Almost 40 years have passed since Andreas Grüntzig performed the first successful percutaneous coronary angioplasty of the proximal left anterior descending artery. However, probably not many interventional cardiologists are aware that the first percutaneous structural heart interventions are a bit older, as these were performed before Grüntzig’s remarkable feat. The first atrial septal defects were closed percutaneously in 1974. Then, in the 1980s the Rashkind occluder was introduced, giving the possibility of patent foramen ovale closure1. Also, the first single-balloon valvuloplasty of the mitral valve was described by Inoue in 1984. Another important milestone for structural heart interventions was the introduction of transcatheter aortic valve implantation (TAVI). In 2002, Cribier and co-workers performed the first TAVI in an inoperable patient using a transseptal antegrade approach and a balloon-expandable aortic valve prosthesis, demonstrating the feasibility of percutaneous valve implantation. From then on, the method evolved rapidly. Importantly, advances in technologies dedicated to structural heart interventions expanded treatment possibilities to patients with mitral, pulmonary and even tricuspid valve disease. Most of these technologies are now a part of everyday clinical practice in European countries. This is reflected in the current report which provides a six-year overview on the trends in structural heart interventions in selected countries taking part in the registries endorsed by the European Association of Percutaneous Cardiovascular Interventions (EAPCI)2. From 2010 to 2015, significant changes in structural heart interventions occurred following compelling clinical evidence which became available and subsequent guideline recommendations. TAVI has become the most common procedure in this field, performed especially using the transfemoral approach (mean of about 60%). The highest (as high as 83%) utilisation of the transfemoral approach was reported for France. It might be related to a high level of expertise in French centres. An increasing number of TAVI procedures (Figure 1) met the need of ageing populations across European countries and may also be the result of the Valve for Life initiative initiated by the EAPCI3. The primary goal of this campaign is to popularise and spread knowledge on TAVI in different societies. The campaign is primarily addressed to people 70+ and their families. It serves to introduce the possibility of applying this new method of treatment for patients with severe aortic stenosis who are not good candidates for cardiac surgery. An additional aim of the Valve for Life initiative is to create pressure and a suitable climate for serious discussion with decision makers about increasing reimbursement for TAVI. Moreover, strong evidence in favour of TAVI versus optimal medical treatment and of similar outcomes compared to cardiac surgery in high-risk patients with severe aortic stenosis has meanwhile become available4,5. Appropriate selection of TAVI candidates not only according to widely available risk scores is crucial in order to obtain the best possible outcomes6. However, a large diversity in the number of TAVI procedures is still observed among countries (Figure 2A). Also, some of them, for instance Serbia and Egypt, are at the very beginning of their TAVI programmes. On the other hand, leading countries are extending their indications for TAVI to moderate-risk populations. These new indications are supported by encouraging results of contemporary studies7,8. In addition, recent developments in valve technologies allow better valve positioning/repositioning, thus facilitating the procedure and improving outcomes. Implementation of TAVI in centres without on-site cardiac surgery facilities might be another important step to increase availability. An increasing number of valve-in-valve procedures and paravalvular leak closures is worthy of mention. This might suggest that interventional cardiology may effectively deal with the failure of surgical/percutaneous valve interventions. Interestingly, balloon aortic valvuloplasty (BAV) has experienced a revival in recent years and, similarly to TAVI, its numbers have increased probably due to issues concerning TAVI reimbursement in particular countries. BAV is used mainly in patients with aortic stenosis as a bridge procedure to final therapy – TAVI/surgical aortic valve replacement9. However, it might still be a valuable option for patients scheduled for conservative treatment to relieve symptoms of heart failure. Another growing field is that of mitral valve interventions. At present, the MitraClip procedure is the most popular one. Despite relatively low numbers of procedures, its availability increased from 2010 to 2015 (Figure 1, Figure 2B). On the other hand, MitraClip® technology (Abbott Vascular, Santa Clara, CA, USA) is dedicated to patients with mitral valve insufficiency who are at very high risk for cardiac surgery. Also, these patients should meet strict echocardiographic criteria. Hopefully, the introduction of new devices, for instance Cardioband® (Valtech Cardio, Or Yehuda, Israel) and Harpoon (Harpoon Medical Inc., Baltimore, MD, USA), may address other populations of patients with mitral valve disease. Until recently patients with tricuspid valve disease were overlooked by interventional cardiologists. Luckily, some of the mitral valve-dedicated technologies (MitraClip) have been successfully applied for the treatment of the tricuspid valve. In addition, some new dedicated devices are expected. Thus, we hope that the next EAPCI survey will confirm the broad introduction of these new technologies and indications. Due to increasing life expectancy, apart from the increased rate of degenerative aortic valve disease, a higher prevalence of atrial fibrillation is expected. Thus, the left atrial appendage (LAA) closure technique has become more and more widespread. This technique aims to exclude blood flow from the LAA, thereby reducing thrombus formation and the risk of cerebrovascular accidents in patients with atrial fibrillation. Similarly to TAVI, LAA closure has evolved and been performed more and more frequently over the years (Figure 1). It goes without saying that large variability in the utilisation of LAA closure is observed among countries (Figure 2C). These differences are related first and foremost to reimbursement policies. In some countries, the use of LAA closure is limited only to patients with a high risk of bleeding and contraindications to oral anticoagulation. On the other hand, the strongest evidence supports LAA closure as an alternative to oral anticoagulation10.
