Abstract
Aims: The influence of age on baseline demographics and outcomes of patients selected for MitraClip® has not been previously investigated.
Methods and results: Baseline demographics and acute outcomes in 1,064 patients from the German TRAMI registry were stratified by age (525 patients ≥76 years and 539 patients <76 years). In elderly patients, logistic EuroSCORE was higher (25[15-40]% vs. 18[10-31]%, p<0.0001) and the proportion of women was greater (47.2% vs. 29.3%, p<0.0001). Elderly patients were more likely to have preserved left ventricular ejection fraction >50% (40.1% vs. 21.8%, p<0.0001) and degenerative mitral regurgitation (DMR, 35.3% vs. 25.6%, p<0.01). Age was the most frequent reason for non-surgical treatment in the elderly (69.4% vs. 36.1%, p<0.0001). The intrahospital MACCE (death, myocardial infarction, stroke) was low in both groups (3.5% vs. 3.4%, p=0.93) and the proportion of non-severe mitral regurgitation at discharge was similar (95.8% vs. 96.4%, p=0.73). A logistic regression model did not reveal any significant impact of age on acute efficacy and safety of MitraClip therapy. In both groups, the majority of patients were discharged home (81.8% vs. 86.2%, p=0.06).
Conclusions: Elderly and younger patients have similar benefits from MitraClip therapy. Age was the most frequent cause for denying surgery in elderly patients.
Abbreviations
DMR: degenerative mitral regurgitation
FMR: functional mitral regurgitation
IQR: interquartile range
LVEF: left ventricular ejection fraction
MR: mitral regurgitation
MV: mitral valve
TRAMI: TRAnscatheter Mitral valve Interventions
Introduction
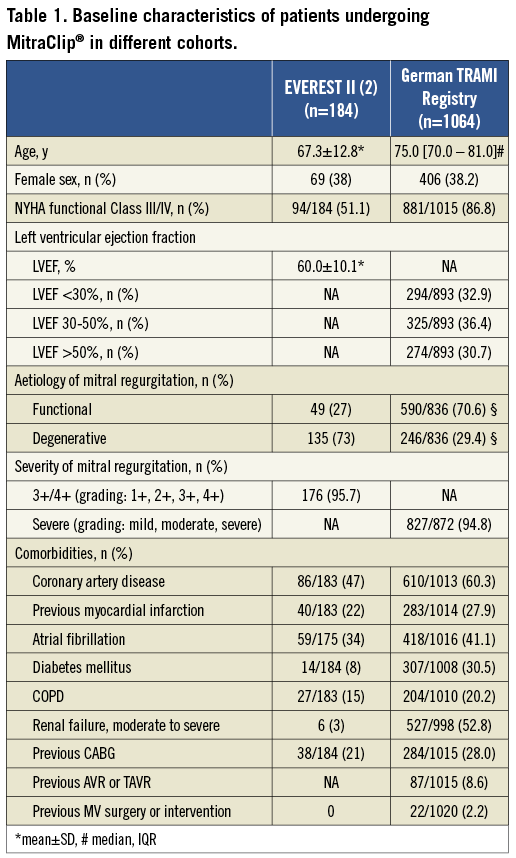
The most common type of heart valve insufficiency, mitral regurgitation (MR) affects more than one in ten people over the age of 75 years – approximately four million people in Europe alone1. Recently, percutaneous mitral valve repair with MitraClip® (Abbott Vascular, Santa Clara, CA, USA) has emerged as a novel therapeutic option in select patients with severe mitral regurgitation (MR). MitraClip has proven efficacy in both degenerative MR (DMR) as well as functional MR (FMR)2-5. EVEREST II, a randomised controlled trial that compared this technology to conventional surgery has shown that MitraClip was associated with superior safety and similar improvements in clinical outcomes2. At 24 months, surgery could be avoided in 78% of patients in the percutaneous group. In contrast, surgery was more effective in reducing MR and the primary efficacy endpoint of freedom from death, from MR 3+ or 4+ and from mitral valve surgery was met significantly more often in surgical patients. This was mainly driven by one out of five patients in the percutaneous group who needed surgery subsequent to MitraClip within six months after the procedure. Yet, EVEREST II enrolled only operable patients with a mean age of 67 years. Large registries on MitraClip therapy, like the German TRAMI registry3 and ACCESS Europe4, have shown that the patient population in a real-world setting was different from EVEREST II. Patients were older and presented with abundant comorbidities. In the German TRAMI registry the median age of patients treated with MitraClip was 75 years and 25% of patients were older than 80 years3. It is therefore obvious that in daily clinical practice MitraClip is considered a viable option for elderly patients. Yet, systematic analyses on the influence of age on outcomes after MitraClip are missing. We therefore stratified acute safety and efficacy outcomes of patients according to age in the German TRAMI registry, which represents the largest database of patients treated with MitraClip in a real-world setting to date.
