Abstract
Aims: The aim of this study was to evaluate the prognostic role of echocardiographic parameters assessing secondary mitral regurgitation (SMR) severity and left ventricular dimension, including proportionate versus disproportionate SMR, in MitraClip recipients.
Methods and results: We analysed 137 patients undergoing MitraClip implantation for SMR at three centres. SMR was classified as proportionate or disproportionate based on the median value of the ratio between effective regurgitant orifice area (EROA) and left ventricular end-diastolic volume (LVEDV). The primary endpoint was a composite of cardiovascular mortality and heart failure hospitalisation at two-year follow-up. Mean age was 70±10 years, 80% were male, and median EuroSCORE II was 5.7%. No differences were observed in the disproportionate compared to the proportionate group except for a more severe NYHA class and their expected higher EROA and lower LVEDV. Number of clips deployed, device success and procedural success were similar between the two groups. Residual mitral regurgitation (MR) >1+ at 30 days was more common among patients with an EROA >0.42 cm2 compared to those with an EROA ≤0.42 cm2 (81.3% vs 58%; p=0.004). The relative risk of the primary endpoint was independent from any echocardiographic parameter, including the presence of disproportionate SMR. The only independent predictors of clinical events were EuroSCORE II >8%, NYHA class and residual MR >1+ at 30 days.
Conclusions: Echocardiographic parameters, including the EROA/LVEDV ratio, do not have independent prognostic value in patients undergoing MitraClip implantation. High surgical risk, advanced symptoms and non-optimal MR reduction increase the relative risk of two-year clinical events.
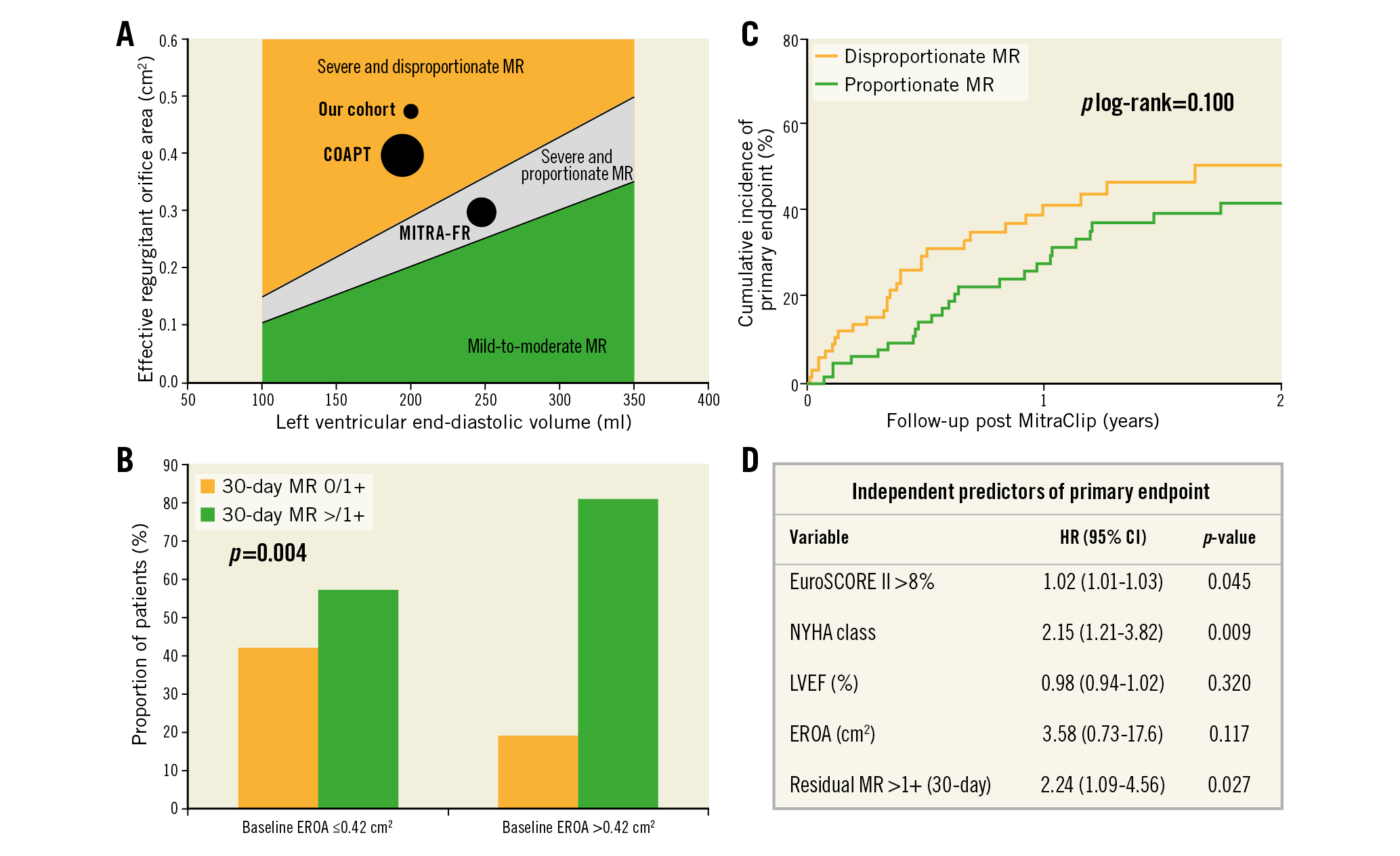
Visual summary. Distribution of effective regurgitant orifice area (EROA) and left ventricular end-diastolic volume (LVEDV) in our population and in those of the COAPT and MITRA-FR trials according to the proportionate/disproportionate classification of secondary mitral regurgitant (SMR) proposed by Grayburn et al (A). Kaplan-Meier curves for the primary endpoint (cardiovascular death or HF hospitalisation at 2 years post MitraClip) of the population stratified by the presence of proportionate SMR (EROA/LVEDV ratio below the median value) or disproportionate SMR (EROA/LVEDV ratio above the median value) (B). Residual SMR (30 days post MitraClip) in patients with baseline EROA above or below the median value (C). Multivariable analysis for the primary endpoint (D).
Introduction
