Abstract
Aims: Limited data exist regarding procedural and clinical outcomes of percutaneous coronary intervention (PCI) in patients with trifurcation disease of the distal left main (LM) coronary artery. We therefore aimed to examine the procedural methods and early and late outcomes among patients undergoing distal LM trifurcation versus bifurcation PCI in the EXCEL trial.
Methods and results: Patients with distal LM bifurcation disease randomised to PCI with everolimus-eluting stents in the EXCEL trial were categorised into those with and without trifurcation involvement. Angiographic and procedural characteristics in addition to clinical events up to five-year follow-up after PCI were compared. Among 605 patients with site-reported distal LM disease, 61 patients (10.1%) were identified with trifurcation anatomy. The five-year primary composite endpoint of death, myocardial infarction, or stroke occurred in 16.6% of patients with trifurcation disease compared with 22.5% of patients with distal bifurcation disease only (p=0.32). Ischaemia-driven target lesion revascularisation rates were also similar (11.9% vs 12.0%, p=0.94). No significant differences in definite or probable stent thrombosis were observed between treatment groups (1.7% vs 2.3%, p=0.76).
Conclusions: Despite the greater inherent complexity, procedural and long-term clinical outcomes following PCI of distal LM trifurcations with everolimus-eluting stents in a modest-sized cohort from the EXCEL trial were similar compared with treatment of distal LM bifurcation disease without trifurcations. These findings support PCI as a treatment strategy for selected patients with distal LM trifurcation disease. ClinicalTrials.gov Identifier: NCT01205776
Introduction
Coronary artery disease involving the distal left main (LM) coronary artery bifurcation increases procedural complexity of percutaneous coronary intervention (PCI) and is associated with worse outcomes compared with isolated ostial or shaft LM disease1,2. Despite extensive analysis of PCI techniques and clinical outcomes after distal LM bifurcation treatment, few reports have examined procedural strategy and outcomes in patients with trifurcation disease of the distal LM artery segment. Among such studies, procedural and early clinical outcomes appear favourable3,4,5,6, yet late-term adverse event rates are high and correspond with increasing trifurcation disease complexity and number of stents used5,6.
Whether contemporary outcomes in LM trifurcation PCI are similar to distal bifurcation disease using contemporary techniques and drug-eluting stents has not been characterised. We therefore examined the procedural methods and early and late outcomes among patients undergoing distal LM trifurcation versus bifurcation PCI in the EXCEL (Evaluation of XIENCE Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularisation) trial.
Methods
TRIAL AND STUDY POPULATION
The design, enrolment criteria, methods and principal outcomes of the EXCEL trial have been reported previously7. EXCEL was an international, large-scale, open-label, multicentre trial in which 1,905 patients with LM disease and low or intermediate SYNTAX scores (≤32) eligible for both PCI and coronary artery bypass surgery (CABG) as assessed by a site-based Heart Team were randomised to treatment with cobalt-chromium alloy fluoropolymer-based everolimus-eluting stents (XIENCE; Abbott Vascular, Santa Clara, CA, USA) or bypass graft surgery. The study was approved by the institutional review board or ethics committee at each enrolling site, and consecutive, eligible patients signed written informed consent prior to the revascularisation assignment.
Patients with site-reported distal LM disease (LM distal diameter stenosis [DS] >50%) were included in this analysis and compared relative to the presence of trifurcation versus “only” bifurcation disease as assessed by an independent angiographic core laboratory (Cardiovascular Research Foundation, New York, NY, USA). Treatment approaches to LM trifurcation or bifurcation disease (e.g., use of single versus multiple stents, provisional one-stent vs planned two-stent technique, predilation and post-dilation) were left to the discretion of the operator. If side branch post-dilation was required, the protocol recommended implanting an additional stent if, after a kissing balloon inflation, either a severe dissection (≥grade B), Thrombolysis In Myocardial Infarction (TIMI) flow <3, or a severe stenosis was present (>70% angiographic DS, minimal luminal area by intravascular ultrasound [IVUS] ≤4.0 mm2 with plaque burden >60%, or fractional flow reserve ≤0.80). Proximal optimisation and kissing balloon inflations were recommended in cases of multiple stents or if side branch post-dilation was required.