Methods
GERMAN TRAMI REGISTRY
The German TRAMI registry (also known as the German mitral valve registry) was established in August 2010. The aim of this registry was to assess the efficacy and safety of the procedure in daily clinical practice in Germany and to document the baseline demographics of patients undergoing percutaneous mitral valve interventions as well as the indications used for percutaneous treatment. The registry is open to all German sites performing percutaneous mitral valve therapies. It comprises a retrospective part enrolling patients being treated before the individual study site was initiated for prospective enrolment, and a prospective part after study site initiation. Follow-up for the retrospective part was not defined in the study protocol and was accomplished according to institutional practice. Follow-up for the prospective part was scheduled at 30 days and then at one, three and five years. Data were collected via web-based electronic case report forms by the Institut für Herzinfarktforschung (IHF) at the Heart Center Ludwigshafen. Patients gave written informed consent. Detailed descriptions of the registry and initial results have recently been published3.
PATIENTS
For the present analyses all patients from the German TRAMI registry who underwent a MitraClip procedure were included. As of March 4, 2013, a total of 1,064 patients treated with MitraClip have been enrolled in 20 German sites (504 retrospectively and 560 patients prospectively). Individual centres enrolled between 271 and four (median 36) patients. Baseline demographics of the total cohort are shown in Table 1. For comparison baseline demographics of the EVEREST II cohort2 are also shown. Patients in the German TRAMI registry were older (75 vs. 67 years) and showed extensive comorbidities as compared to EVEREST II. In contrast to EVEREST II, a significant proportion of patients had reduced left ventricular ejection fraction (32.9% of patients had LVEF <30%) and 86.8% of patients had severe heart failure symptoms according to NYHA functional classes III and IV. In addition, the aetiology of MR was different. In the German TRAMI registry, 70.6% of patients had FMR and only 29.4% DMR. In EVEREST II the inverse was true. To evaluate the influence of age, patients were divided into subgroups of patients <76 years and ≥76 years according to the median age in the total cohort.
MITRACLIP PROCEDURE AND MR ASSESSMENT
MitraClip and the procedure have been described in detail previously2. The severity of MR was graded in 3 grades as I (mild), II (moderate) and III (severe) based on actual recommendations6 and evaluated at each individual centre.
STATISTICAL ANALYSIS
Absolute numbers and percentages as well as means (with standard deviation) and medians (with the interquartile range) were computed to describe the patient population and outcomes. The influence of age ≥76 years on efficacy and safety were analysed by multivariate logistic regression models using gender, NYHA IV at admission, LVEF<30%, and coronary artery disease for adjustment. P-values <0.05 were considered significant. All p-values are the results of two-tailed tests. The tests were performed using the SAS© statistical package, version 9.2 (Cary, NC, USA).
Results
BASELINE CHARACTERISTICS AND DECISION MAKING FOR NON-SURGICAL TREATMENT
Table 2 shows baseline characteristics of patients stratified by age. Mean age was 81.0 [78.0-84.0] years in elderly patients and 70.0 [IQR 66.0-73] years in the group of younger patients. The proportion of female patients was higher in elderly patients (47.2% vs. 29.3%). As a consequence, surgical risk as reflected by logistic EuroSCORE and STS Score was higher in elderly patients. Elderly patients were more likely to have DMR (35.3% vs. 25.6%, p<0.01) and preserved ejection fraction (LVEF >50%, 40.1% vs. 21.8%, p<0.0001) and were less likely to have functional FMR (64.2% vs. 76.6%, p<0.0001) and severely depressed left ventricular function (LVEF <30%, 21.7% vs. 43.6%, p<0.0001). The proportion of patients presenting with atrial fibrillation was higher in elderly patients (48.1 vs. 34.4%, p<0.0001). No significant differences were found for other comorbidities.
