Abstract
Aims: Patients with severe secondary mitral regurgitation (MR) and normal ejection fraction are being excluded from clinical trials evaluating transcatheter mitral devices. We sought to evaluate the long-term mortality with medical management alone in this patient population.
Methods and results: We retrospectively evaluated patients diagnosed with ≥3+ MR at our institution over 15 years. Only patients with an ejection fraction ≥60% were included in the study. Those with degenerative mitral valve disease, papillary muscle dysfunction, or hypertrophic cardiomyopathy, and those who underwent mitral valve intervention were excluded. The study included 400 patients (age 71.1±14.8, 25.1% male, ejection fraction 62.5±3.6%). Mechanism of secondary MR was restricted valve motion, annular dilation and apical tethering in 91.5, 4.5 and 4%, respectively. One-year and three-year mortality were 19.1 and 26.3%, respectively. On multivariable Cox proportional regression analysis, older age, New York Heart Association functional Class III or IV, >3+ MR and larger left atrium were independent predictors of mortality.
Conclusions: Severe secondary MR with normal left ventricular systolic function has significant mortality with medical management alone. This initial observation needs to be confirmed in larger prospective studies. These patients should be included in future transcatheter clinical trials.
Abbreviations
AF: atrial fibrillation
AMR: atrial mitral regurgitation
CAD: coronary artery disease
EF: ejection fraction
LA: left atrium
LV: left ventricle
MR: mitral regurgitation
MV: mitral valve
Introduction
Mitral regurgitation (MR) is among the most common valvular heart disorders in the western world1-3. It is generally classified into primary –which is caused by a structural pathology of the valvular apparatus– and secondary MR –which occurs despite a structurally normal mitral valve (MV).
Secondary MR occurs most commonly secondary to left ventricular (LV) dilation in heart failure patients due to the resultant mitral annular dilation and apical papillary muscle displacement4,5. More recently, newer factors for secondary MR have been described, where atrial remodelling (e.g., due to atrial fibrillation [AF]) is the main driver of imperfect leaflet coaptation; the term “atrial MR” (AMR) has been used to refer to the secondary MR demonstrated in this setting6-8. Those newer mechanisms have been recognised by the Mitral Valve Academic Research Consortium (MVARC)9; yet, in contrast to secondary MR in the setting of LV dysfunction, little is known about the prognosis and natural history of secondary MR in patients with normal LV systolic function. Furthermore, patients with severe secondary MR and normal ejection fraction (EF) are currently being excluded from clinical trials evaluating transcatheter MV intervention9.
In this study, we sought to characterise the clinical and echocardiographic features of this unique population of secondary MR patients and assess their long-term mortality with conservative management.
Methods
STUDY POPULATION
All consecutive patients who had comprehensive two-dimensional (2D) transthoracic echocardiography (TTE) or transoesophageal echocardiography (TEE) carried out at our institution between January 2000 and December 2014 had been prospectively maintained in the echocardiography data registry and were screened for eligibility for the current study. Only patients who were ≥18 years of age with 3+ (moderately severe) and/or 4+ (severe) secondary MR and EF ≥60% were eligible for inclusion and were retrospectively identified. The study excluded patients with an EF <60%, those with MR mechanisms consistent with primary MR (myxomatous degeneration, mitral valve prolapse, rheumatic thickening, chordal rupture, etc.), papillary muscle scarring or dysfunction, hypertrophic or restrictive cardiomyopathy, constrictive pericarditis, as well as those who underwent percutaneous or surgical MV intervention before or after the index echocardiogram. The Cleveland Clinic Institutional Review Board approved the study with waiver of individual informed consent.
ECHOCARDIOGRAPHY DATA
All echocardiographic images were reviewed and read by experienced cardiologists in the cardiac imaging section of our Heart and Vascular Institute at the Cleveland Clinic at the time of the original study. Standard echocardiographic measurements were recorded and severity of MR was graded from 1+ to 4+ after comprehensive evaluation, incorporating vena contracta, visual estimate of opacification of LA, regurgitant volume and fraction, and effective regurgitant orifice area to report the grade of severity of MR, according to the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE) guidelines10-12. The predominant mechanism of MR was determined and documented in the echocardiography data registry at the time of the original study, and was used for selection of the study population. Upon retrospective review, the secondary MR population was defined by exclusion of MR mechanisms consistent with primary MR or papillary muscle scarring or rupture, in addition to hypertrophic or restrictive cardiomyopathy and constrictive pericarditis (Figure 1). For patients who had more than one echocardiogram over time, the very first study showing 3 or 4+ MR was used as the index echocardiogram. When relevant clinical or echocardiographic data were missing, electronic medical records were interrogated and information was obtained by individual chart review.