Secondary (or functional) mitral regurgitation (SMR) has a prevalence of 25-30% in patients with heart failure (HF)1 and is an independent predictor of outcomes2. However, two recent prospective randomised controlled trials comparing MitraClip and guideline-directed medical therapy (GDMT) to GDMT alone in SMR patients had opposite results. MitraClip had no effect on mortality and heart failure (HF) hospitalisations in percutaneous repair with the MitraClip device for SMR in the MITRA-FR trial3, while it reduced both HF hospitalisations (primary endpoint) and mortality in the cardiovascular outcomes assessment of the MitraClip percutaneous therapy for HF patients with functional mitral regurgitation (COAPT) trial4. Several hypotheses have been proposed to explain these differences and identify the patients more likely to benefit from the MitraClip procedure5,6,7.
Grayburn et al hypothesised that, in patients whose SMR is disproportionate compared to left ventricular (LV) dilation (COAPT-like patients), the MitraClip might be more effective in improving prognosis than GDMT, while patients in whom SMR is proportionate (MITRA-FR-like patients) might receive the same benefit from MitraClip and GDMT5.
The aim of our study was to assess the prognostic value of echocardiographic parameters assessing SMR severity and left ventricular dimension, including proportionate versus disproportionate SMR, in a population with HF and SMR undergoing MitraClip implantation.
Methods
STUDY POPULATION
This is a retrospective analysis including 137 patients with moderate-to-severe (3+) or severe (4+) SMR undergoing MitraClip implantation between December 2008 and May 2016 at three European institutes (Civil Hospitals of Brescia and University Hospital of Pisa, Italy, and University Hospital of Zurich, Switzerland). We excluded all the patients with primary (or organic) MR and those with incomplete baseline echocardiographic data with respect to the effective regurgitant orifice area (EROA) and the LV end-diastolic volume (LVEDV).
DEFINITIONS
The EROA/LVEDV ratio was calculated as (EROA [cm2]/LVEDV [ml])×1,000.
Patients were defined as having proportionate or disproportionate SMR if their EROA/LVEDV ratio was, respectively, ≤ or > than the median value.
An additional analysis was performed using as cut-off to stratify our population a value derived from Grayburn’s diagram5. The slope of the regression line, calculated considering 0.15 and 0.50 cm2 as EROA values and 100 and 350 ml as LVEDV values, was 1.4.
DATA COLLECTION
For the purpose of the present analysis, echocardiographic data have been separately re-analysed by two expert cardiologists at each individual centre and reviewed by a third reader for consensus when there was disagreement.
