Abstract
The left main is the largest bifurcation of the coronary tree and is, therefore, easier to access. Nevertheless, the risks of untoward consequences associated with the loss of the side branch are much higher. Although the usual technical strategies implemented in coronary bifurcations can generally be applied to left main lesions, several inherent characteristics (the ostial position of the main branch, the size of the side branch, the amount of calcification, the angle which is often in a T shape, the use of stents of variable suitability, the crucial role of POT) need to be taken into account in order to achieve optimal acute and long-term results.
Introduction
Percutaneous coronary intervention (PCI) with drug-eluting stents (DES) is increasingly recognised as a valid revascularisation alternative to coronary artery bypass surgery (CABG) in patients with significant left main (LM) disease1-3. Furthermore, recent studies have shown that patients with low or intermediate coronary complexity as assessed by the SYNTAX score have comparable outcomes with PCI and CABG4, for up to five years5. More recently, when including clinical data in the risk prediction, as assessed by the SYNTAX score II6, PCI seems to have a better four-year outcome than CABG in certain patient subgroups. With experienced operators and an optimal technical approach, LM PCI today is at least as safe as CABG in patients with a low or intermediate SYNTAX score and has accordingly been upgraded to a class Ib indication in patients with a low SYNTAX score in the latest European Society of Cardiology/European Association for Cardio-Thoracic Surgery guidelines7.
Most LM lesions are bifurcation lesions (65 to 80% of cases) as defined by the latest European Bifurcation Club consensus8 and, as such, they require the same practical and technical approach as any bifurcation lesion (Online Figure 1), namely adequate support, appropriate visualisation of the bifurcation and side branch (SB) ostium (working view), compliance with the coronary branching law (Figure 1), analysis of the three diameters, implementation of the provisional strategy whenever feasible (Figure 2), initiation of the procedure with two wires, optimal selection of the main branch (MB) stent and of its diameter (in relation to the distal MB reference diameter), proximal optimisation technique (POT) before guidewire exchange, distal strut opening toward the SB (Online case example 1), SB stenting when needed, and sometimes SB stenting first when its access is difficult.
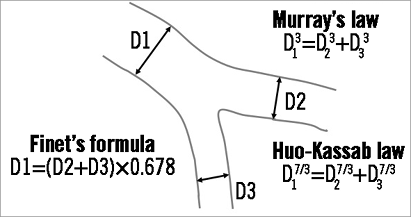
Figure 1. Different main structure-function scaling laws of vascular trees.
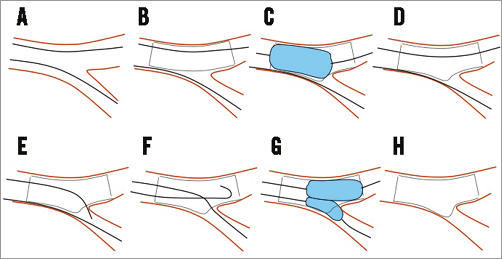
Figure 2. Provisional side branch LM stenting approach, step by step. A) Two wires in each branch. B) Stent from LM to LAD (diameter according to LAD). C) POT. D) Favourable stent deformation after POT. E) “Pullback” technique to enter distal strut. F) Wire exchange. G) Kissing balloon inflation with two short NC balloons. H) Final result.
The LM is, however, the largest bifurcation of the coronary tree and has a number of unique specificities, which may require a different technical approach compared to other coronary bifurcations which are more distal in the coronary tree:
The myocardium supplied by the LM generally accounts for considerably more than 50% of the total myocardial mass. Technical inadequacies may, therefore, seriously affect not only the procedure, but also the long-term outcome.
The SB is the circumflex artery (LCx) in most instances. It generally has a large diameter and is not always easily accessible, especially after MB stenting. In cases where the LAD has a 3.5 mm diameter and the LCx a 3 mm diameter, the percentage of myocardial necrosis following occlusion of the LCx is approximately 70% compared9 to the occlusion of the proximal segment of the LAD. This may furthermore induce acute ischaemic mitral regurgitation. The occurrence of LCx occlusion is therefore not acceptable.
The LM is the only bifurcation where the proximal MB originates directly from the aorta. This is a major specificity with numerous strategic and technical implications, which will be addressed later.
With a proximal reference diameter generally measuring between 4 and 5 mm, this type of bifurcation is rather large considering the size of currently available coronary stents.
