Abstract
Aims: Trifurcation lesions, which are mostly observed in distal left main (LM), represent a technical challenge for interventional cardiologists. We sought to determine the feasibility and long-term clinical outcome of drug eluting stent (DES) implantation in patients with LM coronary trifurcation lesions.
Methods and results: All patients with clinically significant de novo LM trifurcation lesions, who refused coronary artery bypass surgery and were considered eligible for percutaneous coronary intervention (PCI), were consecutively enrolled in this study from November 2005 to February 2007. Eleven patients (65±9 years, 91% men) met all the inclusion criteria and underwent LM trifurcation stenting with DES. Angiographic success was 100%. Clinical follow-up in all patients and angiographic follow-up in 91% of patients was available at 32±7 and 8±2 months, respectively. The primary endpoint, defined as the composite of cardiac death or acute myocardial infarction, occurred in one patient (9%). No cases of stent thrombosis were recorded. Three patients (27%), experienced a clinically-driven target lesion revascularisation (TLR).
Conclusions: PCI with DES implantation in patients with LM trifurcation seems feasible and safe, with acceptable TLR rates. Large scale multicentre registries are warranted to reliably address clinical outcome of this subset of patients.
Introduction
The treatment of bifurcation lesions, especially those involving left main (LM), remains a technical challenge for the interventional cardiologists as it is hampered by a worse clinical and angiographic outcome when compared to non-bifurcation lesions.1-4 Trifurcation lesions, which are mostly observed in the distal LM, are technically even more challenging, with the potential for both early procedural complications (stent distortion, plaque shift, dissection, side branch trapping) and late in-stent restenosis5. Part of the complexity of treating these subset of lesions relates to the different anatomic patterns of the stenosis, given the possible involvement of the proximal as well as the distal part of the main branch and/or the side branches, the close proximity of the side branches origin6, the angle of side branches take-off and the size of both main and side branches.
The use of drug eluting stents (DES), either sirolimus-eluting stent (Cypher®, Cordis/Johnson & Johnson, Warren, NJ, USA), paclitaxel-eluting stent (Taxus®, Boston Scientific, Natick, MA, USA) or zotarolimus-eluting stent (Endeavor® Medtronic, Minneapolis, MN, USA) has been shown to be associated with a low event rate, driven by a reduction in restenosis compared with historical controls in complex subsets of lesions, including coronary bifurcations7-10.
Some anecdotal cases of trifurcation lesions have been reported highlighting the importance of triple kissing balloon inflation at the completion of the procedure and the need for DES implantation in order to achieve an optimal angiographic and clinical outcome11-13. However, no reports specifically addressed the impact of DES implantation in this subset of lesions. Thus, we sought to evaluate feasibility and long-term clinical and angiographic outcome following DES implantation in a series of consecutive patients with LM coronary trifurcation lesions.
Materials and methods
Study population
We report data on all consecutive patients eligible for percutaneous coronary intervention (PCI) with DES and presenting with clinically significant de novo LM trifurcation lesions who refused coronary artery bypass surgery and gave informed written consent for PCI from November 2005 to February 2007. Anatomically, a trifurcation was defined as the close origin of two side branches (SB) from the main branch (MB), identified as the distance of both SBs’ take-off <3 mm, with branch size ≥2.25 mm at baseline angiography or after pre-dilatation. Trifurcation lesions were defined as the presence of a diameter stenosis >50% within 5 mm from the carina involving the MB, associated or not with significant disease in either one or both SBs. The MB was defined as the bigger branch with the largest perfusion territory. Between the SBs, the one with the narrowest angle from the distal main branch was defined as SB1, while the other one was identified as SB2 . Trifurcation lesions were classified by visual assessment according to the Medina classification described for bifurcation lesion14 and adapted for trifurcation lesions (Figure 1).
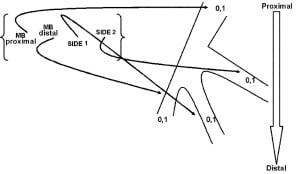
Figure 1. Medina classification adapted for trifurcation lesion.
