Although coronary artery bypass grafting (CABG) is still a major cornerstone of the revascularisation strategy in patients with significant left main coronary artery (LMCA) disease, percutaneous coronary intervention (PCI) has been a good alternative choice for revascularisation on the basis of key randomised clinical trials (RCTs) and several observational studies12. Current practice guidelines recommend either CABG or PCI with a drug-eluting stent (DES) for the treatment of significant LMCA disease with low-to-intermediate anatomical complexity34.
However, there has been no one-size-fits-all approach for LMCA revascularisation in real-world clinical practice, and the choice of the best revascularisation strategy is a complex undertaking. A multidisciplinary decision-making (Heart Team) approach can play an important role in tailored decision making for patients with LMCA disease, incorporating key clinical factors, anatomic factors, and physician/patient preferences, which are likely to influence the selection of the best procedure for individual patients. In addition, it should be recognised that the particularities of clinical practice in each institution, as well as the specific expertise of the interventional cardiologists and cardiac surgeons who perform the procedures, might differ substantially for each institution and practitioner among different geographic regions. This might potentially limit the reproducibility of specific experiences from dedicated practising centres and observed findings from specific trials in other unrestricted clinical settings. Furthermore, there was a substantial regional difference in the interaction between important risk factors and the outcome risk of PCI relative to CABG in patients with complex multivessel and LMCA disease5. However, little is known about the potential variations in practice patterns and whether comparative short- and long-term outcomes after PCI or CABG for LMCA disease are consistent without substantial regional differences.
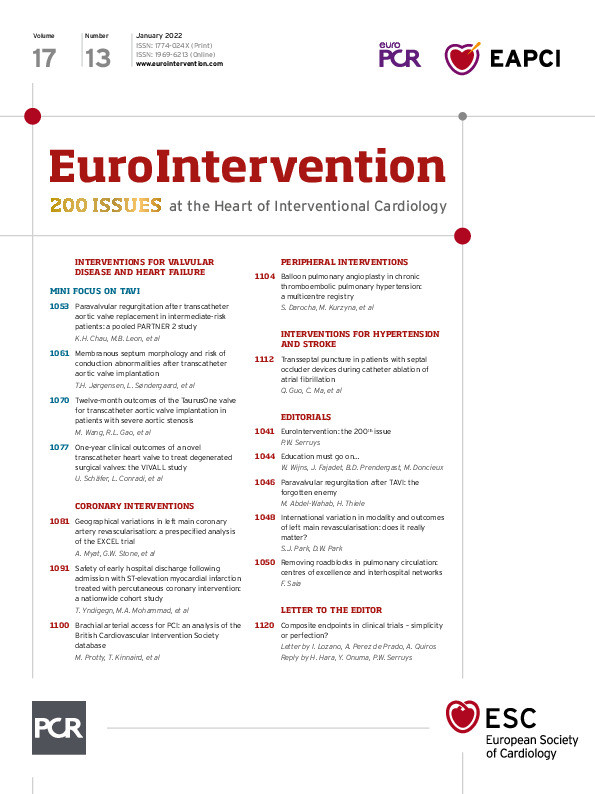
This issue has been addressed by Myat et al in this issue of EuroIntervention6. They performed a pre-specified analysis of the EXCEL trial. In this large, international trial, study patients were enrolled from 126 centres from 17 countries including the European Union (EU), the USA, Canada, South America, Asia, and Australia.
The investigators sought to determine whether relative outcomes after PCI and CABG remained consistent, regardless of known geographic variations, in patient characteristics and clinical practice. Among 1,905 randomised patients, 1,075 (56.4%) were recruited at 52 EU centres, and 752 (39.5%) were recruited at 67 North American (NA) centres. There were substantial regional variations in numerous baseline demographics (e.g., gender, body mass index, and concomitant cardiovascular risk factors), complexity of coronary anatomy, pharmacotherapy and procedural or operative characteristics. Nevertheless, there were no significant differences in the relative 30-day, three-year, and five-year primary composite endpoint of death, myocardial infarction (MI), or stroke after PCI versus CABG across the different regions. However, patients enrolled in NA had substantially higher late rates of ischaemia-driven revascularisation after PCI, for which the plausible explanations might be multifactorial (e.g., a different proportion of diabetes, prior PCI or MI, different site and operator procedural experiences, variations of cardioactive medications and duration of dual antiplatelet therapy). In addition, a different threshold for reintervention after PCI could be a possible cause because of different rates of follow-up stress testing or reimbursement policy. These findings reinforce once again that the principal findings from the EXCEL trial of comparable five-year rates of primary outcome after PCI and CABG for left main disease could be equally applicable to patients enrolled in EU and NA centres.
Medical infrastructure, racial distribution, procedural strategy and experience, and the corresponding outcomes of each revascularisation strategy may vary in Europe, the USA, Asia, and other continents7. Furthermore, there could be several known or unknown confounders influencing the practice pattern and outcomes beyond geographical difference. Current practical guidelines strongly recommend a “Heart Team” approach in patients with complex coronary artery disease (CAD), including significant LMCA disease34. Despite this, as supporting evidence for PCI as a less invasive and reasonable approach in selected LMCA disease has accumulated, the physicians’ threshold for performing complex PCI for LMCA disease has become less restrictive. As a result, a rapid rise in the volume of left main PCI and a relative decrease in CABG have been observed in a real-world multinational registry1. Although the rise in PCI utilisation is a widespread phenomenon, there is marked variability in PCI-to-CABG ratios observed between countries or across regions under different healthcare systems8, which could raise concern on the overuse or the inappropriate use of PCI for LMCA disease. Furthermore, the available treatment options for patients in developing countries differ from those in Western countries due to the less well-developed healthcare infrastructure (i.e., experienced physicians, medical services, and devices). In this regard, the consistency and generality of recommendations could be addressed by the Heart Team approach, which has been a common practice worldwide to encourage appropriate treatment. This fact is important in our daily clinical practice when deciding a treatment strategy and could have a significant impact in the cardiology community, taking into account the ongoing globalisation of our medical practice. Finally, considering this ongoing globalisation, the regional heterogeneity for LMCA revascularisation needs to be well recognised and taken into account during the decision-making process.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.