centres already performing PMVR therapy were planning to increase the number and variety of transcatheter mitral procedures in the next year.
Of those centres not performing PMVR (n=70), 29 (41.4%) were not considering initiating transcatheter procedures for the mitral valve within the next 12 months, mostly due to economic constraints (69.0%), or because they considered the available scientific evidence still too limited (20.7%), or because they were not interested (10.3%) (Figure 4). All these 29 centres had performed fewer than 300 TAVI at the time of the survey, 82.8% of them having performed fewer than 200 TAVI procedures.
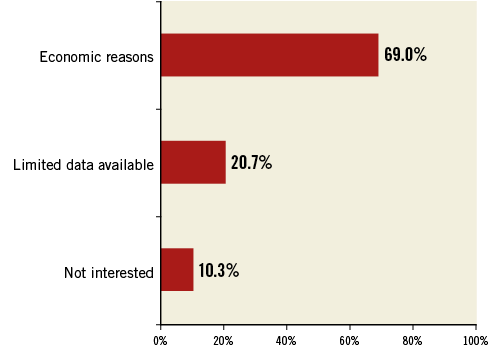
Figure 4. Proportions of reasons for not planning to start a percutaneous mitral valve repair programme among 29 centres.
Among centres providing a response to the specific question (n=193), the numbers of surgical mitral procedures performed in 2014 were ≤100 in 138 centres (71.5%), between 100 and 200 in 37 centres (19.2%), and >200 in 18 centres (9.3%), of which 98/138 (71.0%), 28/37 (75.7%) and 14/18 (77.8%), respectively, also had a PMVR programme.
PMVR ORGANISATION PROGRAMME
Among the 176 centres running a PMVR programme, the head of the PMVR programme was the interventional cardiologist in 108 (61.4%), the cardiac surgeon in nine (5.1%), and both in 59 (33.5%).
Among the 225 centres providing a response to the specific question, patients with mitral regurgitation were referred by the clinical cardiologist in 96.9% (n=218), the heart failure specialist in 64.9% (n=146), the cardiac surgeon in 53.8% (n=121), the heart transplant specialist in 16% (n=36), and the general practitioner in 6.2% (n=14).
Among the 195 centres already performing or planning to start PMVR procedures, the choice of the PMVR technique is represented in Figure 5, with MitraClip being the preferred percutaneous therapy (in 91.8% of centres) followed by the valve-in-ring or valve-in-valve for failed surgical prostheses using transcatheter aortic valve devices. Percutaneous treatment was considered for primary and secondary mitral regurgitation in 34.1% and 65.9%, respectively.
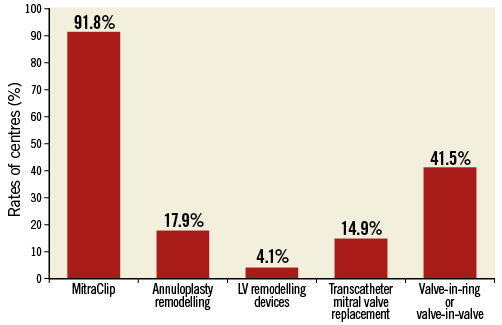
Figure 5. Rates of centres performing each different type of percutaneous mitral valve repair (PMVR) procedure.
Most centres (90.3%) performed all the screening imaging procedures internally, while the remaining centres evaluated the images provided by referring physicians.
Discussion
TRENDS IN TRANSCATHETER MITRAL VALVE THERAPY
The section of the EAPCI survey concerning mitral percutaneous procedures in Europe showed the following main findings: 1) almost 30% of centres performing TAVI have no PMVR programme; 2) one third of those centres without a PMVR programme are not planning to start one, mainly for reimbursement reasons (69%); 3) the majority of centres with a PMVR programme have performed fewer than 40 procedures in 2014 (74%), with more than half (58%) having performed fewer than 10 procedures in one year; 4) the vast majority of centres (82%) with more than 40 PMVR procedures performed were from only one country (Germany).
Despite the fact that mitral regurgitation is a frequent valve pathology among the European population and a significant proportion of patients is not treated by surgery4,5, the present survey findings show that the penetration of PMVR across Europe can be considered marginal and not comparable to that of TAVI, which on the contrary has been progressively expanded also to intermediate- and low-risk patients6-8. There are several possible explanations for this trend of PMVR procedures, including economic, regulatory and logistic issues, challenging techniques due to the more complex nature of the mitral valve treatment, along with the lack of compelling studies and clear indications.
An interesting finding of the present survey is that there seems to be a relation between the extent of the TAVI experience and the coexistence of a PMVR programme, as the majority of centres (71%) without a PMVR also had a limited experience with TAVI (<200 procedures performed in total), while centres with low TAVI volume were less represented among those performing PMVR procedures (11% and 9% of those performing >10 or >40 PMVR procedures, respectively). On the other hand, it is notable that about 10% of the centres with a high TAVI volume (>500 procedures performed in total) had not started a PMVR programme.