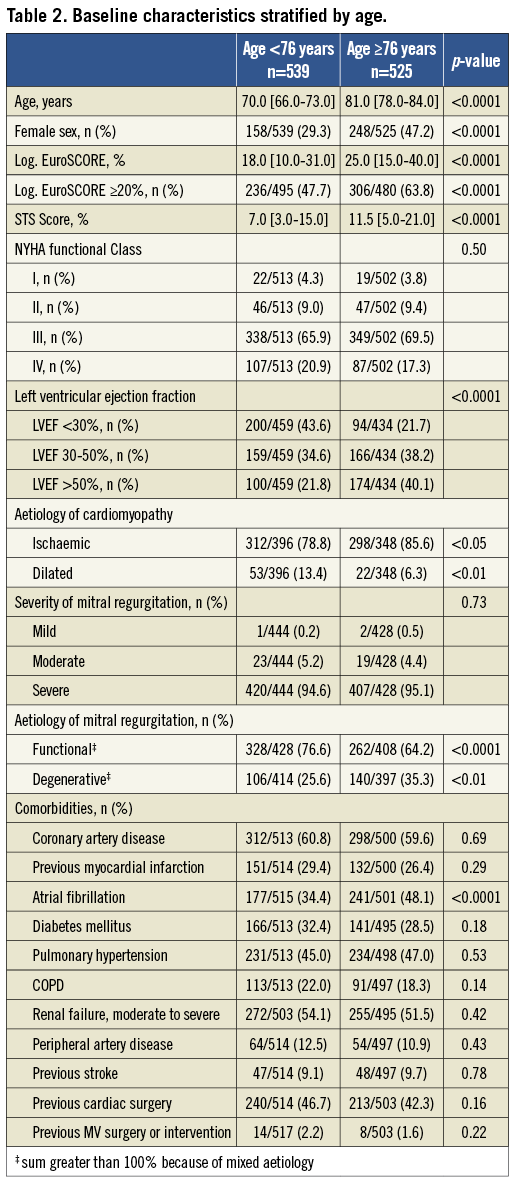
High surgical risk, which is a prerequisite for performing transcatheter valve therapy according to actual guidelines6, was a leading cause for non-surgical treatment in both patient age groups, without significant differences between groups. However, surgical risk reflects the sum of multiple risk factors. The leading single, independent cause for non-surgical treatment was age, which was quoted two times more frequently in elderly patients ≥76 years when compared to the group of younger patients <76 years (69.4% vs. 36.1%, p <0.0001, Figure 1). The allocation of patients for non-surgical treatment was based on a heart team decision in 47.7% of elderly patients and 44.8% of younger patients (p=0.34), on the recommendation of a cardiologist in 51.0% and 53.9% (p=0.33), and on the recommendation of a cardiac surgeon in 1.3% each (p=0.97). A patient’s age did not significantly influence the composition of groups or the specialisation of persons involved in the decision-making process.
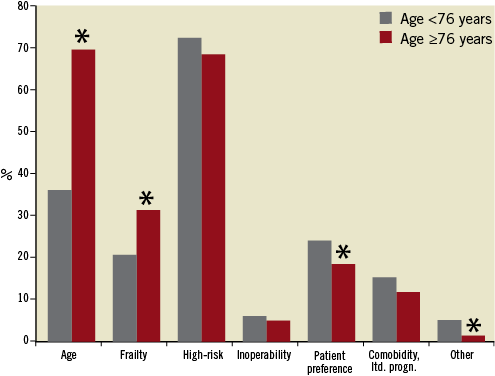
Figure 1. Bar graphs showing causes for non-surgical treatment in different age groups of patients. *p<0.05 vs. age <76 years.