STUDY ENDPOINTS AND DATA MANAGEMENT
The primary endpoint was the composite rate of death, myocardial infarction (MI), or stroke at three-year follow-up. Major secondary endpoints included death, MI, or stroke at 30 days, and the composite rate of death, MI, stroke, or ischaemia-driven revascularisation (IDR) at three years. Study endpoint definitions and qualifying criteria have been described previously5. The case report form collected site-assessed stenosis severity and location within the different regions of the LM and, in cases in which the distal LM bifurcation or trifurcation was involved (>50% visually assessed DS), the number of stents used to treat the LM segment. An independent clinical events committee adjudicated all primary and secondary endpoints following review of original source documents.
STATISTICAL ANALYSIS
The present analysis was pre-specified in the original study protocol. All patients with site-assessed distal LM bifurcation and trifurcation disease randomised to and treated with PCI were included, and patient groups were compared according to intended treatment.
Baseline characteristics of study patients were summarised in terms of frequency and percentage for categorical variables and by mean with standard deviation for continuous variables. Categorical variables were compared by χ2 or Fisher’s exact test if >20% of the expected cell frequencies were <5. For continuous variables that met the assumption of normality by the Shapiro-Wilk test, the two treatment groups were compared by the two-sample t-test. If the data failed to meet the assumption for normality, comparisons were made using the Wilcoxon rank-sum test. Five-year clinical events were summarised as Kaplan-Meier estimates. Odds ratios, 95% confidence intervals and p-values were determined using logistic regression including follow-up days as a log-transformed offset term. Multivariable analysis was performed in order to adjust for the influence of potential confounders on the relationship between distal LM anatomy and composite adverse events at five years using the following covariates: trifurcation versus no trifurcation, age, male sex, recent MI (<7 days), current smoker, diabetes, creatinine clearance <60 mL/min, SYNTAX score, concomitant LM ostial or shaft DS >50%, worst LM %DS, ostial left anterior descending (LAD) %DS, ostial left circumflex (LCX) %DS, TIMI flow <3 in either the LAD or LCX artery, and left ventricular ejection fraction (LVEF). All angiographic measures in the model were determined by angiographic core laboratory assessment. A two-sided p-value of 0.05 was established as the level of statistical significance for all superiority tests. All analyses were performed with SAS software, version 9.4 (SAS Institute, Cary, NC, USA).
Results
CLINICAL AND ANGIOGRAPHIC CHARACTERISTICS
Among 605 patients with site-reported distal LM bifurcation disease (DS >50%), 61 patients (10.1%) had distal trifurcation anatomy. No significant differences were present in the baseline clinical or demographic characteristics between the groups other than a higher prevalence of prior PCI in the bifurcation only group and greater LVEF in the trifurcation cohort (Table 1). Presentation with unstable angina or MI as well as a history of MI was non-significantly higher among bifurcation only patients. Approximately one fourth of the overall study population had diabetes mellitus.