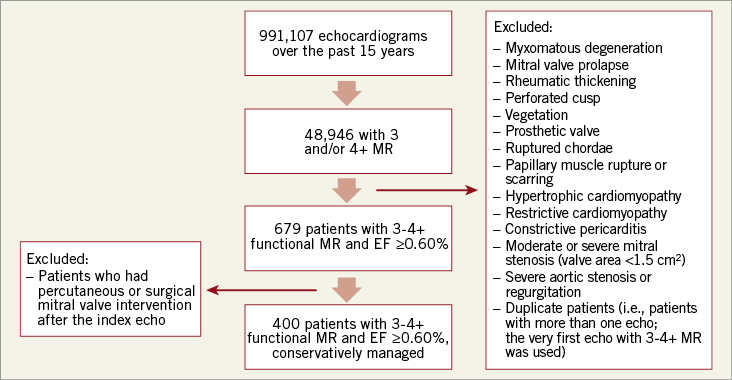
Figure 1. A schematic illustration of the selection process of the study population from our echocardiography database.
FOLLOW-UP AND OUTCOMES
The date of the index echocardiogram was defined as the beginning of the observational period. Follow-up was ascertained by chart review and we recorded the date at which events occurred. Mortality data for the cohort were obtained from medical records and the US Social Security Death Index database (last inquiry in October 2015). Primary outcome was one-year and three-year all-cause mortality.
STATISTICAL ANALYSIS
Continuous variables were expressed as means±standard deviation (SD), or medians and interquartile range (IQR) for skewed distributions, and compared using the Student’s t-test or the Mann-Whitney test, respectively. Categorical data were expressed as percentages and compared using Pearson’s chi-square test or Fisher’s exact test where applicable.
Multivariable Cox proportional regression analysis was performed to identify significant independent predictors of adverse outcomes. The regression model was adjusted for age, sex, smoking status, coronary artery disease (CAD; defined as history of myocardial infarction, coronary artery bypass grafting or percutaneous coronary intervention, or presence of >70% stenosis on prior coronary angiogram), AF, diabetes mellitus, hypertension, EF, mechanism of secondary MR, MR grade, LA diameter and New York Heart Association functional class. LA diameter was analysed as both a continuous variable and as categorised into quartiles. Variables with >25% missing data were not included in the model (LA systolic surface area, LA volume, LA indexed volume, LV end-systolic and end-diastolic diameters, LV end-systolic and end-diastolic volumes, and effective regurgitant orifice area). Hazard ratios (HRs) with 95% confidence intervals (CI) were calculated and reported. Kaplan-Meier curves were used to represent univariable data graphically, and event curves were compared using the log-rank test.
All p-values reported are from two-sided tests and p<0.05 was considered statistically significant. All model assumptions were examined including linearity, collinearity, additivity, and proportional hazards. Statistical analysis was performed using Stata, version 12 (StataCorp LP, College Station, TX, USA) and SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Figure 1 illustrates the selection process of the study population from our echocardiography database. Between January 2000 and December 2014, 991,107 studies were performed at our institution. Out of these studies, 679 patients were found to have 3 and/or 4+ secondary MR and an EF ≥60%, 400 of whom had no subsequent surgical or percutaneous MV intervention and were managed conservatively. Those 400 patients were included in the current analysis. Baseline characteristics and echocardiographic data of the study population are shown in Table 1. Mean age was 71.1±14.8 years, 25.1% were male, 60.5% were hypertensive, and 26 and 44.4% had CAD and AF, respectively. Mean EF was 62.5±2.3%. Mean LV end-systolic and end-diastolic diameters were 29±6 and 46±7 mm, respectively, and mean LA diameter was 47±10 mm. Patients with 3+ MR were 59.8% while those with >3+ MR (i.e., 3-4+ or 4+ MR) were 40.2%. The vast majority of patients (82%) were asymptomatic or with mild symptoms (New York Heart Association functional Class I or II).