Severity of SMR was assessed at each centre by expert operators according to the most recent recommendations8. In particular, for this analysis, EROA, calculated by the PISA method, was considered. Data regarding LV dimension and function were also collected: LV end-diastolic diameter (LVEDD), LV end-systolic diameter (LVESD), LVEDV, LV end-systolic volume (LVESV)) and LV ejection fraction (LVEF). Left atrial volume (LAV) and pulmonary arterial systolic pressure (PASP) were also evaluated.
OUTCOMES
Procedural and acute outcomes were evaluated as technical success, device success, and procedural success according to the Mitral Valve Academic Research Consortium (MVARC) recommendations9.
The primary endpoint was a composite of cardiovascular (CV) death and HF hospitalisations at two-year follow-up. Two-year all-cause death was also analysed.
STATISTICAL ANALYSIS
The normal distribution of continuous variables was explored with the Kolmogorov-Smirnov and Shapiro-Wilk tests. Continuous variables following a normal distribution are reported as mean±standard deviation (SD) and were compared using the Student’s t-test, whereas those not following a normal distribution are presented as median and interquartile range (IQR) and were compared with the Mann-Whitney U test. Categorical variables are reported as counts and percentages and were compared using the χ² or Fisher’s exact test, as appropriate. To explore the linearity of the relationship between EROA/LVEDV ratio and events, a cubic spline analysis was performed. The cumulative incidence of clinical events at two years was estimated using the Kaplan-Meier method and the differences between groups were calculated using the log-rank test. A multivariable Cox regression analysis, including baseline variables differently distributed at an alpha level of 0.10, was performed. Each result is expressed as hazard ratio (HR) and corresponding 95% confidence interval (CI). For all analyses, a two-sided p<0.05 was considered to be significant. All statistical analyses were performed using SPSS, Version 21 (IBM Corp., Armonk, NY, USA) and Stata, version 14.2 (StataCorp LP, College Station, TX, USA).
Results
BASELINE CHARACTERISTICS
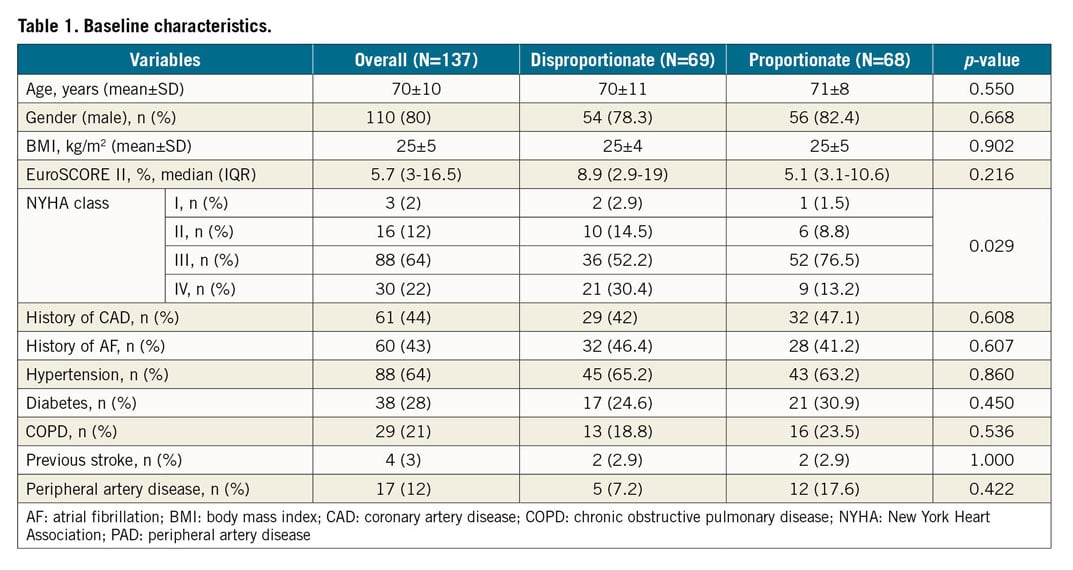
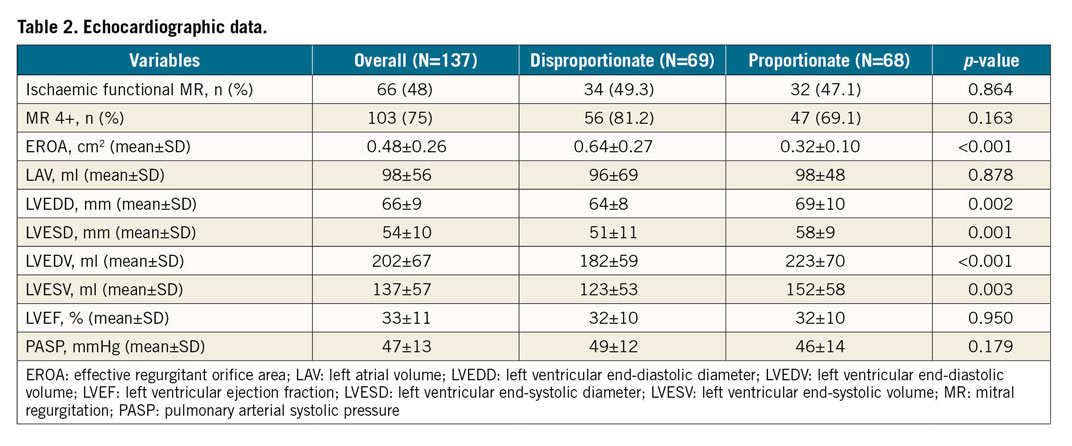