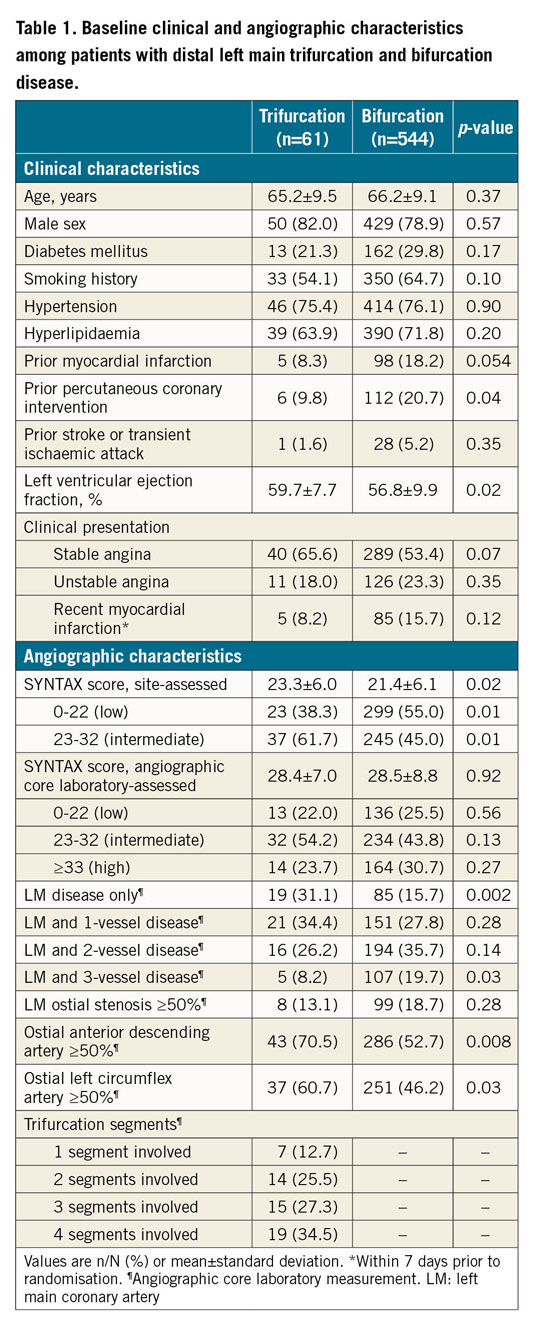
The baseline SYNTAX score was significantly higher among trifurcation patients by site estimation, but not by angiographic core laboratory assessment (Table 1). The presence of isolated LM disease was significantly more common in the trifurcation group, whereas the prevalence of LM and three-vessel coronary artery disease was significantly more frequent in the bifurcation only group. Among those with trifurcation anatomy, disease involvement (DS ≥50%) of at least three segments was present in more than half of the patients.
PROCEDURAL CHARACTERISTICS AND OUTCOMES
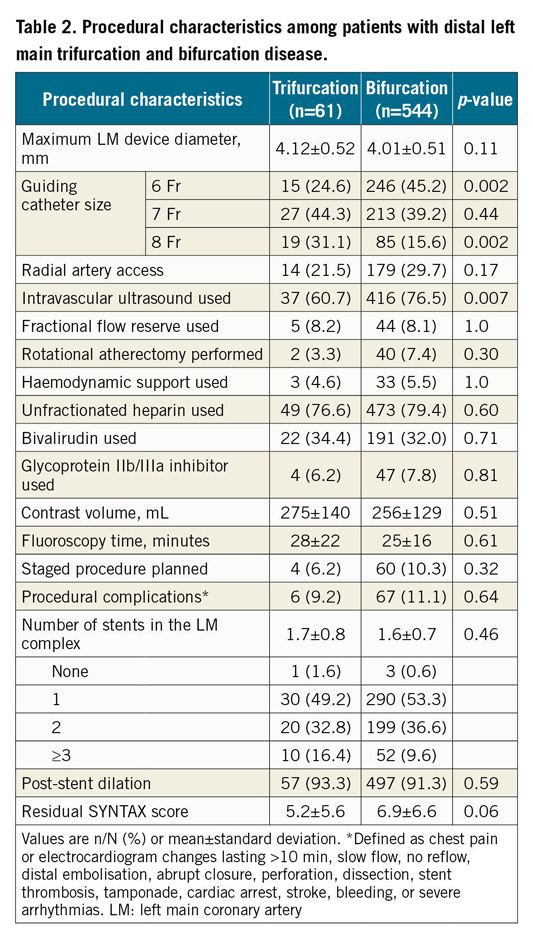
6 Fr guiding catheters were used more frequently in bifurcation only procedures, whereas 8 Fr guiding catheter use was more common in trifurcation cases (Table 2). IVUS guidance was used more frequently in bifurcation only cases. Use of haemodynamic support devices, procedure duration, and site-reported procedural complications did not differ between treatment groups. The average number of stents used to treat the LM complex (the distal LM, ostial LAD, ostial LCX and, in trifurcation disease, ostial ramus) was also similar among trifurcation and bifurcation only cases, although treatment with three or more stents was numerically higher in the trifurcation cohort (16.4% vs 9.6%, p=0.09). Despite differences in the prevalence of multivessel coronary disease, there was no significant difference in the post-PCI residual SYNTAX score between groups.