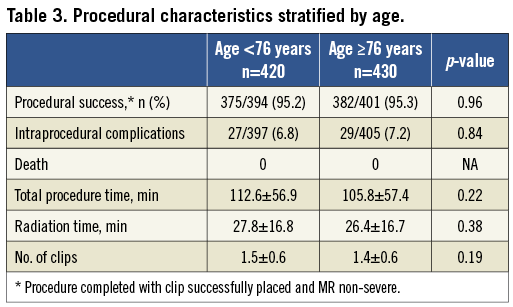
PROCEDURAL CHARACTERISTICS
Technical success, defined as non-severe MR after successful placement of the clip, was high and intraprocedural complications were rare in both age groups. Total procedure time and radiation time were similar and the number of clips placed was not significantly different between groups (Table 3).
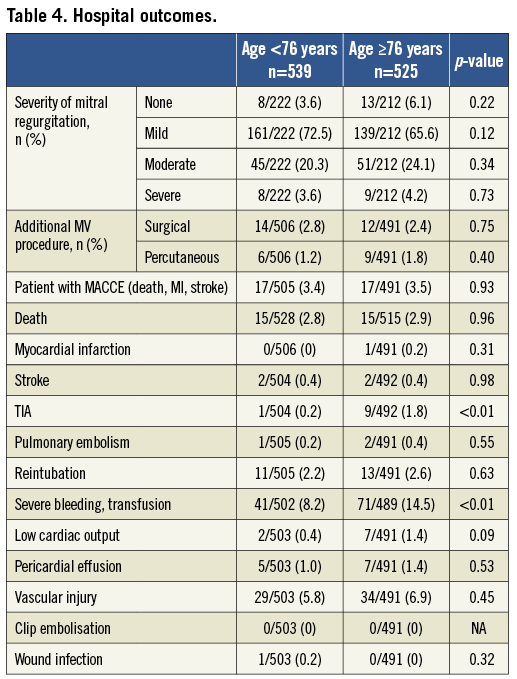
HOSPITAL OUTCOMES
Hospital outcomes are shown in Table 4. The procedure proved to be safe in both groups. Hospital mortality was 2.9% in elderly patients and 2.8% in younger patients (p=0.96). Major adverse cardiovascular or cerebrovascular events (MACCE) defined as a composite endpoint of death, myocardial infarction or stroke was 3.5% vs. 3.4% (p=0.93). Clip embolisation did not occur in either group. Despite this, elderly patients were more prone to experience a transitory ischaemic attack (1.8% vs. 0.2%, p<0.01) and severe bleeding necessitating transfusion (14.5% vs. 8.2%, p<0.01). The need for an additional procedure on the mitral valve after MitraClip was similar in both groups (4.3% vs. 4.0%, n.s.). There was a trend among elderly patients towards more often undergoing a second clip intervention (1.8%) than in younger patients where the second intervention was more likely to be surgery (2.8%). However, this was not statistically significant. The median length of hospital stay was nine days [IQR 7.0-16.0] in elderly patients and eight days [IQR 6.0-15.0] in younger patients (p<0.05).
