Introduction to the session: the trial headlines
The aim of the article is to capture the session at EuroPCR 2017 covering the EXCEL and NOBLE trials, communicate the analysis of the trialists, and report the views expressed in the interactive discussion. This article does not constitute an independent review of the topic by the authors. The session was dedicated to the critical review and analysis of two recent major randomised controlled trials (RCT) comparing percutaneous coronary intervention (PCI) and coronary artery bypass graft (CABG) surgery for the treatment of left main (LM) disease, namely the Evaluation of XIENCE versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization (EXCEL)1 and the Nordic-Baltic-British Left Main Revascularisation Study (NOBLE)2 trials, and aimed to assess their potential impact on daily clinical practice.
Case presentation: how should I treat?
Michael Maeng (Denmark) presented a representative case from the NOBLE trial, of which he was one of the investigators. The patient was a 66-year-old male with stable angina in Canadian Cardiovascular Society (CCS) class III. He was a previous smoker already on medical treatment for hypertension and hypercholesterolaemia, with normal renal function and unremarkable echocardiographic findings. Coronary angiogram showed distal LM disease with a tight stenosis at the bifurcation involving the ostia of both the left anterior descending (LAD) and the left circumflex (LCx) arteries.
“What is common practice?” discussion
The audience was polled on the therapeutic approach they would choose for this patient. Nobody was in favour of ad hoc PCI, whereas nearly all participants would have discussed the case with the surgeons. When polled on how they discuss cases with surgeons in their routine practice, what emerged is that slightly more than half of the audience have formal Heart Team meetings, whereas the remainder discuss cases on an individual basis. However, for the majority of the audience, CABG was the treatment of choice for LM disease in their routine practice. The majority of the audience reported that they do not routinely use the Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) score in the decision process, mainly because it is not deemed to carry sufficient prognostic information in the setting of LM disease. EuroSCORE II and Society of Thoracic Surgeons (STS) score were preferred by the majority of participants.
Background: what was known before the trials
Guillaume Cayla (France) provided an overview of the literature. Prior to EXCEL and NOBLE, four randomised studies had compared PCI and CABG for the treatment of LM disease3-7. All these early studies evaluated first-generation drug-eluting stents (DES), included a relatively small number of patients, and were designed for non-inferiority compared to CABG (except for the LE MANS registry). In a meta-analysis of the four randomised studies by Capodanno et al8, stroke at one-year follow-up was significantly more frequent in patients treated with CABG, whereas target vessel revascularisation (TVR) was significantly more frequent with PCI, but importantly there were no significant differences in the incidence of death, myocardial infarction (MI) and MACCE. Moreover, in a pooled analysis of patient-level data from the Premier of Randomized Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease (PRECOMBAT) and Synergy between PCI with TAXUS drug-eluting stent and Cardiac Surgery (SYNTAX) Left Main trials9, MACCE rates at five years were similar between PCI and CABG groups among patients with a SYNTAX score <33 (23.9% vs. 21.1%, p=0.47), but significantly higher after PCI among patients with SYNTAX score ≥33 (38.5% vs. 26.4%, p=0.007).
Based on this evidence, the 2014 ESC/EACTS guidelines on LM revascularisation10 recommend a class IB for both PCI and CABG for patients with a SYNTAX score ≤22, a class IB for CABG and class IIa B for PCI for those with a SYNTAX score between 23 and 32, and class IB for CABG and class IIIB for PCI for those with a SYNTAX score ≥33.
Trial analysis: summary of the trialists’ critical review
Alexandra Lansky (USA) provided an in-depth analysis of the EXCEL and NOBLE trials. The EXCEL trial1 recruited 1,905 patients with left main coronary artery disease and SYNTAX score ≤32 at 126 sites in 17 countries (both American and European) from 2010 to 2014. Mean age was 66 years, with 30% of those in the PCI cohort having diabetes mellitus, and 24% presenting with acute coronary syndrome (ACS). Mean SYNTAX score, based on core lab assessment, was 27 in patients treated with PCI. The primary endpoint of the trial was the composite of death, stroke and MI (including periprocedural events) at three-year follow-up, which was not significantly different between patients randomised to receive PCI or CABG (15.4% versus 14.7%; hazard ratio [HR] 1.00, 95% confidence interval [CI]: 0.79-1.26; p=0.98). The trial was powered for non-inferiority testing (with a margin of 4.2%) of the primary endpoint, which was met. Non-inferiority was also met for the secondary pre-specified composite endpoint of death, stroke, MI or ischaemia-driven revascularisation at three years (23.1% vs. 19.1%). A landmark analysis showed that, within the first 30 days, PCI performed better than CABG in terms of the primary composite endpoint (4.9% vs. 7.9%, p=0.008) and in terms of MI, which was defined as >10 times elevation of myonecrosis markers (3.9% vs. 6.2%, p=0.02), whereas there was no significant difference in the death and stroke rates. From 30 days to three years, there was a reversal of these results, with CABG performing better with respect to death, stroke or MI (11.5% vs. 7.9%, p=0.02) and MI (4.2% vs. 2.5%, p=0.05).