CLINICAL OUTCOMES
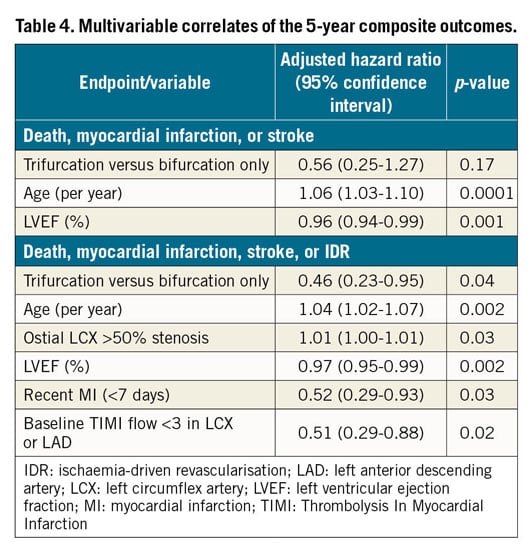
Adverse event rates within 30 days were infrequent and not statistically different between the two groups (Table 3). At five years, no significant differences were identified between trifurcation and bifurcation only patients regarding the primary endpoint of death, MI, or stroke (16.6% vs 22.5%, p=0.32, respectively) (Table 3, Figure 1A) or the composite endpoint of death, MI, stroke or IDR (21.5% vs 32.6%, p=0.11, respectively) (Table 3, Figure 1B). The five-year rates of IDR of the LM complex and any MI were also similar between groups. In multivariable analysis, the presence of trifurcation versus bifurcation only disease was not identified as a predictor of the composite primary endpoint but was a significantly negative predictor of death, MI, stroke or IDR at five years compared with bifurcation only disease (Table 4). Definite or probable stent thrombosis up to five years occurred in 1.7% and 2.3% of trifurcation and bifurcation only patients, respectively (p=0.76). Adherence to dual antiplatelet therapy at five years was 45.8% among trifurcation patients and 57.1% in bifurcation only patients (p=0.13).
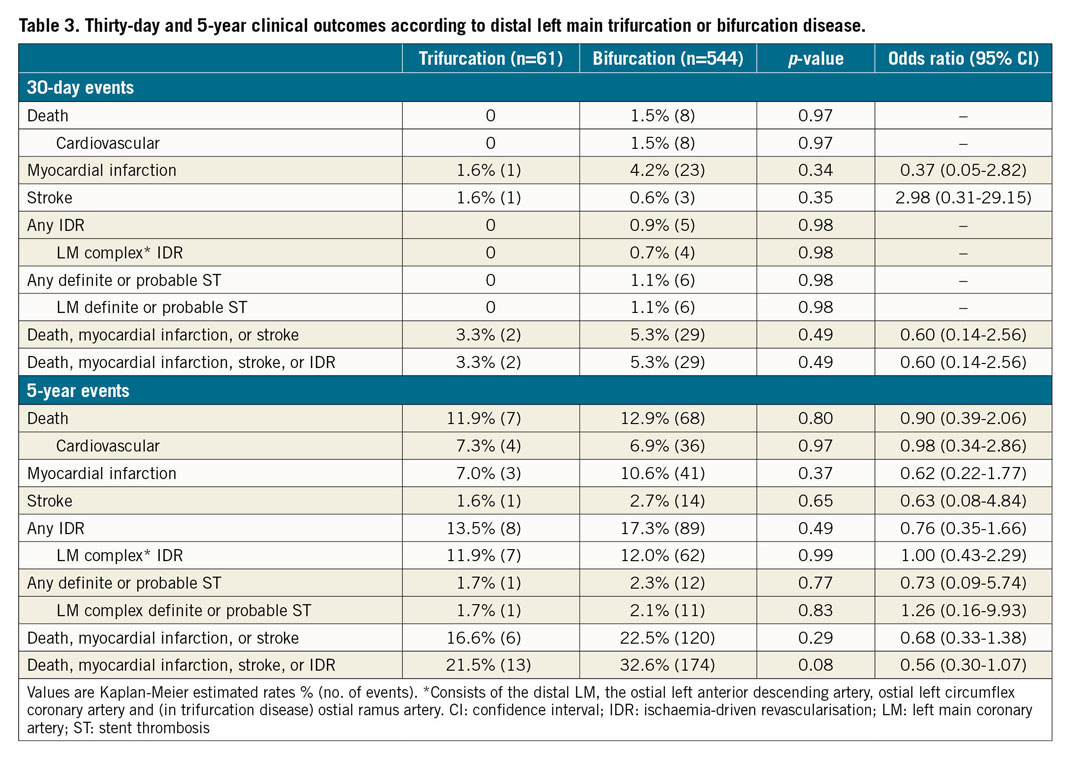
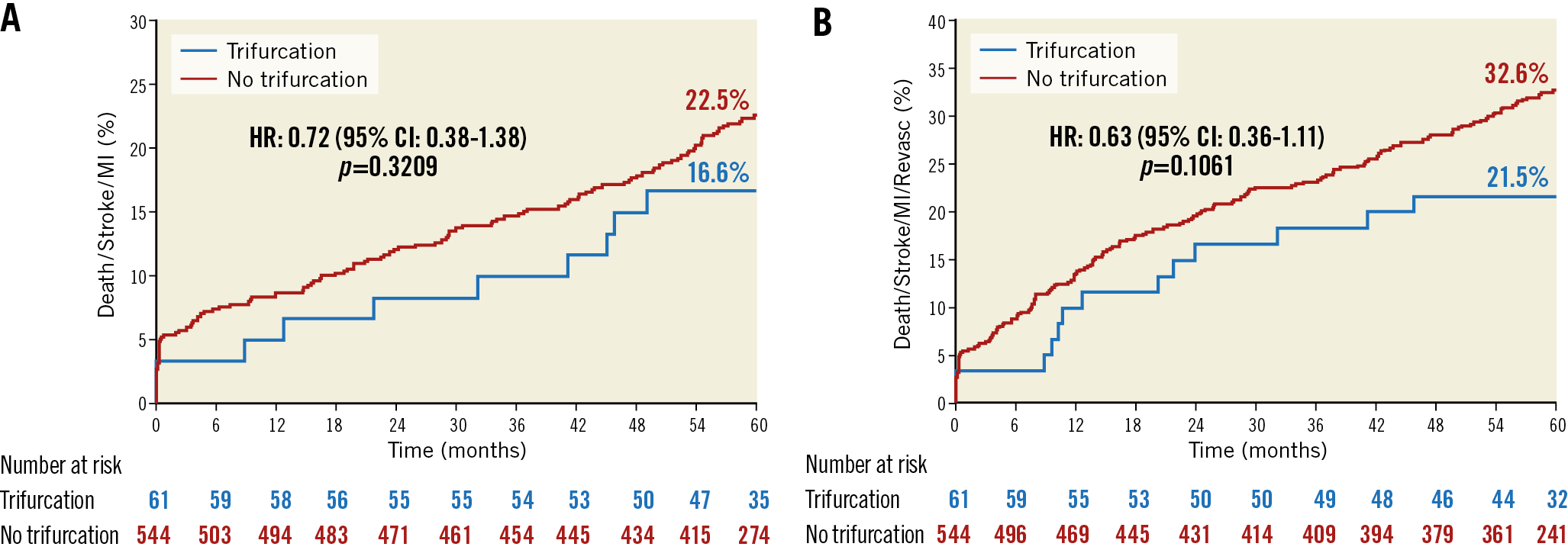
Figure 1. Five-year outcomes following percutaneous coronary intervention for patients with distal left main trifurcation disease versus bifurcation only disease. A) The composite rate of death, myocardial infarction (MI), or stroke. B) Composite rate of death, MI, stroke, or ischaemia-driven repeat revascularisation. CI: confidence interval; HR: hazard ratio
Discussion