Mean age of the overall population was 70±10 years, 80% were male and median value of EuroSCORE II was 5.7%. Most of the patients had advanced symptoms (64% were in NYHA Class III, and 22% in NYHA Class IV). Almost half of them had ischaemic SMR and 75% had severe SMR (4+). Mean and median values of EROA were 0.49±0.26 cm2 and 0.42 (IQR 0.31-0.56) cm2, respectively. Mean and median values of LVEDV were 202±68 ml and 190 (IQR 160-231) ml, respectively.
The EROA/LVEDV ratio had a median value of 2.25. No differences were observed, with respect to demographic and clinical characteristics, between patients with disproportionate SMR compared to those with proportionate SMR, except for NYHA class that was more severe in the patients with an EROA/LVEDV ratio above the median value compared to the others (Table 1). As expected, patients with disproportionate SMR had higher EROA and smaller ventricles compared to those with proportionate SMR (Table 2). No other differences between groups were noted with respect to other parameters, including LVEF, LAV, and PASP (Table 2).
Considering Grayburn’s diagram5, our cohort was positioned close to the COAPT population in the disproportionate area, though with a slightly higher mean EROA value compared to COAPT (0.48 cm2 vs 0.41 cm2) (Visual summary).
Considering the cut-off derived from Grayburn’s diagram, 107 patients (78%) had disproportionate SMR, while the remaining 30 (22%) patients had proportionate SMR. Baseline characteristics did not differ between these two groups except for the expected higher EROA (0.55±0.26 cm2 vs 0.27±0.08 cm2; p<0.001) and lower ventricular dimensions (LVEDV: 188±54 ml vs 254±85 ml; p<0.001) in the patients with disproportionate SMR, compared to those with proportionate SMR. Patients with disproportionate SMR also had higher PASP (49±12 mmHg vs 40±13 mmHg; p<0.001).
ACUTE AND EARLY-TERM OUTCOMES
Forty percent of patients received one clip, while two devices were implanted in 51% of the population. The number of deployed clips did not differ between patients with disproportionate and proportionate SMR, using both definitions. Technical success was achieved in all patients. Device success and procedural success, evaluated at 30 days, occurred in 80.3% and 75.2% of the overall population without differences between groups (Table 3). In particular, residual MR at 30 days was comparable in patients with disproportionate compared to proportionate SMR, regardless of the definition used.