Another important insight on the current European status of PMVR highlighted by the survey is the suggestion of a probable relation between PMVR activity and the existing local reimbursement policy. Indeed, centres with >40 procedures/year were mostly from Germany (82.4%), followed by a few centres in other countries with special local reimbursement policies, and by a few research or private centres. Most European countries recognise PMVR programmes as special niche programmes. The feeling that the growth of these procedures is held back by economic factors is demonstrated by country distribution, and by the answers to the following question: “If a transcatheter mitral program does not currently exist, do you consider to initiate a program within the next 12 months?”. Although the majority were willing to begin one, 41.4% answered negatively because of reimbursement reasons (69%), while only 20.7% considered the available scientific evidence on PMVR insufficient. Interestingly, centres which already had an ongoing programme declared an interest in increasing their activity and expanding it to new emerging techniques.
Finally, the survey showed no apparent relationship between the number of mitral valves treated with surgery and the presence of a PMVR programme, as the proportions of centres undertaking a PMVR programme were similar regardless of the number of surgical procedures performed. In addition, the concomitant low rate (9.3%) of centres reporting >200 surgical mitral procedures performed per year suggests that a diffuse invasive undertreatment of mitral regurgitation still persists.
MITRAL PROGRAMME CHARACTERISTICS
Interventional cardiologists mainly coordinate PMVR programmes, but a significant involvement of cardiac surgeons was observed (38.6%).
The clinical cardiologist and the heart failure specialist are the main referral sources for PMVR patients (96% and 64.9%, respectively). This information reflects the aetiology of mitral regurgitation (MR) referred for PMVR, being functional MR (FMR) in 65.9% of patients. This is consistent with what is already known from several European registries and multicentre experiences9-12. Interestingly, European guidelines indicate PMVR for degenerative MR (DMR) as possible and safe, but less effective than surgery, and restrict the percutaneous treatment of DMR and FMR to inoperable or high surgical risk patients (class IIb, level of evidence C), according to the EVEREST results13, underlining the need for more evidence, especially for FMR that lacks randomised trials1. On the other hand, the interventional community seems to rely on the more recent literature on FMR10,11,14, underlining the need for an update of current guidelines.
Currently, PMVR programmes in Europe consist mostly of repair techniques, especially the edge-to-edge technique, which is the most commonly used (performed in 92% of centres), but the use of annuloplasty remodelling devices in 18% of the centres is also notable, showing a current increasing interest in this different percutaneous valve repair approach. On the other hand, percutaneous mitral replacement is still limited to valve-in-valve or valve-in-ring procedures for patients with dysfunction of surgical mitral prostheses or annuloplasty rings (performed in 41% of centres), while percutaneous mitral replacement with dedicated devices is limited to fewer than 15% of centres. This limitation is due to the fact that new mitral prostheses are still investigational, although they receive great interest, and mitral valve replacement is still rarely and selectively performed, mainly with aortic devices in centres with high experience in structural valve procedures. The question whether repair or replacement will have a similar indication to surgery needs more years of experience before being answered, as mitral intervention is far more complex than aortic intervention.
Finally, almost all centres are still performing all the screening imaging techniques in-house, showing that they do not rely on referring hospitals. This highlights the need for further education and involvement of referring cardiologists in patient selection for PMVR.
Limitations
This survey has important limitations, which should be taken into account when interpreting the results. First of all, not all the invited centres responded to the PMVR section, barely reaching the majority (50.2%). Therefore, the results are only partially representative of the whole European community. Moreover, although the survey meant to address the practice of each centre in its complexity, we had to rely on one responder as the representative of the whole structural intervention team. Moreover, the PMVR section had a smaller number of questions than the TAVI section, and was designed to investigate only the principal aspects of the status of this therapy.
Conclusions
The section of the EAPCI survey dedicated to PMVR therapy demonstrated its still limited penetration in Europe, despite the increase of interest in these new therapies. Possible reasons for the slow increase of PMVR procedures include economic, regulatory and logistic issues, challenging techniques, along with the lack of large, high-quality studies and clear indications, especially on FMR. Although, at the moment, there is only one predominant PMVR technique, newer procedures and devices are already on the way, underlining that PMVR is definitely a more complex therapy as compared to TAVI.
| Impact on daily practice PMVR treatment across the European community has demonstrated a slow and limited penetration, unlike transcatheter aortic valve implantation procedures. However, an increasing interest in PMVR techniques has emerged from the survey. This suggests that efforts should be made to overcome the limitations hampering the implementation of PMVR procedures in clinical practice. |
Acknowledgements
The authors would like to express their gratitude to the staff of Europa Organisation/EuroPCR for the support given during survey planning and conduct. Moreover, the authors would like to thank the European Presidents of National Societies and Working Groups of Interventional Cardiology for providing contacts at each centre.
Conflict of interest statement
A.S. Petronio is a proctor for Medtronic and Boston Scientific. N. Piazza is a consultant for Medtronic and MicroPort. The other authors have no conflicts of interest to declare.