The aspect of diffuse LM disease may be misleading10 and may appear “normal” or disease-free to an inattentive eye. Bearing in mind the principles of the branching law allows the identification of diffuse LM disease when the reference diameter of the LM is identical to that of the LAD.
Trifurcations are encountered in about 10% of cases11,12 and may require specific treatment strategies.
The pattern of atheroma development in the LM is the same13 as in any bifurcation (formation of atheroma in areas opposite the flow divider) but with a more disseminated distribution14. Though the nature of atheroma seems to be different15, the inherent implications are still unknown. It appears, however, that plaque distribution may influence long-term prognosis16.
The presence of calcification in the LM is a frequent occurrence, given the mean age of patients with LM disease (about 68 years in most series).
The bifurcation angle is generally T-shaped, which may have an impact on prognosis17,18 after stenting.
Numerous studies have shown that incomplete revascularisation is associated with a higher risk of short-term and midterm MACE. The recently developed concept of the residual SYNTAX score has highlighted the significantly increased risk associated with scores >819,20. This is even more relevant in patients with LM disease in whom untreated chronic occlusion of the right coronary artery is associated with a higher mortality risk21-23.
The practical aspects will be addressed in the sections which follow.
The largest bifurcation of all
The fact that the reference diameter of the LM is usually >4 mm and is located in a proximal segment constitutes both an advantage and a disadvantage. On the one hand, it makes stent delivery easier, even in calcified lesions. This is particularly interesting when using dedicated stents whose deliverability is inferior to that of traditional stents24-27, especially in more distal lesions.
On the other hand, the proximal location of the LM may generate a number of issues.
Should the proximal segment of the stent always involve the LM ostium? As a general rule, in the presence of a long LM whose proximal segment is free of atheroma, it is not necessary to position the stent as far up as the ostium, provided that the segment of the stent proximal to the carina is longer than the shortest balloon available in the cathlab for performing POT (in order to avoid geographical miss and the subsequent increased risk of restenosis). In a short LM or in the presence of diffuse atheromatous disease (Online case example 2), it is strongly recommended that LM stenting should involve the ostium and that ostial coverage should be checked (Figure 3) in a 40° cranial view (between RAO 10° and LAO 10°). Ostial stent positioning may create several technical problems such as stent malapposition with the additional risk of inserting a wire between the external wall of the stent and the arterial wall (Online case example 3), risk of longitudinal stent distortion (Online case example 4) during guiding catheter engagement, removal of the jailed wire from the SB (Online Figure 2) or removal of an incompletely deflated stent delivery balloon. In all these cases, the role of POT is crucial in allowing stent apposition to the arterial wall and preventing the occurrence of the complications described above.
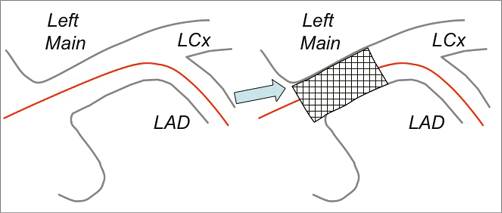
Figure 3. Optimal view for left main ostium positioning. In order to obtain an optimal ostium scaffolding, it is very important to check the upper part of the ostium (the lower part of the stent will protrude a little bit in the aorta).
Selection of the guide size may vary according to each operator’s preference. In Europe, most LM bifurcations are treated using a provisional SB stenting strategy with a 6 Fr guiding catheter. However, in some cases (large LM reference, trifurcation) a 7 or 8 Fr guide may be preferred.
Stent selection is also crucial, as is the accurate assessment of the maximal stent expansion capacity. This has been very well demonstrated by Nicolas Foin28 using virtual bench testing (Figure 4).
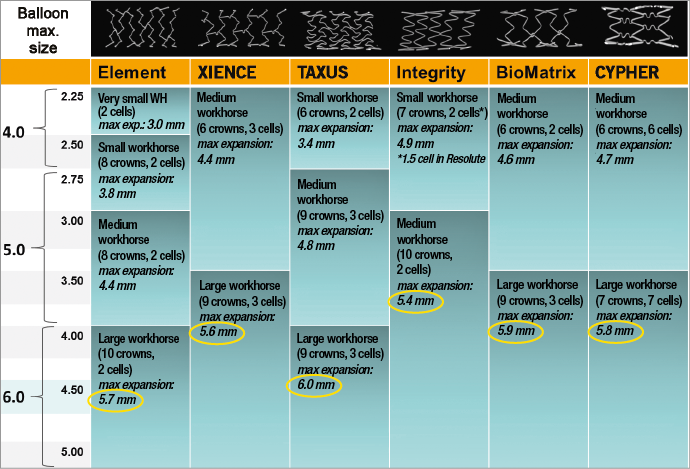
Figure 4. Maximal diameter of main drug-eluting stents in a virtual bench.
