Randomised controlled trials and large observational registries form the bedrock of research in clinical medicine. Each has limitations and our understanding is enhanced by a synthesis of information from both sources. Broad though the scope of this information is, it provides little insight into the practical issues on which the delivery of healthcare to patients depends. These issues are particularly pertinent at times when there are seismic-like changes in the way in which patients are treated, and when those changes have implications regarding the structure of healthcare provision. The move from thrombolysis to primary PCI was just such an example. Having carefully characterised the benefits of primary PCI over thrombolysis in a series of randomised clinical trials and large registries, the practical implications were far-reaching and present ongoing challenges to those trying to offer this treatment 24/7/365 for patients in widely disparate geographic environments.
The adoption of TAVI represents another example – a disruptive technology whose adoption will result in important changes to the structure of healthcare delivery. TAVI offers a therapeutic option to patients where previously none existed and, as we treat patients at less risk, it will increasingly be used in place of a surgical approach1. Most TAVI procedures are performed in catheter laboratories that are already busy with PCI and electrophysiology procedures. As the volume of TAVI procedures increases, there will be significant implications in optimising the delivery of this new therapeutic option.
Surveys are additional tools that can gather important information to inform the decisions about changing healthcare structures. Like all methodologies, there are limitations that must be understood to interpret findings correctly (Figure 1)2. While the move to online surveys has obvious advantages, the internet is not favoured by older patients, an important consideration when addressing TAVI.

Figure 1. Value of online surveys2. Reproduced with permission © Emerald Group Publishing Limited all rights reserved.
In this issue of EuroIntervention are two surveys that provide interesting and important insights into our new world that includes TAVI and the nascent technology of mitral valve intervention. The EAPCI survey on the current status of transcatheter valve therapy in Europe3 shows a heterogenous uptake of these technologies. The survey was performed from November 2015 to January 2016 and so represents a contemporary snapshot of this fast changing situation. Although only 61% of European centres participated, information was obtained from 301 centres in 25 different countries and so gives us a reasonable impression of the current state of play in most countries with well evolved healthcare systems. While a Heart Team is considered mandatory in the selection of patients for treatment, only 81% of centres had scheduled Heart Team meetings and, though 79% used predefined internal protocols for TAVI case selection, only a quarter included frailty scores. The volumes of activity are also interesting as there was an enormous variation. While a quarter of centres were performing fewer than 100 cases a year, 21% of centres performed >500 cases a year, of which the majority (77%) had started their TAVI programmes before 2008. Volume also appeared to be associated with case mix, so that the proportion of lower-risk cases (STS <8) was 19% in centres performing <400 cases, but 44.5% in those performing >400 cases. The balance between local and general anaesthesia was quite even (53% vs. 47%), though the trend observed in many centres means that local anaesthesia is likely to become dominant quickly. As a clinician it is enormously gratifying to see some elderly patients treated under conscious sedation being discharged the day after their procedure. We can expect the relatively prolonged length of stay identified in this survey (only 11% discharged in <4 days) to reduce in the future.
This new activity has important resource implications. About half had set up a dedicated ambulatory clinic for patients with heart valve disease. TAVI was performed in standard catheterisation laboratories in 61%, and in hybrid operating theatres in 39%. The survey is unable to help us understand if new theatres and catheterisation laboratories are being built to deal with this increased workload.
Planning resources to meet the new demand is fraught with difficulties. In 2012, Osnabrugge et al4 estimated the annual number of new TAVI candidates in Germany would approximate 3,952 (95% confidence interval: 1,684-7,227), and yet we see no obvious end to the meteoric rise of procedures in that country which exceeded 13,264 in 2014 representing 164 TAVI per million population5. While Germany may be a European outlier in this regard, they are not unique in demonstrating that the careful calculations by Osnabrugge et al may be underestimates, even before TAVI starts to be used in lower-risk patients.
A comparison between the wide range of activity, and that estimated to be required in 2014 is presented in Table 1.