MECHANISMS OF SECONDARY MR
The primary mechanisms of secondary MR identified in the study population were restricted valve motion (91.5%), annular dilation (4.5%) and apical tethering (secondary to apical displacement of the posteromedial papillary muscle) (4%), as shown in Figure 2. Mean LA diameter in patients with restricted valve motion, annular dilation and apical tethering was 47±10, 51±6 and 47±18 mm, respectively (p=0.449).
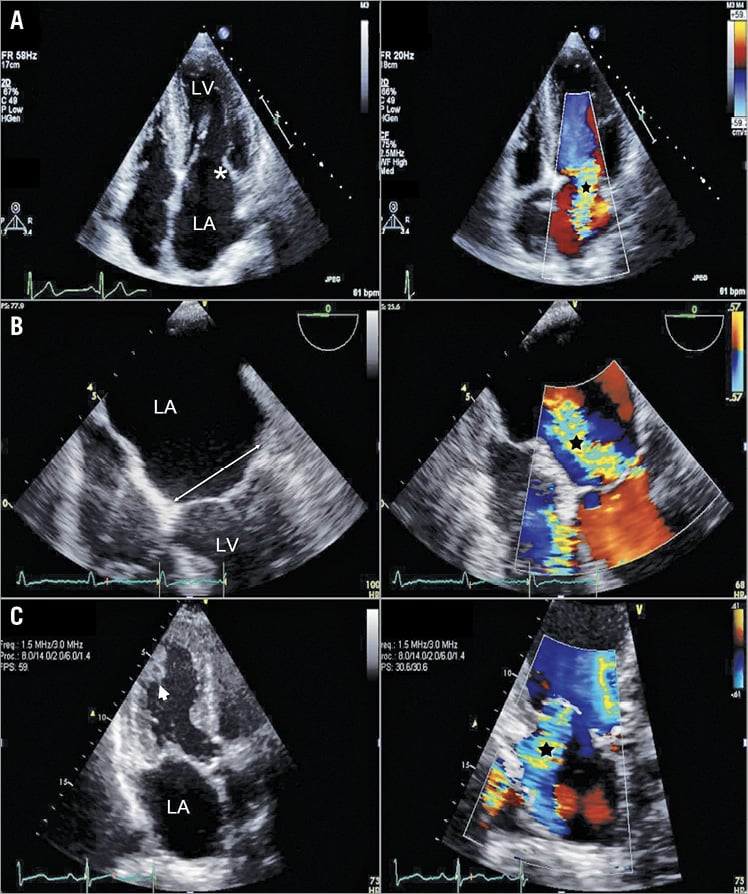
Figure 2. Echocardiographic mechanisms of secondary mitral regurgitation (MR) identified in the study population. A) Apical four-chamber view (left) showing restricted motion of the posterior mitral leaflet (asterisk), and colour Doppler flow (right) in the same view demonstrating significant jet of MR (black star). B) Transoesophageal echo image (left) showing mitral annular dilation (double-headed arrow) secondary to severe left atrial dilation, and colour Doppler flow (right) in the same view demonstrating significant jet of MR (black star). C) Apical three-chamber view (left) showing apical tethering of mitral leaflets secondary to apical displacement of the posteromedial papillary muscle (arrowhead), and colour Doppler flow (right) in the same view demonstrating significant jet of MR (black star). LA: left atrium; LV: left ventricle
FOLLOW-UP AND OUTCOME DATA
Median follow-up was 15.7 (3.0-49.6) months. One-year and three-year mortality of the study population was 19.1 and 26.3%, respectively.
Echocardiography at one-year follow-up was available in 153 patients (38.3%). In 63 of these (41%), EF dropped to <60% upon follow-up. Echocardiography at three-year follow-up was available for 124 patients (31%), with 51 patients (41%) showing an EF drop below 60%. Cardiac resynchronisation therapy (CRT), left ventricular assist device (LVAD) and heart transplantation were eventually performed in 17, one and one patients, respectively, upon long-term follow-up. The mean time to CRT implantation was 36±11 months. LVAD and heart transplantation were performed >5 and 6 years after index echocardiography, respectively.