Angioplasty procedure
All patients were pretreated with aspirin 100 mg and clopidogrel 75 mg. A clopidogrel 300 mg loading dose before the procedure was given if patients were not pretreated. During the procedure, patients received intravenous unfractioned heparin (80 IU/Kg) to maintain activated clotting time between 250 and 300 sec. Administration of glycoprotein IIb/IIIa inhibitors was left to the operator’s discretion, and was employed in 27.3% of cases. After procedure, all patients were prescribed lifelong aspirin (100 mg daily) and clopidogrel (75 mg daily) for 12 months.
The strategy of trifurcation stenting was chosen by the operator, who decided to implant 3, 2 or 1 stent(s) according to vessel anatomy, lesion distribution (e.g., SBs significantly narrowed at the ostium or within a few millimeters) and/or when a significant plaque shift was expected. The common techniques for treating bifurcation lesions (Provisional T stenting, Crush, Minicrush, T-modified, V-stenting) were performed as previously described15-19. When the operator decided to stent all branches, the «double Crush», the «double Minicrush», the «double T-Modified» or the «double Modified V-stenting» techniques were used. Final kissing balloon was strongly recommended as a laboratory standard, while final triple kissing inflation was performed based on operator’s judgement.
All patients were monitored for any post-procedure event, including chest pain, heart failure, bleeding, or recurrent ischaemia. CK-MB and troponin I were measured at 6-8 and 12-24 hours post-procedure.
Follow-up and clinical definitions
Clinical follow-up was performed by office visit. All patients underwent stress test at one and six months. Angiographic follow-up was scheduled between six and eight months after the procedure, or earlier if clinically indicated, as a standard of care.
The primary endpoint was defined as the composite of cardiac death and acute myocardial infarction (AMI), whereas secondary endpoints were stent thrombosis, target lesion revascularisation (TLR) and target trifurcation revascularisation (TTR), either percutaneous or surgical. All deaths were considered cardiac unless otherwise documented. A non-Q-wave AMI was defined as creatine kinase-MB enzyme elevation ≥3 times the upper limit of the normal value; the event was defined as a Q-wave AMI when, in addition to enzyme elevation, there were new pathological Q waves in the electrocardiogram. TLR was defined as a repeat revascularisation with a stenosis ≥50% within the stent or in the 5 mm distal or proximal segments adjacent to the stent; TTR was defined as a repeat revascularisation with a stenosis ≥50% within 5 mm proximal or distal to the carina of trifurcation, either into the MB and/or the SBs (Figure 2).
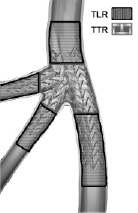
Figure 2. A schematic diagram of a typical left main trifurcation with definition of target lesion revascularisation (TLR) and target trifurcation revascularisation (TTR).
According to the Academic Research Consortium definition20, stent thromboses were defined as follows: 1) definite/confirmed, when patient presented in the context of an acute coronary syndrome with angiographic documentation of either vessel occlusion or thrombus within or adjacent to a previously successfully stented vessel or, in the absence of angiographic confirmation, either AMI in the distribution of the treated vessel or death not clearly attributable to other causes; 2) probable, in case of unexplained death within 30 days or target vessel AMI without angiographic confirmation of acute stent thrombosis or another identified culprit lesion; 3) possible, in case of unexplained death after 30 days. Stent thrombosis was further categorised according to the timing of the event into intraprocedural, subacute (from the end of the procedure to 30 days), late (>30 days up to one year) and very late (>1 year) stent thrombosis.
Angiographic success was defined as a final residual stenosis <30% with TIMI flow grade 3 in either the MB or the SBs.
Quantitative coronary angiographic analysis (QCA)
Coronary angiograms obtained at baseline, at completion of the stenting procedure and at angiographic follow-up, were analysed using a computer-based algorithm developed by CardiOp-B system (Paeion Inc, New York, NY, USA) (Figure 3).
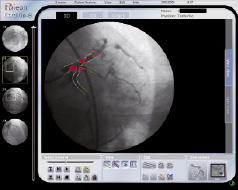
Figure 3. An example of the CardiOp-B 3D angiogram reconstruction process.