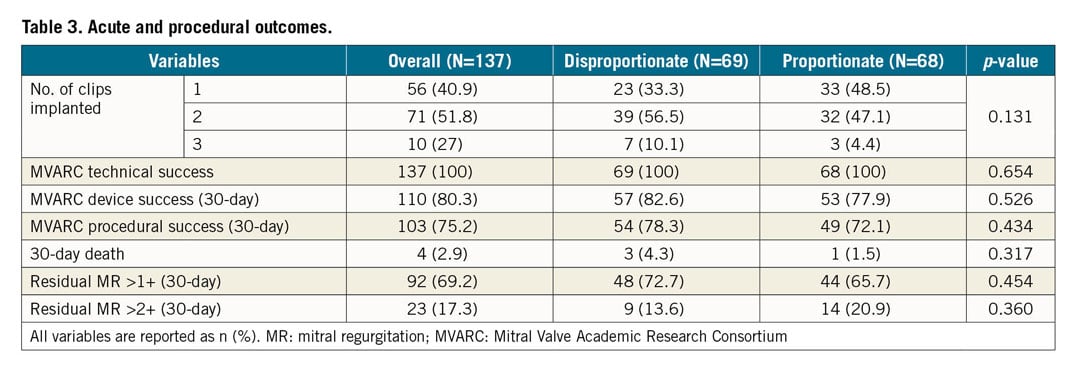
Residual MR >1+ at 30 days was more frequently observed in patients with EROA above the median value (81.3% in patients with EROA >0.42 cm2 vs 58% of those with EROA ≤0.42 cm2; p=0.004) (Visual summary). No differences in residual MR >1+ at 30 days were found when patients were subdivided according to median LVEDV (69.2% in patients with LVEDV ≤190 ml vs 69.1% in those with LVEDV >190 ml; p=0.989).
LONG-TERM OUTCOMES
The median follow-up duration was of 461 (interquartile range, 213-884) days.
Twenty-eight patients died during the first year after MitraClip implantation, 16 of CV causes. In the second year of follow-up, 13 patients died, 8 from CV causes. Hospitalisations due to HF occurred in 39 patients, and the composite endpoint of CV death or HF hospitalisation occurred in 52 patients, during the first two years of follow-up.
A linear relationship between EROA/LVEDV ratio and two-year clinical events (both primary endpoint and all-cause death) was observed (Supplementary Figure 1).
The cumulative incidence of the two-year composite endpoint was 46.1%, with a numerically higher rate among patients with EROA >0.42 cm2 compared to those with EROA ≤0.42 cm2 (53.4% vs 41%; log-rank p=0.064) (Figure 1). No significant differences were observed between patients with LVEDV > or ≤190 ml (48.4% vs 43.3%; p=0.900) (Figure 2) or between patients with proportionate or disproportionate SMR (41.5% vs 50.3% using the definition based on the median EROA/LVEDV ratio, log-rank p=0.100; and 44% vs 46% using Grayburn’s cut-off, log-rank p=0.318) (Visual summary, Supplementary Figure 2).
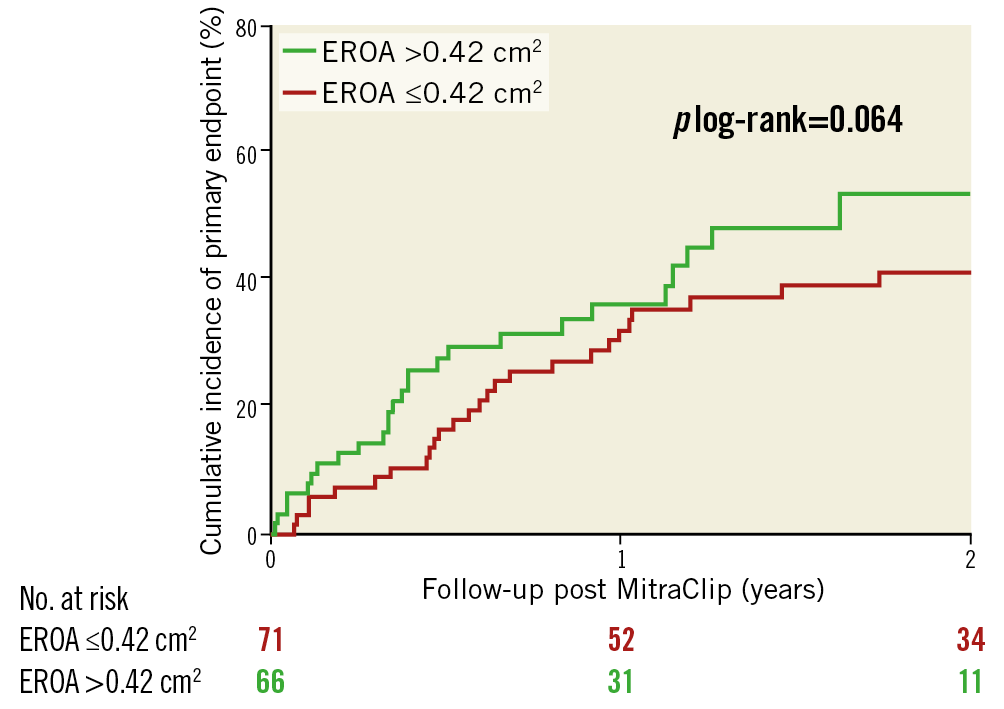
Figure 1. Cumulative incidence of the primary endpoint according to mitral regurgitation severity. Kaplan-Meier plots of the population stratified by median effective regurgitant orifice area (EROA).