Of 177 patients with AF, 19 (11%) underwent ablation procedures at a median of 38.3 (0.77-80.57) months after index echocardiography, and 43 (24%) received antiarrhythmics. Of 104 patients with CAD, revascularisation after the index echocardiography was performed in six patients (5.8%). The target vessel was left main stem in three patients, proximal left anterior descending artery in one patient and left circumflex artery in two patients. Revascularisation occurred within 30 days of the index echocardiography in three patients, and in the remaining three it occurred >1 year later.
After multivariable Cox proportional regression analysis, older age (HR per year increase 1.03, 95% CI: 1.02-1.05; p<0.001), >3+ MR (HR versus 3+ MR 1.45, 95% CI: 1.11-1.80; p=0.01), larger LA (HR per 10 mm increase 1.48, 95% CI: 1.17-1.69; p<0.001) and New York Heart Association functional Class III or IV (HR versus I or II 1.98, 95% CI: 1.40-2.60; p<0.001) were found to be significant independent predictors of cumulative mortality at last follow-up (Table 2). LA diameter was found to have a strong association with mortality, regardless of whether it was treated as a continuous (HR per 10 mm increase 1.48, 95% CI: 1.17-1.69; p<0.001) or categorical variable (HR of 4th [>52 mm] versus 1st [<41 mm] quartile 2.44, 95% CI: 1.81-3.06; p=0.001). The Kaplan-Meier curves for survival according to MR grade and LA diameter are shown in Figure 3 and Figure 4, respectively.
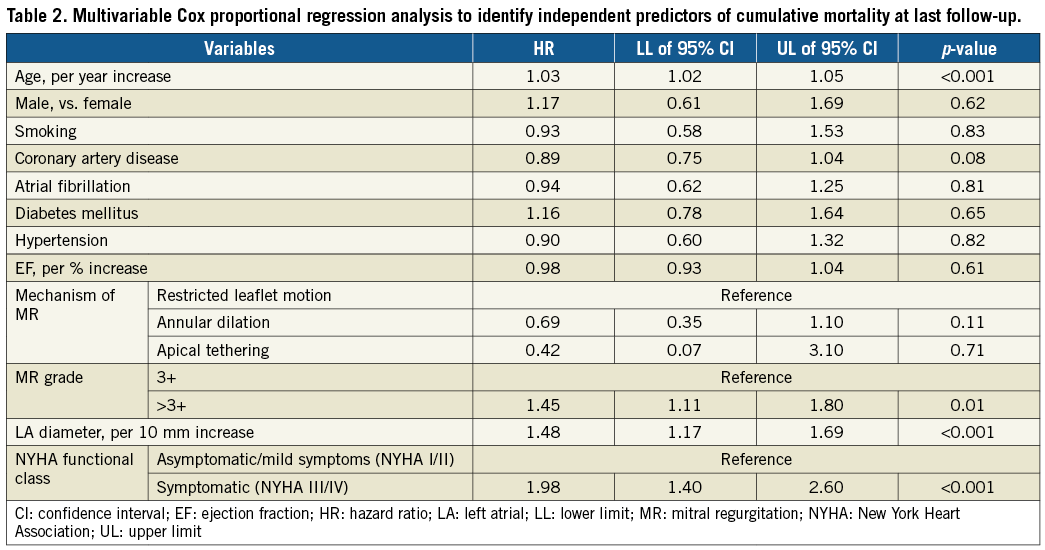
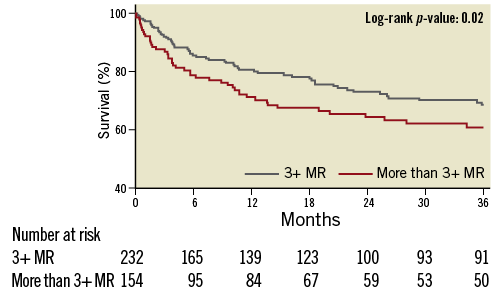
Figure 3. Kaplan-Meier curves showing long-term survival in patients with 3+ and >3+ MR. MR: mitral regurgitation
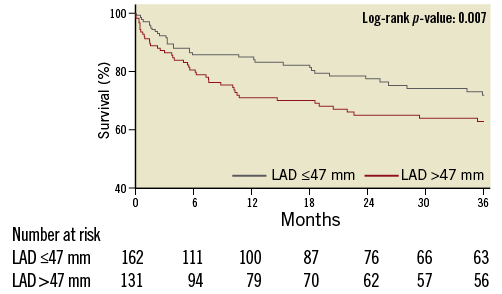
Figure 4. Kaplan-Meier curves showing long-term survival based on LA diameter. LA: left atrial
Discussion
The study describes the outcomes of a unique subset of secondary MR patients with normal LV systolic function. The study demonstrates a significant one-year and three-year mortality with medical management from the time of echocardiographic diagnosis. Other important findings include the association of older age, higher grade of MR, and larger LA size with mortality in this patient population.