How to avoid losing the circumflex coronary artery
It is essential that strategies should be implemented not only to avoid the occurrence of occlusion but also to reopen an occluded LCx efficiently. Respecting the branching law is essential for ensuring adequate prevention (Online case example 5). The stent diameter should be selected according to the distal reference diameter in order to avoid pushing the carina towards the ostium of the circumflex. Once the stent has been appropriately deployed, POT should be carried out in order to ensure apposition of the proximal segment of the stent proximal to the carina and to facilitate guidewire access to the SB through the stent struts, which are opened by POT proximal to the carina. Balloon positioning is crucial for performing POT. Use of balloons with two markers is required and the distal marker should be positioned in front of the carina.
Optimal visualisation is obviously necessary to check the position of the balloon with respect to the carina.
In the unlikely event that occlusion should occur despite all the precautions described above, and if attempts to re-cross using various wires (Fielder FC, Fielder XT; ASAHI Intecc, Aichi, Japan, etc.) prove unsuccessful, the implementation of POT at higher pressure may restore flow in the SB and facilitate guidewire insertion (Figure 5).
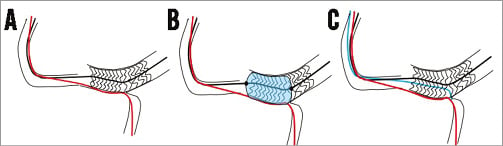
Figure 5. POT may facilitate side branch access. A) Difficult side branch access secondary to carina shifting. B) POT will enlarge the stent (and the struts towards the side branch), proximal to the carina. C) Use of a third wire to access the side branch through the main branch stent.
Should these manoeuvres be of no avail, the jailed wire can be used with a small diameter balloon to restore flow in the SB and facilitate guidewire passage through the struts of the MB stent (Figure 6).
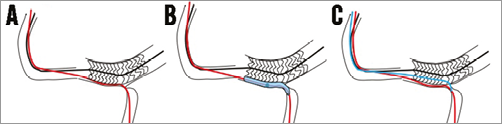
Figure 6. Use of the side branch jailed wire in case of side branch occlusion. A) Impossible side branch access secondary to carina shifting with side branch occlusion. B) Use of a small 1.2 or 1.5 mm balloon on the jailed wire to restore side branch flow. C) Use of a third wire to access the side branch through the main branch stent.
The LM is often calcified
Calcifications in the LM are frequent. In the presence of moderately calcified lesions, the use of non-compliant (NC) balloons may ensure adequate preparation of the lesion. Some operators advocate the use of cutting balloons or scoring balloons for lesion preparation. We recommend the use of NC balloons in the majority of cases in order to test the ability to expand the LM lesion correctly before stenting. When the lesion is resistant to high pressure, the Rotablator device (Boston Scientific, Marlborough, MA, USA) should be used. The Rotablator is also an excellent option in the presence of extensive calcification or when a large nodule of calcium has developed in the LM lumen. In some cases, this technical approach can be successfully implemented in the MB when access to the circumflex artery is impossible.
It is also important to underline that the ostium of the LM is part of the aorta and is significantly more resistant than other segments of the coronary tree to the radial force generated by the stent. Indeed, cases of stent recoil requiring implantation of a second stent inside the first one have been described. Now that stent struts are increasingly thinner in order to improve deliverability, the radial strength of the stent used to treat the LM should be selected carefully.
Is a T-shaped angle a marker of complexity or a marker of risk?
LM bifurcations generally have a T shape configuration. Three-dimensional (3D) measurement of the distal angle of LM stems treated with bifurcation PCI in the SYNTAX trial18 confirmed this characteristic at baseline (95° mean angle between the distal MB and the SB during diastole), and also showed that the angle was reduced by a mean value of 6° after stenting.