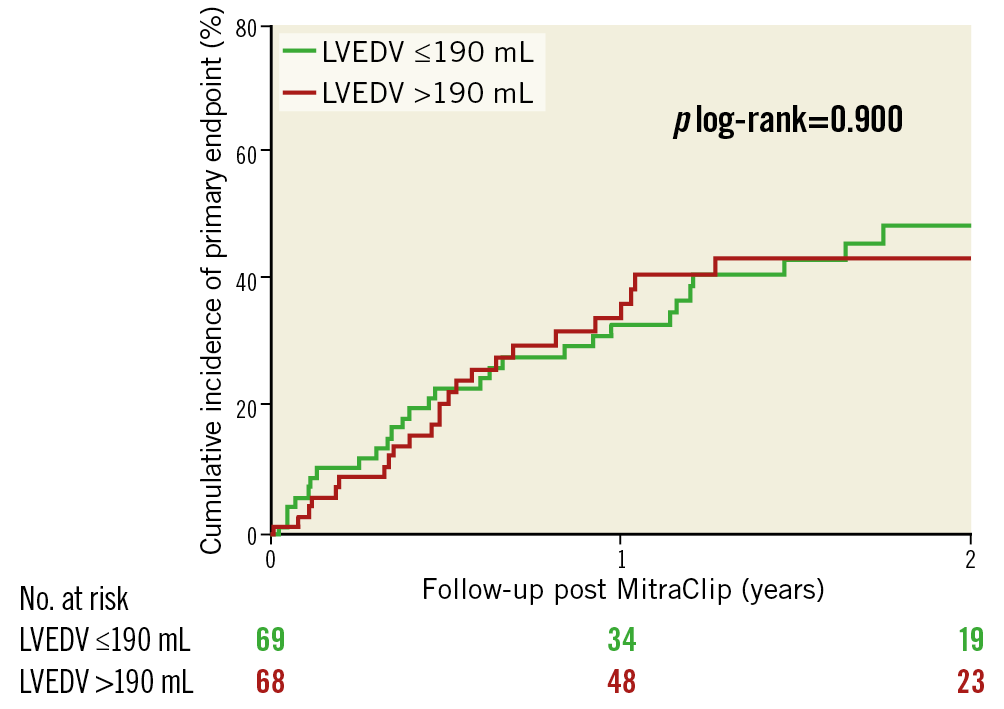
Figure 2. Cumulative incidence of the primary endpoint according to left ventricular dimension. Kaplan-Meier plots of the population stratified by median left ventricular end-diastolic volume (LVEDV).
The cumulative incidence of two-year all-cause death was 39.4% and did not differ significantly in patients with EROA > versus ≤0.42 cm2 (35.1% vs 45.6%; log-rank p=0.223), LVEDV > versus ≤190 ml (45.9% vs 33.5%; log-rank p=0.129), or proportionate versus disproportionate SMR (33.4% vs 46.2% using the definition based on the median EROA/LVEDV ratio, log-rank p=0.091; and 26.2% vs 43.9% using Grayburn’s cut-off, log-rank p=0.066) (Supplementary Figure 3).
PREDICTORS OF LONG-TERM OUTCOMES
The presence of disproportionate SMR at baseline did not predict better long-term outcomes (Supplementary Table 1).
A larger EROA was associated with worse outcomes at univariate analysis but lost its power at multivariable analysis. Residual MR >1+ at 30 days and NYHA class were associated with a twofold increased risk of the two-year composite endpoint. An increased risk of clinical events was also observed in patients with a EuroSCORE II >8% (Visual summary).