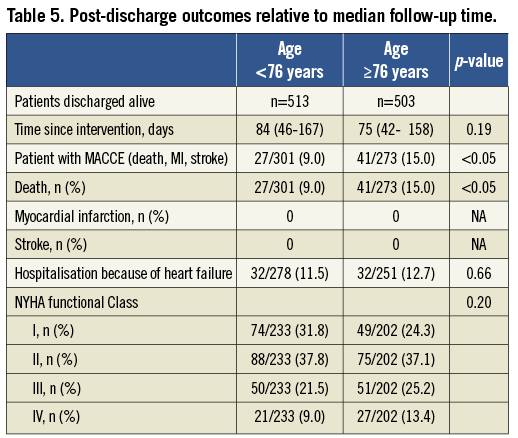
POST-DISCHARGE OUTCOMES
Regular discharge to a normal social environment after termination of mitral valve therapy was possible in 81.8% of elderly patients and 86.2% of younger patients (p=0.06), respectively. Patients not fully recovering after the procedure and needing additional medical therapy or nursing care were 18.1% for the elderly patients and 13.8% for the younger patients. Transfer to a rehabilitation hospital was performed in 9.6% and 7.0% of patients (n.s.), transfer to other hospitals was performed in 4.9% and 4.0% of patients (n.s.), and only 1.8% and 1.2% of patients were in need of new nursing care (Figure 2). The 30-day mortality as estimated by Kaplan-Meier-analyses was 6.7% and 4.7%, respectively (p=0.29). Further post-discharge outcomes were assessed with a median time of 75 and 84 days since intervention in elderly and younger patients, respectively (p=0.19). MACCE were significantly higher in elderly patients (15.0% vs. 9.0%, p< 0.05), which was completely driven by a significantly higher mortality (Table 5). The majority of patients had a substantial clinical benefit concerning the relief of heart failure symptoms, with 69.5% and 61.4% (n.s.) linked to NYHA functional classes of heart failure I and II.
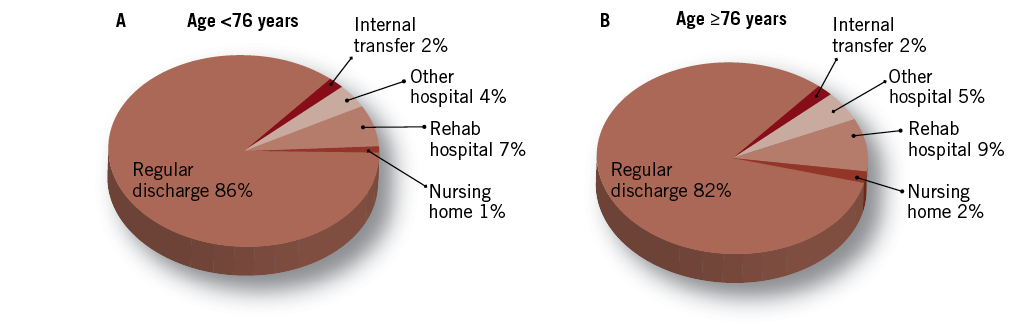
Figure 2. Pie chart showing stay of patients after termination of mitral valve therapy in different age groups of patients.
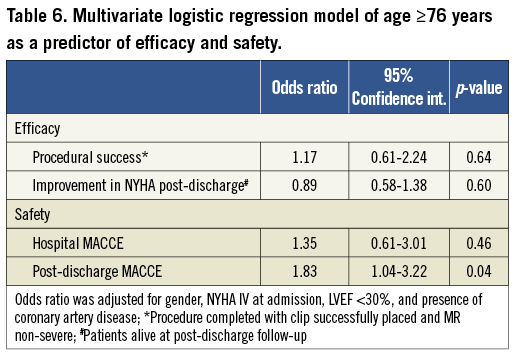
MULTIVARIATE ANALYSES OF THE IMPACT OF ADVANCED AGE ON SAFETY AND EFFICACY
For analysing the independent effect of advanced age on safety and efficacy we performed multivariate logistic regression analyses of age in both age groups adjusted for gender, NYHA IV at admission, LVEF <30%, and coronary artery disease. Efficacy (procedural success and improvement in NYHA functional class post-discharge) as well as hospital safety (hospital MACCE) did not show any statistically significant differences when comparing the elderly to younger patients; yet, advanced age was a predictor of post-discharge MACCE with an odds ratio of 1.83 (Table 6).
Discussion
The present study investigated the influence of age on patient selection and short-term outcomes after percutaneous mitral valve repair using the MitraClip in the German TRAMI Registry, which represents the largest real-world cohort of patients with percutaneous treatment of mitral valve disease. The main findings are that: 1) procedural and hospital safety and efficacy outcomes were similar in elderly patients as compared to younger patients; 2) in three out of four elderly patients, age was indicated as an independent reason for allocating patients to non-surgical interventions; 3) degenerative MR was more frequent in the higher age group; 4) the proportion of patients with preserved left ventricular function was higher in the elderly as compared to younger patients.