The projection that best showed the stenosis in both the MB and the SBs in its tightest view was used for all angiograms. In none of the patients the angiogram was unreadable or technically deficient for the analysis. One experienced technician who was blinded to the patients’ identities and outcomes performed quantitative analyses of all angiographic data. Minimal lumen diameter and the nearest normal reference diameter were measured in millimetres using the catheter as scaling factor. Percent stenosis was calculated as 100x(1- minimal lumen diameter/normal reference diameter). Binary angiographic restenosis was defined as >50% diameter stenosis of the target lesion. Late lumen loss was defined as the difference in minimal luminal diameter at completion of the stent procedure and at follow-up. The pattern of restenosis was evaluated according to the classification of Mehran et al21.
Results
Procedural characteristics
A total of 11 patients with LM trifurcation lesions submitted to PCI was analysed. Baseline and clinical characteristics of these patients are outlined in Table 1.
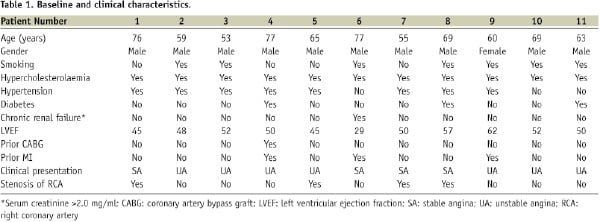
Men accounted for 91% of patients. Mean age and left ventricular ejection fraction were 65±9 years and 50±9%, respectively.
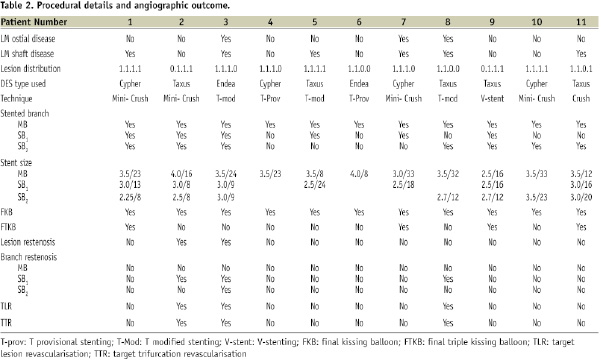
Procedural details and angiographic outcomes are listed in Table 2.
Haemodynamic support devices, such as intra-aortic balloon pumping, were not used during the procedure. In five (45%) patients only the LM trifurcation was involved whereas in three (27%) cases a significant ostial and shaft stenosis was present as well.
Successful delivery of stent to MB and SBs was adequately accomplished in all cases. During and after the procedure, occlusion of SBs and significant residual stenosis did not occur in any case (angiographic success=100%). No additional stent was required to seal significant dissections at edges, but in patients No 3, 6 and 11 an additional stent was implanted to cover the full lesion length in the distal MB. The stenting techniques used were the Mini-crush or double Mini-crush in four patients (36%), T-provisional stenting in two patients (18%), T-modified in three patients (27%), double modified V stenting in one patient (9%) and double crush in one patient (9%). Five patients (45%) received a DES in all the trifurcation branches. Final kissing balloon was employed in all patients and in four of them (36%), final triple kissing balloon was also performed. Five patients received additional balloon angioplasty and/or stenting for non-trifurcation lesions during the index procedure, with a total stent length per lesion of 17±8 mm. Angiographic QCA results are summarised in Table 3.

In-hospital and long-term clinical outcome
Clinical follow-up was available for all patients at a mean of 32±7 months. Angiographic follow-up was performed in 10 patients (91%) at 8±2 months (Figure 4).
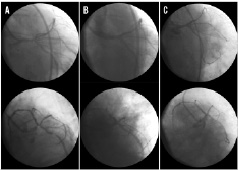
Figure 4. A case example of percutaneous coronary intervention for left main trifurcation (patient No. 1): Antero-posterior caudal view and left anterior oblique caudal view showing severe narrowing stenosis of left main (A), the same projections after double mini-crush technique (B), the same projections at 8-months angiographic follow-up (C).