The NOBLE trial2 included 1,201 patients at 36 sites in nine European countries between 2008 and 2015. In the PCI cohort, the mean age was 66 years, 15% were diabetics and 18% presented with acute coronary syndromes. The mean SYNTAX score was 23 in patients treated with PCI. The primary endpoint was a composite of death, non-periprocedural MI, any repeat coronary revascularisation, and stroke. Non-inferiority of PCI to CABG required the lower end of the 95% CI not to exceed an HR of 1.35 after up to five years of follow-up. In the NOBLE trial, PCI was associated with significantly higher rates of MACCE (29% vs. 19%; HR 1.48, 95% CI: 1.11-1.96; p=0.007), non-periprocedural MI (7% vs. 2%; HR 2.88, 95% CI: 1.40-5.90; p=0.004), and repeat revascularisation (16% vs. 10%; HR 1.50, 95% CI: 1.04-2.17; p=0.032), whereas there was no significant difference in mortality and stroke rates, although there was a strong trend towards higher stroke rates in the PCI group (5% vs. 2%; HR 2.25, 95% CI: 0.93-5.48; p=0.07).
Analysing these results (Figure 1), Alexandra Lansky pointed out that, taking into account the differences between the two trials, which include a higher risk population in EXCEL, different endpoint definitions between trials and the use of different stents (in all cases everolimus-eluting stents in EXCEL; first-generation DES at the beginning of the trial and biolimus A9-eluting stents afterwards in NOBLE), the results are more similar than one might think. In fact, there were no major differences between the two studies with respect to the relative outcomes of all-cause death, cardiovascular death, periprocedural and non-periprocedural MI, and revascularisation. Comparing the absolute incidence of each endpoint stratified by randomisation group in the two studies, the results at three years were very similar, except for a slightly higher mortality in EXCEL, which might be partly explained by the overall higher risk of the patients enrolled in EXCEL compared to NOBLE. The real differences pertain to stroke and stent thrombosis or symptomatic graft occlusion. Of note, in NOBLE there were more strokes in the PCI group, which was not observed in any other study, and there were more stent thromboses associated with the first-generation DES/biolimus A9-eluting stent compared with the everolimus-eluting stent.
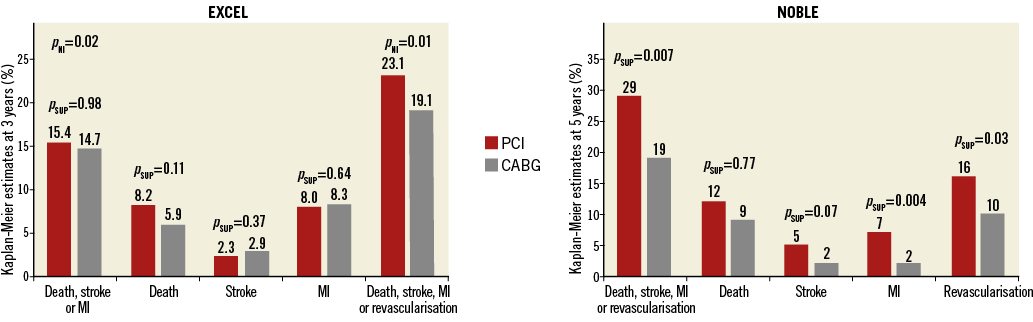
Figure 1. Main results of the EXCEL and NOBLE trials. MI: myocardial infarction; PNI: p-value for non-inferiority; PSUP: p-value for superiority.
In subgroup analyses of the EXCEL trial, there were no differences in the rates of the primary endpoint when patients were stratified according to the number of diseased vessels or to SYNTAX score. However, among patients with low SYNTAX score (i.e., ≤22), there was a trend towards better outcomes with PCI compared with CABG (10.3% vs. 13.3%; HR 0.71, 95% CI: 0.45-1.14, p=0.16).
The gender analysis of EXCEL deserves attention. Of all subgroup analyses in EXCEL, gender was the only one demonstrating a borderline interaction with treatment strategy. In fact, women, who accounted for less than a quarter of the overall population, benefited more from CABG than PCI. A similar observation was previously shown in the SYNTAX trial, where in the PCI group female gender was an independent predictor of death at five years; this was not the case in the CABG group where there was no difference in mortality between men and women11.
