Ostial lesions represent a challenging setting for percutaneous coronary artery intervention (PCI), requiring an in-depth understanding of the underlying anatomy and precise handling of a large variety of interventional tools and techniques. This subset includes, by definition, all lesions arising within 3 mm of the origin of a coronary vessel, encompassing a broad spectrum of pathologies according to lesion location: (1) aorto-ostial lesions, (2) non-aorto-ostial lesions, and (3) side branch ostial lesions1.
Lesions involving the origin of the left main (LM) coronary artery are classified as aorto-ostial lesions. Frequently fibrotic and calcified, extending proximally into the aortic wall where thick muscular and elastic fibres are prominent, these lesions present high resistance to dilatation and are prone to recoil. Therefore, in the balloon angioplasty era, treatment of aorto-ostial lesion was associated with lower angiographic success, higher rates of repeat revascularisation, and higher incidence of procedural complications such as acute dissection, vessel closure and myocardial infarction (MI), jeopardising a large area of myocardium2. The breakthrough came with the routine use of stenting, which led to improvements in clinical outcomes, although the rate of repeat revascularisation remained high compared to non-aorto-ostial lesions. The development of plaque modification devices, the introduction of drug-eluting stents (DES), and the implementation of intravascular imaging finally turned the tables3. Hence, in the DES era, technological refinements have allowed PCI to achieve comparable long-term outcomes with coronary artery bypass graft (CABG) for isolated ostial/mid-shaft LM lesions. Lesion location is currently considered a relevant factor in determining the choice of revascularisation strategy in patients presenting LM disease4. A prespecified analysis of the EXCEL (Evaluation of XIENCE versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization) trial showed no difference in the primary endpoint of death, stroke, or MI between PCI or CABG at 3-year follow-up, regardless of lesion location and SYNTAX (Synergy between PCI with TAXUS and Cardiac Surgery) score, although a higher rate of ischaemia-driven revascularisation was observed with PCI versus CABG in patients with bifurcation disease5. In a recent meta-analysis including randomised trials and adjusted observational studies, PCI and CABG showed similar rates of major adverse cardiac events in patients with ostial/mid-shaft LM disease, whereas revascularisation with CABG led to improved outcomes in the setting of distal LM bifurcation disease6. Few real-world studies have compared the outcomes of LM PCI according to lesion location. A small multicentre study including 147 consecutive patients undergoing PCI with first-generation DES for ostial/mid-shaft LM stenosis (almost 50% with intravascular ultrasound guidance) reported promising long-term outcomes (7.4% rate of major adverse cardiovascular events and 0.7% target lesion revascularisation [TLR] at 2-year median follow-up)7. In the large DELTA (Drug-Eluting Stent for Left Main Coronary Artery Disease) registry (1,612 patients included: 482 with ostial/mid-shaft versus 1,130 with distal LM bifurcation lesions), PCI of ostial/mid-shaft lesions essentially using first-generation DES was associated with improved long-term (>3-year median follow-up) clinical outcomes compared to distal bifurcation lesions, mainly due to lower rates of repeat revascularisation (TLR 4.5% vs 10.9%; propensity score adjusted hazard ratio [HR] for distal bifurcation versus ostial/shaft lesions: 1.68, 95% confidence interval [CI]: 1.19-2.38; p<0.003). Despite representing the largest available real-world evidence to date, the DELTA registry did not allow a direct comparison of pure ostial lesions with other anatomical subsets of LM disease8.