Discussion
The main findings of the present analysis are the following. First, echocardiographic parameters, including the presence of disproportionate SMR, did not predict outcomes after MitraClip implantation in our selected population. Second, patients with disproportionate SMR had more severe HF symptoms, higher EROA and lower LVEDV compared to those with proportionate SMR. Third, patients with larger EROA were more likely to have residual MR >1+. Finally, the only independent predictors of long-term clinical outcomes were NYHA class, residual MR >1+ at 30 days after MitraClip implantation and EuroSCORE II >8%.
Percutaneous edge-to-edge mitral valve repair using the MitraClip has been part of clinical practice for many years. However, proper patient selection remains challenging. The apparently opposite results of the MITRA-FR and COAPT trials were followed by different interpretations3,4,5,6,7. One of the most interesting hypotheses was focused on the relationship between the severity of SMR and LV dilation. Grayburn et al proposed a classification of SMR as proportionate, when the regurgitation is appropriate to the LV dilation, and disproportionate, when it is excessive compared to LV dimensions. According to this hypothesis, patients with disproportionate SMR would have a prognostic benefit from MitraClip therapy compared to optimal doses of GDMT5.
Grayburn’s classification is useful to explain differences in outcomes between the MITRA-FR and COAPT trials as the two study groups differed with respect to patients’ EROA and LVEDV. The characteristics of our patients are more similar to those of COAPT than of MITRA-FR (LVEDV: 202 ml versus 194 ml in COAPT and 250 ml in MITRA-FR, and EROA 0.48 cm2 versus 0.41 cm2 in COAPT and 0.31 cm2 in MITRA-FR)3,4.
To evaluate whether the EROA/LVEDV ratio had a prognostic value in our patients, we classified them as having disproportionate or proportionate SMR based on the median value of their EROA/LVEDV ratio. The choice of the median value was based on the presence of a linear relationship between EROA/LVEDV ratio and outcomes without deflection points. However, as sensitivity analysis, we compared patients with proportionate versus disproportionate SMR classified on the basis of Grayburn’s diagram5.
Nevertheless, EROA, LVEDV, and their ratio, regardless of the definition used, did not have an independent association with clinical events in our patients. Echocardiographic parameters, including LVEDV and EROA, also did not have an independent association with outcomes in a recent analysis of COAPT10.
There are several hypotheses to explain the lack of differences between proportionate and disproportionate SMR after MitraClip implantation in our population.
1. SELECTION CRITERIA
Having features closer to those of COAPT, our population can be considered as highly selected. Most of our patients (78%) had a disproportionate SMR according to Grayburn’s definition. The number of our patients with proportionate SMR was therefore small and we probably lacked statistical power for the comparison with patients having disproportionate SMR, using Grayburn’s cut-off. Therefore, our results should be cautiously interpreted and need to be definitively confirmed by further investigations.
2. WORSE OUTCOME OF PATIENTS WITH DISPROPORTIONATE SMR TREATED BY MEDICAL THERAPY
The prognostic role of the classification into proportionate and disproportionate SMR has recently been shown by Bartko et al in patients with SMR on medical treatment. In this study, patients with disproportionate SMR had poorer outcomes compared to those with proportionate SMR or with no significant SMR11. The similar outcomes of patients with proportionate and disproportionate SMR who underwent MitraClip implantation in our study are consistent with a beneficial effect of MitraClip in the patients with disproportionate SMR, neutralising its untoward effects on outcomes. This hypothesis would be in line with that of Grayburn where patients with disproportionate SMR had the greatest benefit from MitraClip.
3. NEGATIVE IMPACT OF AN EXCESSIVE EROA
The large EROA of our patients, up to 0.64 cm2 in those with disproportionate SMR, was probably responsible for the higher rate of suboptimal results after a MitraClip procedure (MR >1+ at 30 days). Interestingly, the number of clips used, which was slightly lower compared to COAPT, was similar in our two groups, despite higher EROA in disproportionate versus proportionate SMR. Evidence about the association between high EROA and a suboptimal result after MitraClip implantation is still limited. Lubos et al reported a higher rate of procedural failure among patients with EROA >0.7 cm212. Moreover, despite the fact that the prognostic role of residual MR >2+ is well known13,14,15, few data are available about the prognostic impact of residual MR >1+. Buzzatti et al pointed out that residual MR 2+ was associated with a worse prognosis compared to residual MR 0/1+ after MitraClip therapy16. This is in line with previous studies showing that the degree of SMR is related to patients’ outcomes1,17 and is probably because residual MR, even if 2+, could lead to persistence of LV overload and lack of LV reverse remodelling. We confirm these results showing, in a large multicentre population, that a non-optimal treatment (residual MR >1+ at 30 days after MitraClip implantation) is a strong and independent predictor of two-year clinical events. The results of MitraClip treatment had a major relation with clinical outcomes, outweighing the role of EROA alone. Based on these findings, the best candidates for MitraClip treatment would be patients with SMR more likely to be optimally corrected.