Overall, the take-home messages proposed by Alexandra Lansky were that: 1) the SYNTAX score-based approach for LM disease recommendations seems outdated and at least the low and intermediate categories should be condensed, and appears irrelevant and contradictory in women; 2) guideline recommendations should be upgraded to class I for PCI (with everolimus-eluting stents) as an “acceptable alternative” to CABG in low- and intermediate-risk patients; 3) women were underrepresented and had worse outcomes with PCI compared with CABG, and therefore the overall results of EXCEL should not be generalised to female gender until this population can be further studied; and 4) in general, LM recommendations have to be patient-centred considering the early and long-term trade-offs of each procedure.
“Will these trials change my practice?” discussion
The following discussion focused on the key differences between the two trials. According to Michael Maeng, the difference between the results of the two studies should be mainly attributed to the different length of the follow-up. In fact, after an initial advantage of PCI over CABG in EXCEL, the Kaplan-Meier curves converge by the end of the three-year follow-up and might continue to diverge so that very similar results to NOBLE could be observed at five years. In this respect, Alexandra Lansky pointed out that in NOBLE five-year Kaplan-Meier estimates were reported, whereas the median follow-up was three years. As a consequence of the high dropout rates (more often involving asymptomatic patients), the difference between the two study arms might be overestimated. All discussants agreed on the importance of obtaining very long-term follow-up in both studies. Another point raised by the audience was the small rate of arterial-only revascularisation in CABG-treated patients in both studies (25% in EXCEL, 14% in NOBLE). Philippe Kolh stated that, although challenging, this revascularisation modality should be the first choice, at least in patients below the age of 70, and that, if the rates of arterial-only revascularisation were higher in the two studies, the results would probably have been better in the CABG groups, at least in the long run. The difference in the stent type used in the two trials was then discussed. The use of first-generation DES in the first part of enrolment was also proposed as a possible explanation for the worse outcomes of PCI in NOBLE, and Michael Maeng reminded the audience that, out of the seven definite stent thromboses recorded in the study, three occurred in patients treated with first-generation DES, which were only a minority (~10%) of the overall PCI population12. There was general consensus that stent choice is a key element to the success of PCI, especially in a complex setting such as LM disease, which most often involves bifurcations.
Michael Maeng followed up with the case presentation. Interventional cardiologists and surgeons in charge of the patients agreed that PCI and CABG appeared equally safe based on the available evidence. Therefore, the patient was asked to participate in the NOBLE trial and informed consent was obtained. The patient was randomised to receive PCI. He underwent successful IVUS-guided PCI of the left main with the culotte technique using two DES, with a good final angiographic result. The patient has recently been examined, six years after LM stenting; he reported no major events during this period and was still angina-free.
The Chairperson’s conclusion: where do we stand now?
Pascal Meier polled the audience on the treatment strategy they would choose for the patient presented in the session. The majority of participants were now in favour of PCI in this particular case. However, the same would not apply in more complex cases. Everyone agreed that the treatment choice should be individualised, based on the clinical and angiographic characteristics of each patient. Again, there was general consensus that patients should be involved in the decision process and should be offered a clear view of both treatment options, being aware that PCI might be more favourable in the short term/midterm and CABG might have better results in the long run.
| Summary MAJOR ARGUMENTS FOR A CHANGE IN PRACTICE Left main PCI with new-generation DES is associated with improved outcomes compared with first-generation DES. PCI with new-generation DES is an “acceptable alternative” to CABG in low- and intermediate-risk patients, as the two strategies are associated with similar outcomes in the short term/midterm. The SYNTAX score-based approach for left main disease recommendations seems outdated and at least the low and intermediate categories should be condensed. MAJOR ARGUMENTS AGAINST A CHANGE IN PRACTICE Compared with PCI, CABG seems to be associated with improved outcomes in the long run. CABG remains a more favourable option in women, in whom PCI is associated with increased risk of adverse events. Left main recommendations should be patient-centred considering the early and long-term trade-offs of each procedure. |
Conflict of interest statement
M. Maeng reports unrestricted research grants to his institution from Boston Scientific, Biosensors, and Volcano, and consulting/lecture fees from AstraZeneca and Bayer. G. Cayla reports research grants to the institution or consulting/lecture fees from Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Boston Scientific, Biotronik, Bristol-Myers Squibb, Daiichi-Sankyo, Eli Lilly, Europa, Fédération Française de Cardiologie, Fondation cœur et recherche, Medtronic, MSD, Pfizer, Sanofi-Aventis, and The Medicines Company. The other authors report no conflicts of interest in relation to this article.