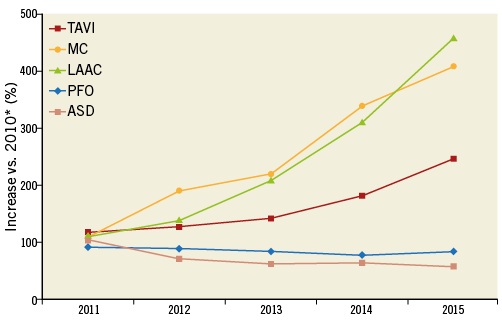
Figure 1. Overall change in the number of structural interventions between 2010 and 2015 in reporting countries. * for countries not reporting data for 2010 the first available number of procedures was used as the reference (assumed no change). ASD: atrial septal defect; LAAC: left atrial appendage closure; MC: MitraClip; PFO: patent foramen ovale; TAVI: transcatheter aortic valve implantation
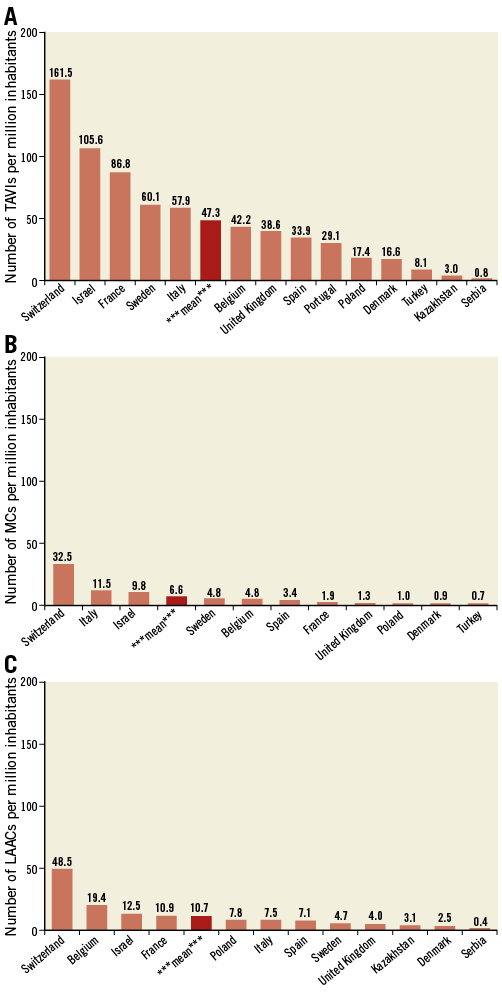
Figure 2. Number of procedures per million inhabitants in different countries in 2015. A) Transcatheter aortic valve implantation (TAVI). B) MitraClip (MC). C) Left atrial appendage closure (LAAC).
Despite inherent limitations linked to the heterogeneous data collection, this six-year overview of the EAPCI registries demonstrates a good overall adoption of novel therapies and implementation of guideline recommendations. The ongoing revolution in the field of percutaneous structural heart interventions and minimally invasive surgical techniques, the so-called “hybrid approach”, is definitely another step towards improving outcomes of high-risk patients. However, as there is no perfect world, interventional cardiologists still struggle with budget constraints and limited reimbursement policies which represent the main reason for the scattered rate of adoption and implementation.
Conflict of interest statement
The authors have no conflicts of interestto declare.