We could also hypothesise that excessive EROA may be a surrogate of advanced disease and that we should treat patients at an earlier stage to avoid the occurrence of “over-disproportionate” SMR.
4. DISPROPORTIONATE SMR AND MORE SEVERE SYMPTOMS IN OUR POPULATION
More advanced symptoms were noted in the disproportionate compared to the proportionate group. Together with residual MR, NYHA class was another strong independent predictor of events. Advanced NYHA class has already been reported as having a negative impact on clinical outcome after MitraClip treatment13,18,19. However, current guidelines still suggest that the MitraClip should be considered in patients with persistence of NYHA class from II to IV despite GDMT8. We speculate that an early stage of symptoms should drive us in the selection of MitraClip candidates to obtain a prognostic benefit.
Based on what is stated above, our study should not be interpreted as opposite but rather complementary to Grayburn’s framework.
Of note, in addition to residual MR and symptoms, EuroSCORE II, that is known to be the best score predicting outcomes after MitraClip treatment even at long-term follow-up20,21, was also confirmed to have an independent role in increasing the risk of clinical events in our population.
Limitations
Our study has several limitations. Firstly, it has the inherent limitation of its retrospective design. Secondly, as a non-randomised study without a control arm, several confounding factors could have influenced our results. Thirdly, the sample size is relatively small; this could have led to a type II error in the interpretation of results. Fourthly, data about right ventricular function and natriuretic peptides, which are known to have a prognostic impact in MitraClip recipients, and medical therapy are lacking. Moreover, data about the presence of left bundle branch block or history of prior inferior-posterior myocardial infarction, which could be associated with disproportionate SMR, are also lacking. Finally, EROA is a single frame measurement and can underestimate MR severity if the orifice is markedly elliptical and can also overestimate MR severity in biphasic or early systolic SMR.
Conclusions
Echocardiographic parameters, including the EROA/LVEDV ratio, did not have an independent prognostic value in a selected population undergoing MitraClip implantation. Patients with large EROA seem less likely to receive an optimal SMR correction. Residual MR >1+ at 30 days, NYHA class and EuroSCORE II >8% are the only independent predictors of long-term clinical events.
|
Impact on daily practice In the patient selection for percutaneous edge-to-edge mitral valve repair, echocardiographic parameters seem not to impact on long-term outcomes. On the other hand, patients with high calculated surgical risk, advanced symptoms and/or a non-optimal MitraClip result are probably those less likely to have a prognostic benefit from the procedure. Attention should be paid in the presence of too large an effective regurgitant orifice area that may be associated with non-optimal correction. |
Acknowledgements
We thank Gianmarco Arabia and Gregorio Zaccone for their support in data acquisition, and Riccardo Maria Inciardi for assistance in statistical analysis.
Conflict of interest statement
F. Maisano has received grant and/or research support from Abbott, Medtronic, Edwards Lifesciences, Biotronik, Boston Scientific Corporation, NVT, and Terumo, consulting fees and honoraria from Abbott, Medtronic, Edwards Lifesciences, SwissVortex, Perifect, Xeltis, Transseptal Solutions, Cardiovalve, and Magenta, royalty income/IP rights from Edwards Lifesciences (FMR surgical annuloplasty), and is a shareholder of Cardiovalve, Magenta, SwissVortex, Transseptal Solutions, Occlufit, 4Tech, and Perifect. M. Metra has received consulting honoraria for participation in steering committees or advisory boards or for speeches from Abbott, Amgen, AstraZeneca, Bayer, Edwards, Fresenius, Novartis, and Servier. A.S. Petronio is a consultant for Medtronic, Abbott, and Boston, and has received research funds from Abbott, Boston and Gada. M. Taramasso is a consultant for Abbott Vascular, Boston Scientific, 4Tech, and CoreMedic, and has received speaker fees from Edwards Lifesciences. M. Zuber has received speaker fees and consulting fees from Abbott, Cardiovalve, SwissVortex, Edwards, Pfizer and Canon. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.