Limited evidence exists to inform procedural methods and clinical outcomes using contemporary techniques and drug-eluting stents for patients with LM trifurcation disease. Among patients with distal LM disease randomised to PCI in the EXCEL trial, trifurcation involvement was identified in ~10% of cases. Despite greater lesion complexity associated with trifurcation anatomy, procedural and early clinical outcomes were similar to those of patients undergoing PCI of the distal LM bifurcation only. Up to five years, event-free survival also did not differ significantly between trifurcation and bifurcation only groups, with late-term repeat revascularisation rates among trifurcation patients representing a considerable improvement compared with historical studies. More specifically, over five-year follow-up, rates of both all-cause and cardiovascular death, in addition to the cumulative incidence of LM complex IDR and MI, were similar to those of patients treated for distal LM bifurcation only disease. In multivariable analysis, the presence of LM trifurcation disease compared with distal bifurcation only disease was associated with a significantly lower incidence of death, MI, stroke or IDR. Altogether, these findings support PCI as a treatment strategy for selected patients with distal LM trifurcation disease.
LM trifurcation anatomy introduces unique technical and procedural challenges beyond bifurcation disease alone given the variability in disease distribution (1 to 4 diseased segments), side branch angulation, and the implications of carinal shift. In the present study, >70% of patients had significant disease involving ≥3 segments of the trifurcation, and the additive contribution of trifurcation disease to anatomic complexity is reflected by a similar overall SYNTAX score to that of patients with distal bifurcation disease despite a lower incidence of multivessel disease among trifurcation patients. As a result of the differential plaque burden in trifurcation