By analysing the changes in the angle between systole and diastole, Girasis showed that there was a systolo-diastolic variation of 11° at baseline which remained comparable after the procedure. However, a post-procedural angle variation <10° was independently associated with an increased risk of MACCE18. In a previous study17 we observed that LM bifurcations with a >70° angle were associated with an increased mortality risk (Online Figure 3). These two findings are probably complementary. Indeed, a reduction in the systolo-diastolic variation of the bifurcation is indicative of a straightening of the bifurcation, which may in turn cause stent fracture and midterm adverse clinical events29. In addition, wide bifurcation angles have been found to contain areas of high shear stress adjacent to those of low shear stress, the former possibly stimulating platelet activation and aggregation, and the latter creating a localised milieu of stasis and thrombosis30,31. Finally, stent placement in bifurcations with >70° angles induces significant rheological changes and may result in suboptimal stent apposition, especially when two stents are implanted32,33. Dzavik had previously shown in 2006 that the risk of major cardiac events was increased when the bifurcation angle was >50° and when the crush technique was used34. A similar impact of the angle was demonstrated by Adriaenssens when using the culotte technique35. Therefore, when a two-stent technique is needed in a T shape angulated LM, the use of a T-stenting or TAP technique seems preferable.
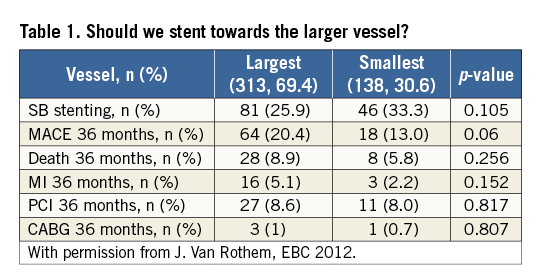
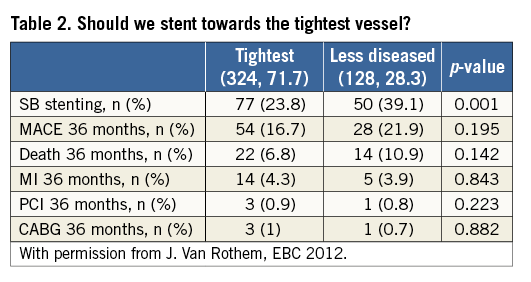
Should we stent towards the largest vessel or the tightest lesion?
This is a very important question because stent orientation towards the circumflex of the LAD may have rheological consequences as well as an impact on the number of stents implanted.
We tried to address this issue through a French multicentre study involving more than 450 patients who underwent LM stenting (oral communication by Van Rothem and Lefèvre at EBC 2012). Table 1 shows that stenting towards the largest vessel is not always the best strategy as it is associated with a higher MACCE rate at three years (p=0.06). Table 2 shows that stenting towards the tightest vessel allows a significant reduction in the number of stents used (p<0.001), with a trend towards a lower event rate at three years. These data seem to confirm that stenting in the most diseased vessel may be associated with a reduction in the number of implanted stents and a decrease in the rate of events at follow-up (Online case example 6).
What is the threshold for SB stenting?
This is a very complex issue. Given the very high inherent risk of restenosis, it is obvious that a >5 mm lesion in the circumflex coronary artery must be stented. However, a focal lesion in the ostial circumflex which is still significant after opening of the stent struts with an NC balloon of nominal size should be thoroughly analysed before being treated. Indeed, this type of lesion is generally overestimated and remains stable during follow-up. Nam et al addressed this issue in a very interesting study36. They compared QCA measurement of LCx ostial lesions after LM to LAD crossover stenting to LCx FFR measurement and showed that only 29% of lesions with >50% stenosis by QCA had an FFR <0.80 FFR (Online Figure 4). This suggests that most LCx ostial lesions should not be stented.
The specific case of trifurcation disease
LM trifurcations pose significant technical problems. However, in current practice, the basic rules of bifurcation treatment can be applied to trifurcations, and provisional SB stenting is also the recommended approach when feasible. The essential difference lies in the need for protecting two SBs instead of one. Therefore, the use of a large guide is recommended (especially when a two- or three-stent technique is anticipated) as well as the use of two protective wires. In the absence of any significant or short ostial SB lesions, the technique of “triple kissing”, also known as “trissing”36, has been shown to be associated with excellent angiographic and clinical results37.
Adjunctive imaging
This issue is still the subject of considerable debate. It is widely accepted that IVUS or OCT assessment of the final result allows verification of appropriate stent deployment and apposition, as well as identification of any anomaly likely to result in stent thrombosis or restenosis in cases where two stents are implanted38-40. These data also provide very useful and educational information on stent size, which is often underestimated, and on stent positioning at the LM ostium, which may often be too proximal or too distal. In current practice, these tools are particularly useful to operators who have limited experience in LM stenting. Intravascular imaging may also be used for evaluating lesion significance in cases where FFR is not possible or difficult to interpret due to downstream stenosis. Various cut-off values for determining physiological significance have been proposed of which the most robust is that in isolated LM disease a minimal luminal area (MLA) <4.8 mm2 is a predictor of FFR <0.80. FFR is also very useful for assessing residual LCx lesions at the end of the procedure and during follow-up in order to avoid unnecessary SB stenting.