The primary endpoint occurred in one patient (No 8) who experienced an in-hospital non-Q-wave AMI for intraprocedural occlusion of a small diagonal branch. At 30 days follow-up, no other events occurred in this patient. Three patients had a TLR within the follow-up period (27%); of these, two underwent repeat PCI with balloon dilatation (patients No 2 and No 8) due to a significant focal restenosis of the first SB close to the trifurcation carina, and one underwent CABG (patient No 3) due to a significant restenosis with a diffuse pattern affecting all branches of LM trifurcation (Table 3). Patients No 2 and No 8 were symptomatic for angina at medium work load, while patient No 3 was re-admitted to our hospital for pulmonary oedema. Therefore, all TLR were driven by symptoms and/or signs of ischaemia resulting from restenosis in LM trifurcation. No episode of death or stent thrombosis was recorded.
Discussion
Coronary trifurcation lesions are mainly found in the distal LM coronary artery. The evolution of stenting techniques and the use of DES have made the treatment of this subset of lesions more attractive for the interventional cardiologist.
The present study collects the longest clinical follow-up following PCI in trifurcation lesions and suggests that the percutaneous approach is safe despite a high procedural complexity. Importantly, no cardiac deaths were observed and no stent thrombosis occurred, despite an average of 2.3±0.8 DES for trifurcation. The rate of TLR was 27%, which is higher than that reported in bifurcation lesions treated with DES5-8, but consistent with that of other studies on unprotected distal LM treated with DES4,22. Also, these results are consistent with those previously reported at shorter follow-up in patients with trifurcation lesions23-25.
The decision to implant three stents from the beginning of the procedure was mainly based on the anatomical patterns of the trifurcation lesion, the size of SBs and the length of SBs’ disease. Conversely, in cases of very tortuous, angled and calcified lesions, it was considered reasonable to accept a residual stenosis, which is a price frequently paid in cases of provisional stenting, rather than performing a dangerous procedure to achieve the goal of an optimal angiographic result at the level of the SBs26-27. Given that the complexity of a trifurcation lesion suggests the need for multiple stents, the suggestion of a simple strategy may be difficult to accept. However, our results demonstrate that even in the case of a simple approach, the patency of the MB, which is the most pressing goal, is maintained at long-term follow-up. It is of note that the technical challenges increase further when the two SBs have their origin in close proximity to each other. In this situation, triple kissing balloon inflation seems to be mandatory to achieve an optimal angiographic and clinical outcome11.
When a three DES approach in a LM trifurcation lesion is deemed necessary, the classical techniques applicable to treat bifurcation lesions can be safely performed with a high early angiographic success rate, despite a rather high rate of restenosis at angiographic follow-up. In our study, five patients received three DES implantations. Of them, two were treated with a double mini-crush (patients No 1 and No 2), one with double crush (patient No 11), one with a double T-modified (patient No 3) and one with a double modified V-stenting technique (patient No 8). In these patients, angiographic success was 100% and restenosis at follow-up was 40%.
Finally, it is important to remark that final triple kissing balloon was not performed in all patients who experienced restenosis, most likely resulting in incomplete dilatation and stent expansion at the level of SBs ostium, as demonstrated by the focal restenosis observed in patients No 2 and No 8.
Study limitation
This study has some limitations. First, it is a retrospective evaluation of a small cohort of patients and it reflects only the experience of a single institution. Large scale multicentre registries are necessary to reliably address the issue of clinical outcome in LM trifurcation PCI with multiple DES, assessing the actual risk of stent thrombosis and death or myocardial infarction. Another caveat of the study is the complex mix of lesion type and stenting strategies. In addition, intravascular ultrasound was not used, both at baseline (to better understand the plaque distribution among the branches of trifurcation) and at angiographic follow-up (to provide insights into stent under-expansion).
Conclusions
Our data suggest that PCI of LM coronary artery trifurcation is feasible and safe at long-term, with acceptable TLR rates, if performed by experienced operators by selecting a specific approach for each type of lesion and patient.