disease, stent number and performance of two-step kissing balloon inflation or triple kissing inflation are variable. However, consistent with contemporary bifurcation strategies that favour a provisional single-stent approach8,9,10, the average number of stents to treat the LM complex was similar among the trifurcation and bifurcation only groups, demonstrating operator intent to avoid multiple stents if possible.
Previous studies examining outcomes following LM trifurcation PCI have reported rates of major adverse events ranging from 19% to 34% over a follow-up period of approximately 1 to 5 years (Supplementary Table 1),3,4,5,6,11,12. In most prior studies, first-generation drug-eluting stents were predominantly used, and the composite endpoint was principally driven by repeat revascularisation that occurred in 19% to 32% of patients. In selected studies, the likelihood for repeat revascularisation escalated with increasing trifurcation disease complexity and number of stents used5,6. In comparison, the 11.9% rate of LM repeat revascularisation over five years is not only similar to the observed rate for bifurcation only disease, but also represents a considerable improvement by indirect comparison with historical reports. It is likely that the use of contemporary thin-strut everolimus-eluting stents contributed to these favourable outcomes, although greater application of the provisional strategy and other unmeasured variables may also be related. Surprisingly, use of IVUS was less common among trifurcation cases, an unexpected observation given the potential for multiple overlapping stent segments and increased likelihood for compromised luminal dimensions secondary to carinal shift13. Even better outcomes may have been achieved had IVUS guidance been used more frequently14,15.