There is consensus that surgery is the standard of care for patients with severe symptomatic mitral valve regurgitation. It is also widely accepted that valve repair, when feasible, is the preferred surgical treatment over valve replacement in patients with severe MR6. However, a recent analysis from the Euro Heart Survey on valvular heart disease7 has shown that approximately half of those patients with severe symptomatic mitral valve regurgitation were denied surgery in Europe. The characteristics independently associated with the decision not to operate were lower LVEF, non-ischaemic aetiology, excess of comorbidities, MR grade 3 (as compared to patients with MR grade 4) and advanced age. In particular, the relationship between age and the decision for non-surgical treatment was highly significant in multivariate analyses. This relationship was also found in patients between the ages of 70 and 80, and yet the risk of surgery is only moderately elevated in this group, which does not support denial of surgery on the sole basis of age. In contrast, beyond 80, surgical risk strongly increases with advancing age8-10, and this group accounted for 10% of the study population in the Euro Heart Survey. Since the Euro Heart Survey only included patients who were referred to cardiologists, the true proportion of patients who were denied surgery for advanced age is likely to be considerably higher. Given the life expectancy in industrialised countries, these data are indicative of a relevant treatment gap in elderly patients with symptomatic MR of any aetiology. Besides objective patient characteristics which were associated with therapeutic decisions in the Euro Heart Survey, patient refusal was mentioned in 21% of patients. In the present analysis from the German TRAMI Registry, a patient’s preference as a reason for non-surgical treatment was reported with similar frequency (21.3%) in the total cohort. Interestingly, this was reported less frequently in the elderly as compared to younger patients. However, the subjective component makes it difficult to interpret, and a patient’s preference may be strongly biased by the treating physician7. It is therefore interesting that in both age groups decision making was the result of a heart team discussion in about 45% of patients, and followed the recommendation of the treating cardiologist in over 50% of patients. These data may indicate that the specialisation of persons involved in decision making was not influenced by age, but reflects considerable differences in this process in individual centres. It is, however, also important to note that patient allocation to non-surgical treatment did not adhere to current standards of care. According to current guidelines and European consensus, a decision should be reached through the process of shared decision making, first by a multidisciplinary “heart team” discussion, then by informing the patient thoroughly, and finally by deciding with the patient and family which treatment option is optimal6.
In EVEREST II, which compared the safety and efficacy of MitraClip to surgery, mainly operable patients with DMR were enrolled reflecting a typical surgical cohort with a strong recommendation for surgery according to the guidelines. In this trial, the MitraClip demonstrated superior safety and similar clinical outcomes, but failed to prove non-inferiority with regard to efficacy as compared to surgery. Yet, a subgroup analysis of EVEREST II has suggested that the MitraClip might show similar efficacy to surgery in patients with FMR, reduced LV function and who are 70 years of age or older2. The current situation of medical care in Europe, recommendations in guidelines and results from EVEREST II have led to the selection of a specific population of patients undergoing MitraClip in daily clinical practice with primarily FMR and a high proportion of patients with LV dysfunction, abundant comorbidities and advanced age, thus, patients who are considered inoperable or non-ideal for surgery3,4. Interestingly, in the present study the proportion of patients with DMR and preserved LV function was higher in elderly patients as compared to younger patients. This is likely to represent a higher proportion of patients who might have been good candidates for surgery with regard to morphological aspects and MR aetiology, but who were denied surgery because of age.
