Introduction
A critical lesion in the left main coronary artery (LMCA) has been observed in 3% to 5% of all the patients undergoing coronary angiography and in 10-30% undergoing coronary artery by-pass graft (CABG). A significant LMCA disease is considered as the lesion with the highest prognostic value in the coronary system because of the extent of myocardium at risk.
In this chapter of Tools and Techniques the percutaneous treatment of LMCA disease is discussed using a step-wise approach. The following is an overview of its management with highlights on specific technical issues. The complete, unabridged e-version with images is available at www.eurointervention.org.
Background
The presence of a significant narrowing in the LMCA has remained one of the last bastions of surgical dominance.
Patient with LMCA stenosis are classified into two subgroups: protected (a previous patent CABG surgery graft to one or more major branches of the left coronary) and unprotected LMCA (ULMCA-without such bypasses).
The LMCA usually it is divided in three anatomical segments: ostium, mid-shaft and distal bifurcation. (Figure 1) Histologically, the ostium and shaft lesions have similar characteristics to the aorta being rich in elastic fibers and smooth muscle cells.
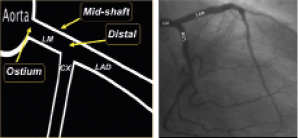
Figure 1. Schematic representation of LMCA. Ostial, shaft and distal segments are illustrated.
Conversely, the distal LMCA is more prone to develop an atherosclerotic lesion, because exposed to a greater shear stress and more frequently to turbulent blood flow. Clinical outcomes may vary according to LMCA complexity and lesion location (non-distal vs. distal and simple vs. complex distal bifurcation).
Although historical studies evaluating PCI for LMCA stenosis with bare-metal stents (BMS) have reported a favourable initial outcome, the high rate of in-stent restenosis with the subsequent need for repeated revascularisations at mid-term follow-up have limited the approach with BMS for LMCA PCI.
However the availability of drug-eluting stents (DES) that led to a significant reduction in restenosis and target lesion revascularisations (TLR) has improved immediate, mid- and long-term outcome of PCI for LMCA.
Current indications for ULMCA PCI
CABG is at the present time the gold standard therapy for patients with ULMCA disease.
However, non-randomised observational studies comparing PCI vs. CABG in ULMCA disease consistently reported, after risk adjustment, a similar composite endpoint of death, myocardial infarction (MI) or cerebrovascular accidents (CVA) at 5- (DES) and 10- (BMS) year clinical follow-up.
Moreover, data obtained from pre-specified subgroup analysis from randomised clinical trials comparing PCI vs. CABG in ULMCA disease are encouraging and in accordance with previous reports.
Emerging evidence derived from the results of the LMCA subgroup of the “Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery” (SYNTAX) Trial, suggested that PCI is non inferior as compared to CABG in the composite endpoint of death, CVA, MI, or repeat revascularisation (major adverse cardiac and cerebrovascular events [MACCE]) in patients with low (<22) and intermediate (23-32) SYNTAX score at one and three years of clinical follow-up.
These encouraging results recently advanced European guidelines recommendations for ULMCA revascularisation with PCI to class IIa B evidence in non-bifurcated lesion isolated or associated to single-vessel disease. Conversely, the indication for more complex ULMCA lesions (bifurcated lesions or ostial-shaft ULMCA lesion plus two or three vessel disease) is class IIb level of evidence B.
Methods
The following issues regarding equipment selection and techniques requiring for LMCA PCI will be discussed along with suggested tips and tricks in order to deal with potential procedural complications in the e-version of this article:
– assessment of significant LMCA stenosis (coronary angiography, intravascular ultrasound, fractional flow reserve)
– equipment for LMCA PCI (guiding catheter selection, need for haemodynamic support, stent selection)
– lesion preparation (rotational coronary atherectomy in case of diffuse and severe calcifications, when the balloon for predilatation does not cross the lesion or fully expand; difficulties in crossing the lesion with the stent)
– decision making and technical approaches depending on lesion location (non-distal vs. distal and simple vs. complex distal bifurcation) and type (LMCA restenotic lesions) (Figures 2 and 3)

Figure 2. Correct stent positioning at the ostial segment.
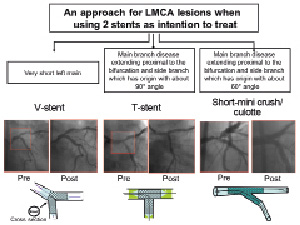
Figure 3. Our flow-chart in treating a distal lesion with 2 stent approach as intention to treat.
– assessing and optimising of LMCA PCI results (IVUS-guidance and preliminary experiences with optical coherence tomography).
– dual antiplatelet therapy management following DES implantation on LMCA
– potential complications following catheter based LMCA procedures and their management