Conclusion
In the SYNTAX trial, the treatment outcome of LM lesions significantly improved the results observed in the PCI group. The ongoing EXCEL and NOBLE trials (PCI versus CABG in LM) may further clarify this issue. The results should be available in 2016. An increasing number of patients, especially those with a low or intermediate complexity score, or those at high surgical risk, can be safely treated by PCI if the technical approach is optimal. As for all bifurcation lesions, a provisional SB stenting approach should be implemented in most cases. Specific technical problems can be solved by systematic use of two or three wires at the beginning of the procedure, proper stent selection and positioning, and liberal use of the POT technique. Because of the T-shape angulation, the T or TAP technique should be adopted in the majority of double stenting cases.
Conflict of interest statement
T. Lefèvre is on the advisory boards of Abbott Vascular, Boston Scientific and Medtronic and received minor fees from Terumo and Biosensors. J. Lassen has received scientific grants from Biosensors, St. Jude Medical, Boston Scientific, Terumo, Medtronic, Abbott Vascular and Biotronik. C. Girasis has no conflicts of interest to declare.
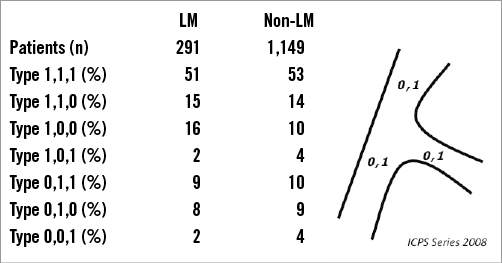
Online Figure 1. Medina classification of LM and non-LM bifurcation lesions.
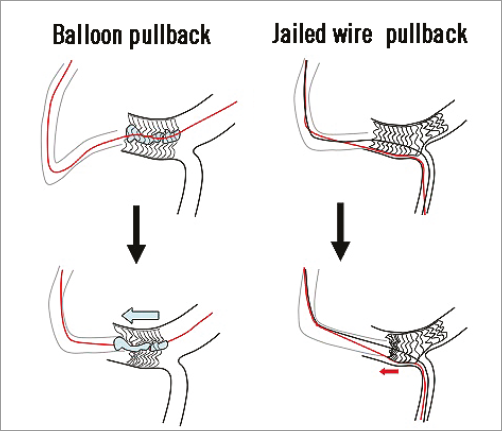
Online Figure 2. Two mechanisms of stent longitudinal distortion when stenting the left main. Left panel: the balloon delivery system or post-dilatation balloon is pulled back too early after deflation.Right panel: pullback of the jailed wire may attract the guiding catheter and damage the stent. Optimal control of the guide with the left hand is crucial.
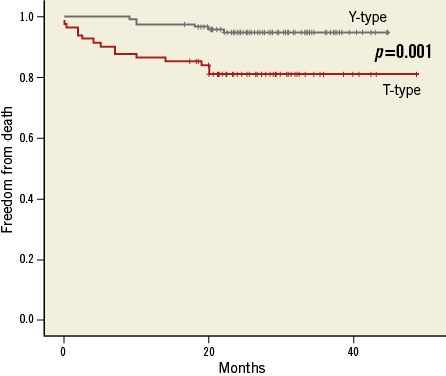
Online Figure 3. 40-month mortality in the French Left Main Taxus registry according to left main angulation (Y shape: <70°, versus T shape).
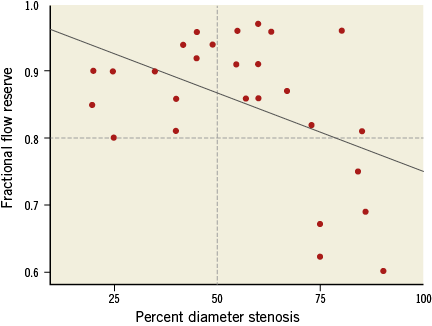
Online Figure 4. Fractional flow reserve in the LCx after LM-LAD stenting. The majority of LCx ostial lesions with a stenosis >50% by QCA are FFR negative.