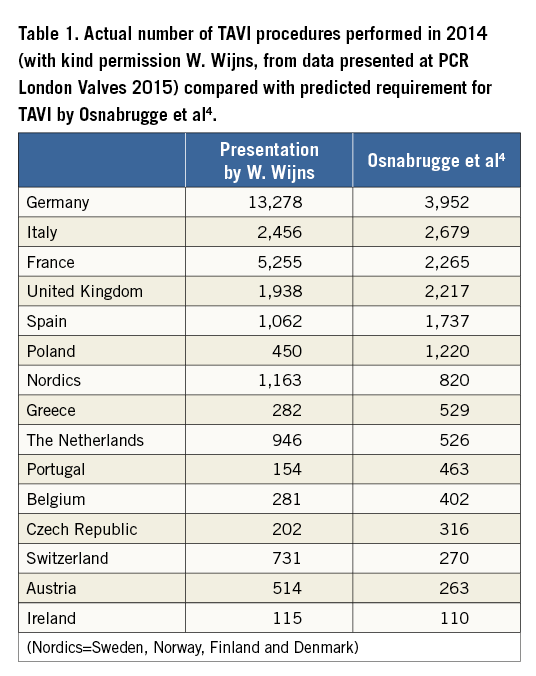
If we examine the ratio between the predicted number of procedures and those actually performed in 2014 (Figure 2), it can be seen that six European countries exceed this by a significant margin and, although Ireland, Italy and the UK were close to predicted, annual rates of increase suggest that they too will exceed these numbers soon.
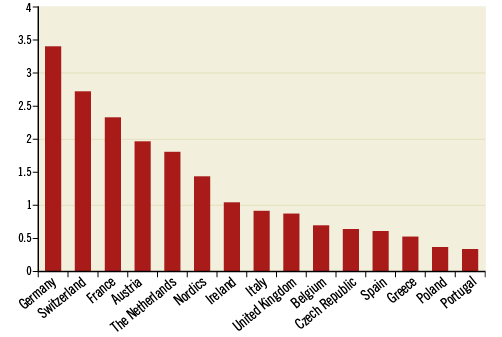
Figure 2. The ratio of number of TAVI procedures performed in 2014 to the number predicted to be needed by Osnabrugge et al4.
The cause of this enormous variation is clearly multifactorial. In spite of the requirement for a multidisciplinary team to assess each case, and the attempt to create objective criteria, the overriding determinant of treatment strategy comes down to the careful clinical assessment of the individual patient by experienced healthcare professionals. Even small changes in the threshold between surgery and TAVI will result in quite different procedural rates. The EAPCI survey gives us some additional insights here. While clinical issues such as patient-specific variables and device-related complications were the most important factors, device costs were felt important in 30%, and regulatory and reimbursement factors in 16%. Thus, while randomised evidence of benefit in lower-risk cases begins to accumulate, and we await data on valve durability, we can expect prices to start to fall, making this technology more cost-effective, and a further shift in indications is likely.
The other survey from Gaede et al6 gives us important insight into patients and general practitioners. It collected views from nine European countries, all with sophisticated healthcare systems and a wide variation in the adoption of TAVI. It used an online methodology, which, as expected, has biased responses towards a younger population with the over 80s very under-represented (only 214/8,860, i.e., 2.5%).
The finding that people’s health concerns are dominated by cancer (27.5%), Alzheimer’s disease (24.7%), stroke (12.4%) and heart attack (9%) will not be a surprise to most. It is a reasonable reflection of published statistics regarding cause of death in older European populations. The prevalence of aortic stenosis is 2-7%, and in this population only 1.7% were “most concerned” about heart valve disease. Nevertheless, valve disease is probably under-represented in national mortality figures, a problem exacerbated by a move away from post-mortem examination. In France, the autopsy rate declined from 15.4% in 1988 to 3.7% in 1997 and will be even less today7. How many elderly patients dying with significant aortic stenosis will remain undiagnosed and be recorded as having died from “heart failure” or “pneumonia”?
The most alarming finding of this survey, however, was the low use of a stethoscope by general practitioners. We do not know how many of the 20% of women and 13% of men who were never examined with a stethoscope were complaining of symptoms that might have been due to aortic stenosis, but the lack of such a pivotal (and cost-free) part of the examination of patients is a source of concern, particularly in the elderly. Unlike many of the other causes of high mortality that dominated patient awareness, suspicion of aortic stenosis requires no complex or expensive diagnostic tests. This survey reinforces the need to increase levels of awareness of aortic stenosis.
In 2015 the EAPCI started the “Valve for Life” initiative with the aim of raising awareness of valvular heart disease in the general population, raising educational standards for healthcare professionals and specialists, and to help facilitate access to novel therapies such as transcatheter heart valve (THV) interventions, reduce obstacles to therapy implementation and diminish age and gender discrimination in the access to care.
Conclusion
These surveys demonstrate a heterogeneous uptake of TAVI as a treatment option in sophisticated European healthcare systems. The current status of TAVI shows us that there is room for improvement and a need for standardisation. There is an urgent need to increase awareness of valvular heart disease, both for the general public and also for general practitioners. The surveys suggest the likelihood of underdiagnosis of aortic stenosis, and show how difficult it is to predict likely demand for this technological advance that offers a key therapeutic option for our increasingly elderly patients.
Conflict of interest statement
The authors have no conflicts of interest to declare.