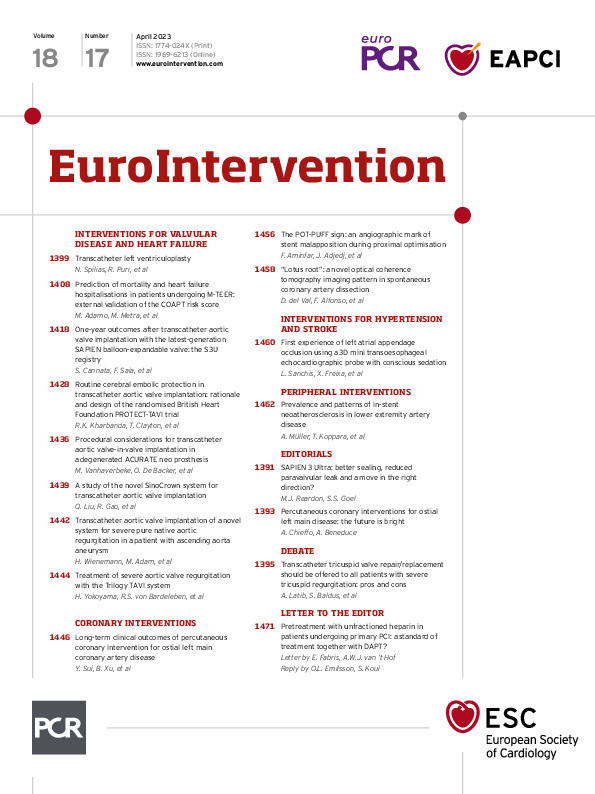
In the current issue of EuroIntervention, Sui et al9 evaluate long-term outcomes of PCI for isolated ostial LM lesions compared to mid-shaft or distal LM bifurcation lesions in a large real-world registry including 4,625 patients from the People's Republic of China. Among patients treated with DES (97.8% of the study population, with 75.9% receiving second-generation platforms), LM PCI was associated with a low and acceptable 3-year rate of the primary composite endpoint of target vessel failure (TVF), regardless of the lesion location (7.5% in ostial, 6.8% in mid-shaft and 9.0% in bifurcation groups). However, the ostial group exhibited a significantly lower 3-year incidence of MI (2.0% vs 4.2%; p=0.02) and target vessel MI (1.8% vs 3.9%; p=0.02) compared to the distal bifurcation group. This difference was already evident at 30-day follow-up and was not paralleled by a difference in long-term repeat revascularisation or stent thrombosis, hinting at the procedural complexity of bifurcation PCI (regardless of stenting strategy) and strict definition of MI as a major explanation for this finding. Major procedural complications (dissection, perforation, slow flow/no flow, major side branch occlusion) were similar among the groups and predicted cardiac death or MI at follow-up in patients with ostial LM disease (HR 4.62, 95% CI: 1.34-15.8; p=0.02), while the year of procedure was a protective factor for those events (HR 0.91, 95% CI: 0.83-0.99; p=0.04).
The authors should be commended for performing the largest available analysis of real-world data comparing LM PCI outcomes according to lesion location. Their effort allowed an accurate evaluation of ostial LM lesions as an independent anatomical subset, therefore adding granularity to the field. Nevertheless, several aspects deserve consideration. Overall, the results of this study are encouraging, showing favourable long-term outcomes for LM PCI across different lesions subgroups, including distal LM bifurcation lesions. However, the lower than previously reported long-term events rate could partly be a consequence of the low-risk population included in this study. Similarly, the anatomical complexity of patients presenting with distal LM bifurcation identified by the SYNTAX score was lower than reported in previous studies (23.8% vs 27.9% in the EXCEL trial and 29.7% in the DELTA registry), with a consequently lower use of two-stent strategies (27.2% vs 43.8% in the EXCEL trial and 40.7% in the DELTA registry) that might have positively affected outcomes58. On the other hand, significant differences in 30-day and 3-year MI rates might be overemphasised by the use of low biomarker elevation thresholds to identify those events. Indeed, although recent analyses of the SYNTAX and EXCEL trials have suggested that a definition of procedural MI based on large biomarker elevation (peak creatine kinase-myocardial band [CK-MB] >10 times the upper limit of normal [ULN]) alone (without additional evidence of myocardial ischaemia) might be useful in identifying prognostically meaningful PCI-related events associated with 5-year cardiac and 10-year all-cause mortality, the definition proposed in the current study (peak CK-MB >2 times ULN) seems excessively inclusive1011. Although the absence of detailed data on procedural techniques represents a major limitation of this study, the most encouraging finding comes from the observation that clinical outcomes of PCI for ostial LM lesions improved over time during the study period (from 2004 to 2014). After the enrolment of the last patient in this study almost 10 years ago, PCI for ostial LM lesions has dramatically progressed: procedural techniques have evolved to allow accurate stent positioning and minimise geographical miss, modern DES with high radial strength and wider expansion ranges have entered the market, dedicated ostial flaring balloons have been developed, and intravascular imaging has been largely implemented in clinical practice to optimise procedural results. Moving from these premises, further studies will clarify how well contemporary refinements are paving the way to a bright future for PCI in this historically challenging setting.
Conflict of interest statement
A. Chieffo received speaker and/or consultant fees from Abiomed, Boston Scientific, Biosensor, Medtronic, Menarini, and Shockwave Medical. A. Beneduce received speaker honoraria from Boston Scientific.