The present analysis from the German TRAMI Registry shows that MitraClip was safe in both age groups despite the high surgical risk. This is in accordance with data from the recently published real-world cohorts from European centres3-5,11-15. In the present study, in-hospital mortality was 2.9% in elderly patients and 2.8% in younger patients, 30-day mortality was 6.7% and 4.7%, respectively, and advanced age did not predict increased hospital MACCE in multivariate analyses. Non-major periprocedural complications were also low in both groups. The most common complication was bleeding, necessitating transfusion, and was seen more frequently in the elderly (14.5%) as compared to younger patients (8.2%). Elderly patients were also more prone to experience a transitory ischaemic attack (1.8% vs. 0.2%). This could be related to the fact that atrial fibrillation was significantly more frequent in elderly patients (48.1% vs. 34.4%) and could therefore be a result of periprocedural anticoagulation management; e.g., the cessation of oral anticoagulation. It is therefore important to note that debilitating stroke was a very rare event with similar frequency in both groups. However, the post-discharge mortality of 15.0% and 9.0% that was assessed at a median of about 12 weeks was considerable. Moreover, advanced age was a predictor of post-discharge MACCE in multivariate analyses, with an odds ratio of 1.83. Still, these are much more likely to reflect the advanced age of the patients themselves as well as the abundant comorbidities and reduced health status of the patients treated than to reflect a safety issue of MitraClip therapy.
In addition, MitraClip was effective in both groups. The proportion of patients with non-severe MR at discharge was 95.8% in elderly and 96.4% in younger patients. Multivariate analyses showed that age was not predictive for efficacy. Finally, it is very important to note that the vast majority of patients recovered well and could be discharged to their regular social environment after MitraClip without significant differences between age groups and only a very small proportion of patients in each group were in need of new permanent nursing care after percutaneous treatment. At post-discharge follow-up, the majority of patients had a sustained improvement in heart failure symptoms with 63.4% and 69.5% of patients related to NYHA functional classes I and II. However, it must also be mentioned that roughly one third in each group reported persistent heart failure symptoms according to classes III and IV at post-discharge follow-up.
Limitations of the study
This study has several limitations. The main limitation is that all data were site reported and echo data were not core lab adjudicated. As such, high-quality data on morphological aspects of mitral regurgitation which would have allowed identifying anatomical predictors of outcome were not available. Moreover, although the study was designed as an all-comers study, enrolment was on a voluntary basis. Because the study was not industry sponsored and no remuneration was paid for patient enrolment, the wide range of patients included across all centres probably reflects non-consecutive enrolment in several centres. Moreover, the study did not have any predefined enrolment criteria which is related to the post-market nature of the study. This, however, can also be regarded as a strength of the study since it reflects the real-world application of the therapy and selection of patients. Finally, the follow-up of the patients was limited and time for post-discharge follow-up was inconsistent. Still, it is important to note that long-term outcome is difficult to assess when age, which is a strong risk factor for mortality and morbidity, is interfering with therapy.
Conclusions
MitraClip has the potential to close a relevant treatment gap in elderly patients with severe mitral valve regurgitation. Further investigations are necessary to identify patients from pre-interventional characteristics who are likely to derive a benefit from the procedure. Also, a consensus finding is required to define indications for the MitraClip and surgical techniques in elderly patients. In select patients, the decision to use MitraClip may be justified due to very advanced age on the sole basis of age and patient’s preference provided that their eligibility has been evaluated by a heart team.
Conflict of interest
W. Schillinger has received lecture fees, study honoraria, and travel expenses and is member of an advisory board of Abbott. M. Hünlich has received lecture fees and travel expenses from Abbott. H. Sievert has received consulting fees, travel expenses and study honoraria from Abbott, Access Closure, AGA, Angiomed, Aptus, Ardian, Arstasis, Atritech, Atrium, Avinger, Bard, Boston Scientific, BridgePoint, Cardiac Dimensions, CardioKinetix, CardioMEMS, Coherex, Contego, CSI, CVRx, EndoCross, EndoTex, Epitek, Evalve, ev3, FlowCardia, GDS, Gore, Guidant, InSeal Medical, Lumen Biomedical, HLT, Kensey Nash, Kyoto Medical, Lifetech, Lutonix, Medinol, Medtronic, NDC, NMT, OAS, Occlutech, Osprey, Pathway, PendraCare, Percardia, pfm Medical, ResMed, Rox Medical, Sadra, Sorin, Spectranetics, SquareOne, Trireme, Trivascular, Velocimed, Veryan, Vessix, and holds stock options and stocks from Cardiokinetix, Access Closure, Lumen Biomedical, Coherex. The other authors have no conflicts of interest to declare.