In this study, the predominant secondary MR mechanism was restricted leaflet motion (91.5%), which, in the absence of organic MV disease or LV systolic dysfunction, emphasises the role of atrial remodelling in affecting proper MV function, whether by restricting MV leaflet movement or by causing annular dilation. The latter was the second most prevalent secondary MR mechanism identified in the study (4.5%). The extension of left atrial muscles into the leaflets of MV has been previously shown13-15. Atrial wall muscle spreads onto the surface of the MV in foetal life16. This finding has been reinforced by studies that demonstrated the electrical continuity of the mitral leaflets and the LA, highlighting the former as a possible origin for atrial dysrhythmias17. Further, the LA endocardium is the embryological origin of the posterior mitral leaflet18. As such, structural remodelling of the left atrium (LA), with the resulting atrial dilation and fibrosis, may be implicated not only in mitral annular dilation but also in restricted leaflet motion. In our study, the presence of atrial remodelling was demonstrated by the increased LA size (LA diameter 47±10 mm). While our study design lacks the ability to confirm whether this remodelling was a cause or an effect of the significant secondary MR, the absence of another echocardiographic explanation for the secondary MR provides at least circumstantial evidence for causality. In such cases, AF and LV diastolic dysfunction secondary to CAD, hypertension, or aging may explain the LA remodelling in the study population.
The main outcome evaluated in the study was mortality of the study population with conservative management. The analysis demonstrated that around one fifth of the patients (19.1%) died in the first year after echocardiographic diagnosis, and more than one fourth (26.3%) within three years. Notably, according to the Centers for Disease Control and Prevention, in 2000 and 2014, the annual mortality rates in the USA for people between 65 and 74 years of age were 2,980 per 100,000 (3.0%) and 2,176 per 100,000 (2.2%) for males, respectively, and 1,921 per 100,000 (1.9%) and 1,444 per 100,000 (1.4%) for females, respectively19. Interestingly, previous reports in patients with severe secondary MR and LV dysfunction demonstrated a comparable one-year mortality to our study population (20%) and a slightly higher three-year mortality (37%) with medical management20.
In a largely asymptomatic or mildly symptomatic population (82% of patients), with a relatively low prevalence of significant non-cardiac comorbid conditions, patients with more severe MR and larger LA diameter had significantly higher mortality. These findings were confirmed on multivariable regression analysis. This was an important finding given the relatively increased age of the population, which otherwise might have explained by itself the increased mortality in the study cohort. Further, outcomes and prognosis in patients with secondary MR due to severe LV dysfunction are believed to be more related to the underlying cardiomyopathy9, hence treatment is mainly guideline-directed medical therapy and cardiac resynchronisation therapy when indicated4,5. However, in patients with preserved LV systolic function, the study showed that possible underlying aetiologies for secondary MR, such as AF and CAD, did not have a similar impact.