Study limitations
The EXCEL trial has many strengths, including its large size and international representation, use of contemporary devices and techniques, complete patient monitoring, and utilisation of independent angiographic core laboratories and clinical events committees to assess outcomes rigorously. Nonetheless (and consistent with prior reports), the modest-sized cohort of LM trifurcation patients limits definite conclusions related to low-frequency events. Whether the absence of difference in outcome between trifurcation and bifurcation groups was influenced by a significantly higher incidence of three-vessel disease and trend towards higher residual SYNTAX score in the bifurcation cohort is undetermined. Indeed, in multivariable analysis, trifurcation disease was associated with a significantly lower composite outcome of death, MI, stroke or IDR despite similar rates of LM-specific IDR between cohorts. In addition, the present analysis was performed principally from the operator’s perspective to be relevant to catheterisation laboratory decisions, and treatment strategy and procedural methods were exclusively investigator determined. The potential influence of selected procedural methods that were not recorded in the database (e.g., stent technique [culotte, double kiss crush, T-stent] or use of the proximal optimisation technique) cannot be determined. Similarly, patients with site-reported LM trifurcation disease were included in this report and therefore subject to limitations of angiographic interpretation of complex distal LM anatomy. Further, despite multivariable analysis, differences in outcomes may have been influenced by unmeasured confounders not collected in the case report form. Finally, the EXCEL trial restricted enrolment to selected patients with LM disease and a SYNTAX score ≤32. In addition, the trifurcation lesions enrolled in EXCEL were carefully selected, i.e., those which the operators estimated to have a high likelihood of procedural success. The present results may therefore not be applicable to patients with high SYNTAX scores and highly complex LM trifurcations not represented in this trial.
Conclusions
In summary, in the EXCEL trial, despite the inherent complexity of PCI in distal LM lesions with trifurcation involvement, the PCI procedural technique (including the number of stents used) was similar to treatment of bifurcation only disease. Event rates including cardiac death, IDR, stent thrombosis and the primary composite endpoint of death, MI, or stroke were similar in patients with trifurcation and bifurcation only disease of the distal LM at 30-day and five-year follow-up. These findings support PCI as an acceptable treatment strategy for selected patients with distal LM trifurcation disease.
|
Impact on daily practice Despite greater lesion complexity associated with trifurcation anatomy, early and late clinical outcomes following PCI with everolimus-eluting stents were similar compared with those of patients undergoing PCI of distal LM bifurcation disease without trifurcations. These findings support PCI as an acceptable treatment strategy for selected patients with distal LM trifurcation disease. |
Guest Editor
This paper was guest edited by Fernando Alfonso, MD; Hospital Universitario de La Princesa, Madrid, Spain.
Funding
Abbott Vascular, Santa Clara, CA, USA.
Conflict of interest statement
D. Kandzari reports grants and personal fees from Biotronik, Medtronic, and Boston Scientific. P. Serruys reports personal fees from Abbott Laboratories, AstraZeneca, Biotronik, Cardialysis, GLG Research, Medtronic, Sino Medical Sciences Technology, Société Europa Digital & Publishing, Stentys France, Svelte Medical Systems, Philips/Volcano, St. Jude Medical, Qualimed, and Xeltis. M. Leon reports grants and personal fees from Medtronic, Boston Scientific and Abbott, personal fees from Gore Medical and Meril Life, and grants from Edwards Lifesciences. C. Simonton is an employee of Abiomed. N. Lembo reports personal fees from Abbott Vascular, non-financial support from Boston Scientific, Medtronic Vascular, and Abiomed. S. Mansour reports grants and personal fees from Abbott Vascular. M. Sabaté reports grants from Abbott Vascular. J. Sabik reports personal fees from Medtronic, and grants from Edwards and Abbott. A.P. Kappetein is an employee of Medtronic. G. Stone reports grants from Abbott, personal fees from Terumo, Amaranth, Shockwave, Valfix, TherOx, Reva, Vascular Dynamics, Robocath, HeartFlow, Gore, Ablative Solutions, Matrizyme, Miracor, Neovasc, V-wave, Abiomed, Claret, Sirtex, SpectraWaveAncora, Qool Therapeutics, MAIA Pharmaceuticals, Orchestra Biomed, and Novartis; equity/options from Ancora, Qool Therapeutics, Cagent, Applied Therapeutics, Biostar family of funds, MedFocus family of funds, SpectraWave, Orchestra Biomed, and Aria. The other authors have no conflicts of interest to declare. The Guest Editor has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.