Moving images
1. Case example: proximal vs. distal strut -male, 53 yrs, unstable angina (1,0,0 lesion).
01. Moving image 01. Proximal vs. distal strut.
02. Moving image 02. EBU 4 DF, 2 wires, direct stenting 3.5×18.
03. Moving image 03. POT with a 5.0 NC balloon.
04. Figure 01. SB recrossing.
05. Moving image 04. Guidewire exchange pull-back technique to enter the most distal strut.
06. Moving image 05. Kissing balloon inflation 3.5×2 NC balloons.
07. Moving image 06. Final result.
2. Case example: missed ostium - male, 62 yrs, stable angina (0,1,0 lesion).
Moving image 01. EBU 3.5, 2 wires direct stenting 3.0×18 mm.
Moving image 02. Final result after kissing balloon 3.0 and 3.5.
Moving image 03. Ostial restenosis at 10 months.
Moving image 04. LM ostium was not covered during the index procedure.
3. Case example: role of POT - male, 75 yrs, unstable angina (1,0,1 lesion).
Moving image 01. Role of POT
Moving image 02. EBU 4, 6 Fr, two wires, direct stenting, 3.5×24.
Moving image 03. No POT, (LM 4.5 mm), kissing balloon inflation after wire exchange
Moving image 04. Final result.
Moving image 05. IVUS control showing LM stent compression (LCx wire was positioned outside of the stent).
4. Case example: longitudinal compression-male, 74 yrs, unstable angina (1,1,1 lesion).
01. Figure 01. Longitudinal compression.
02. Figure 02. Longitudinal compression
03. Figure 03. Longitudinal compression.
04. Figure 04. EBU 4, 6 Fr, two wires 2.5×30 mm, SC balloon.
05. Moving image 01. Careful stent positioning Rao 10° Cr 40°.
06. Moving image 02. DES 3.5×38 at 8 atm.
07. Moving image 03. Difficult (too early) withdrawal of the balloon delivery system attracting the guiding catheter.
08. Figure 05. Stent enhancement.
09. Moving image 04. POT 4.5 mm.
10. Figure 06. Distal stenting.
11. Figure 07. Initial result before kissing balloon inflation.
12. Moving image 05. Kissing balloon inflation with 2 NC balloons 3.5 and 3.0 mm.
13. Figure 08. Ostial stent positioning (4.0×9).
14. Figure 09. Stent enhancement
15. Moving image 06. Final result.
05. Case example - risk of SB occlusion - female, 77 yrs, stable angina (1,1,1 LM lesion).
Moving image 01. Diffuse disease.
Moving image 02. Diffuse disease.
Moving image 03. EBU 3.5, 6 Fr, two wires, 2.75×28 stent, 14 atm.
Moving image 04. LCx occlusion secondary to carina shifting (stent 2.75/distal reference 2.25).
Moving image 05. POT with 3.5 NC balloon.
Moving image 06. Reparation of flow in the LCx after POT, stent crossing toward LCx with Fileder XT wire.
Moving image 07. Kissing balloon with 2.5 and 2.25 NC balloons.
Moving image 08. Careful stent positioning for T-stenting.
Moving image 09. Final kissing balloon inflation.
Moving image 10. Stent enhancement to check optimal stent deployment.
Moving image 11. Final result.
06. Case example - stent LM-LAD or LM-LCx?- male, 84 yrs, unstable angina (1,1,0 or 1,0,1 lesion according to the strategy).
Moving image 01. Baseline.
Moving image 02. EBU 4, 6 Fr, 2 wires, predilatation, LM-LCx, 2.5 NC balloon
Moving image 03. Predilation result.
Moving image 04. Ostial stent positioning, Lao 10°, Cr 38°.
Moving image 05. Stent 3.0×28 deployed at low pressure (8 atm).
Moving image 06. After POT with a 4.5 NC balloon, GW exchange, final kissing with 3.0 and 3.5 NC balloons.
Moving image 07. Final result.
07. Case example - threshold for SB stenting - male, 76 yrs, unstable angina and pulmonary oedema (1,1,1 lesion).
Moving image 01. Short LAD and severe lesion of the mid-LCx.
Moving image 02. JL 3.5 6 Fr, direct stenting toward the LCx (careful ostial positioning in Lao/cranial).
Moving image 03. After POT with a 4.5 NC balloon, wire exchange, kissing balloon 4.0 and 3.0 NC balloons.
Moving image 04. Result after kissing balloon inflation.
Moving image 05. Decision to stent the ostial LAD (lesion >5 mm) with T-stenting with a 3.0×18 DES.
Moving image 06. Final result.