There is a knowledge gap in the outcomes of transcatheter mitral valve intervention in patients with severe secondary MR and normal LV systolic function. This gap is unlikely to be addressed in the near future based on the current criteria, which mandate an EF ≤60% for inclusion of severe secondary MR patients in clinical trials evaluating transcatheter MV devices9. The ongoing Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients With Functional Mitral Regurgitation (COAPT) trial (ClinicalTrials.gov Identifier: NCT01626079) is including patients with LVEF ≥20% and ≤50%, which means that our study population would be excluded even in the presence of significant heart failure symptoms. Similarly, the Multicenter Study of Percutaneous Mitral Valve Repair MitraClip Device in Patients With Severe Secondary Mitral Regurgitation (MITRA-FR) (ClinicalTrials.gov Identifier: NCT01920698) is only recruiting patients with an EF between 15 and 40%. A third ongoing trial, A Clinical Evaluation of the Safety and Effectiveness of the MitraClip System in the Treatment of Clinically Significant Functional Mitral Regurgitation (Reshape-HF2) (ClinicalTrials.gov Identifier: NCT02444338), has an upper limit of 45% for EF in severely symptomatic patients. On the other hand, reports about commercial MitraClip® (Abbott Vascular, Santa Clara, CA, USA) use in secondary MR patients are showing that patients with EF >50% are being treated with the device in the real world21,22. The CARILLON Mitral Contour System for Reducing Functional Mitral Regurgitation (REDUCE FMR) trial (ClinicalTrials.gov Identifier: NCT02325830) will include patients with EF up to 50% and even with moderate (2+) MR, which will provide some insight into these patients but will not include completely normal EF patients. The inclusion of severe secondary MR patients with normal LV systolic function in future transcatheter mitral valve intervention trials would provide much needed answers regarding the possibility of improving the outcomes of this patient population. Importantly, given the insufficient data on the outcomes of the surgical treatment in these patients, mitral valve surgery is not the “gold standard” therapy. Hence, patients would not have to be “non-surgical candidates” to be included in percutaneous mitral valve intervention trials.
In summary, to our knowledge, this is the first study to evaluate the characteristics and outcomes of patients with severe secondary MR and normal LV systolic function, including the more recently recognised entity of AMR. Whether surgical or percutaneous MV intervention would have improved outcomes in this population is beyond the scope of the study, yet the observed findings raise a question about the perception of secondary MR without LV dysfunction as a relatively benign condition. The exclusion of patients with normal EF from clinical trials evaluating transcatheter interventions for secondary MR, based on most recent consensus9, would make an evidence-based answer to this concern unforeseeable in the near future. The findings also call for more research to understand the pathophysiological mechanisms, natural history and factors affecting the prognosis of AMR.
Study limitations
The current study has the inherent limitations of observational studies and potential for selection bias. The Cleveland Clinic is a tertiary referral centre; therefore, some patients may have been referred for further evaluation because of the identification of an atypical MR at other institutions. Although our study population was largely asymptomatic or mildly symptomatic, in those with significant symptoms the acuteness of presentation might have affected the severity of MR and the prognosis of patients. Further, there may be doubts about the homogeneity of the grading of the severity of MR throughout a period of 15 years where definitions of severity have varied. The study design lacks the ability to confirm whether LA remodelling was a cause or an effect of the significant secondary MR in patients with restricted leaflet motion and annular dilation. However, the lack of another explanation for severe secondary MR in this group of patients may suggest causality. The absence of a comparative arm is another limitation to a better interpretation of the results. Yet, we tried to overcome this limitation by providing internal comparisons based on MR severity and LA size. Whether percutaneous or surgical mitral valve intervention would alter the outcome of these patients remains unclear. Lastly, given the retrospective nature of the study, the completion of follow-up data remains a challenge. However, for our primary outcome of all-cause mortality, in addition to electronic medical records, we queried the US Social Security Death Index database to ensure the completeness and the accuracy of our outcomes.
Conclusions
Severe secondary MR with normal LV systolic function has significant mortality with conservative management. Older age, more severe symptoms, worse degree of mitral regurgitation and larger left atrium were independent predictors of mortality. This initial observation needs to be confirmed in larger prospective studies, and further studies are needed to establish optimal medical therapy in this setting. Further, inclusion of these patients, especially if symptomatic, in future transcatheter MV intervention trials may be warranted.
| Impact on daily practice Secondary mitral regurgitation in the setting of normal ejection fraction is not a well-studied entity and these patients are currently being excluded from clinical trials evaluating transcatheter mitral valve devices. Patients with severe secondary mitral regurgitation and normal left ventricular systolic function have significant mortality with medical management alone. Prospective studies evaluating transcatheter mitral valve intervention should include patients with severe secondary mitral regurgitation and normal ejection fraction. |
Conflict of interest statement
The authors have no conflicts of interest to declare.