Abstract
Aims: The study aimed to examine five-year clinical outcomes of complete (CR), partially complete (PCR), and incomplete revascularisation (ICR) in patients with unprotected left main coronary artery (ULMCA) disease treated with drug-eluting stents (DES). Completeness of revascularisation, defined as revascularisation of all vessels ≥1.5 or 2.5 mm in diameter, has been shown to correlate with outcomes after percutaneous coronary intervention (PCI). There are no data to compare revascularisation strategies on long-term clinical outcomes in patients undergoing PCI of ULMCA disease.
Methods and results: This prospective registry enrolled 910 consecutive patients with ULMCA disease undergoing PCI with DES implantation. CR included patients who had a successful revascularisation of all diseased segments with diameter ≥1.5 mm. PCR included patients who had successful revascularisation of all diseased segments with diameter ≥2.5 mm. ICR included patients who did not achieve revascularisation for all diseased segments of diameter ≥2.5 mm. The primary endpoint was the incidence of major adverse cardiac events (MACE: a composite of cardiac death, myocardial infarction and repeat revascularisation) at five-year follow-up. CR was achieved in 386 (42.4%), PCR in 227 (25.0%), and ICR in 297 (32.6%) patients. Patients with ICR had a significantly higher rate of MACE (29.6% vs. 22.5% and 15.5%, p<0.001) and all-cause mortality (12.5% vs. 7.0% and 6.2%; p=0.006) than those with CR and PCR at five-year follow-up. After propensity score matching, patients with CR vs. PCR had similar incidences of MACE (hazard ratio [HR]: 1.16, 95% confidence interval [CI]: 0.78-1.74, p=0.46), mortality (HR: 1.27, 95% CI: 0.61-2.63, p=0.53), and cardiac death (1.8% vs. 4.5%; HR: 2.56, 95% CI: 0.80-8.17, p=0.11). On multivariable logistic regression analysis, ICR appears to be an outcome of poor clinical characteristics, comorbidities and complex coronary anatomy.
Conclusions: In the treatment of patients with ULMCA disease, ICR was associated with worse long-term clinical outcomes than CR and PCR. PCR has clinical outcomes similar to CR in patients with ULMCA disease treated with DES.
Abbreviations
CABG: coronary artery bypass grafting
CR: complete revascularisation
CTO: chronic total occlusion
DES: drug-eluting stent
ICR: incomplete revascularisation
MI: myocardial infarction
MACE: major adverse cardiac events
PCI: percutaneous coronary intervention
ULMCA: unprotected left main coronary artery
Introduction
Unprotected left main coronary artery (ULMCA) disease has traditionally been treated exclusively with coronary artery bypass grafting (CABG), based on historical data comparing CABG with plain old balloon angioplasty or percutaneous coronary intervention (PCI) with bare metal stents1. However, several contemporary studies have shown that PCI with drug-eluting stents (DES) may yield outcomes similar to CABG2-4. PCI for ULMCA disease has, therefore, been upgraded to a Class IIb indication, and it may be considered for patients with coronary anatomy that is associated with a low risk of procedural complications if treated by PCI and/or clinical conditions that predict an increased risk of adverse surgical outcomes1,5.
Complete revascularisation, defined as revascularisation in all diseased segments ≥1.5 up to 2.5 mm (Asan Medical Center Multivessel Registry), ≥1.5 mm (SYNTAX trial), and ≥2.0 mm (ACUITY trial), of complex coronary artery disease with percutaneous deployment of DES has been shown to improve clinical outcomes in patients with multivessel disease, acute coronary syndrome, or diabetes mellitus6-8. However, whether patients who did not receive revascularisation for the diseased segments with diameters between 1.5 mm and 2.5 mm was related to detrimental clinical outcomes remains unknown. Furthermore, there are no data on the impact of complete revascularisation in patients with ULMCA disease treated with DES.
We hypothesised that a “partially complete” revascularisation, defined as revascularisation of all diseased segments ≥2.5 mm diameter, does not lead to an adverse prognosis compared with complete revascularisation. The purpose of this study was to assess the impact of our proposed revascularisation classification (complete [CR], partially complete [PCR], and incomplete revascularisation [ICR]) on long-term clinical outcomes in patients with ULMCA disease after PCI with DES implantation.
Methods
STUDY POPULATION
Data were collected prospectively for patients with ULMCA disease undergoing PCI with DES implantation in eight high-volume cardiac centres in China between March 2004 and April 20079. The left main coronary artery was considered unprotected if there were no patent grafts to the left anterior descending artery (LAD) or circumflex artery (LCX). Patients who were treated with bare metal stents, had previous CABG, or were in cardiogenic shock at the time of the index procedure were excluded. Patients undergoing PCI for acute myocardial infarction were also excluded from the present study, following the inclusion criteria of the SYNTAX trial10. Ethical approval was obtained from relevant committees in all the institutions participating in this study. All patients provided written, informed consent for participation in the study.
INTERVENTIONAL PROCEDURE AND MEDICATIONS
All patients, or their legally authorised representatives, were invited to participate in the discussion with the clinical Heart Team. DES selection, procedural technique, use of IVUS and glycoprotein IIb/IIIa inhibitors were at the discretion of the operators. In this study, sirolimus-eluting stents (Firebird™; MicroPort Co., Shanghai11, China; EXCEL; Jiwei Medical, Shandong, China12; CYPHER®; Cordis, Johnson & Johnson, Miami Lakes, FL, USA) and the paclitaxel-eluting stent (TAXUS™; Boston Scientific, Marlborough, MA, USA) were used. All patients were pretreated with aspirin and clopidogrel. Patients who were not pretreated received 300 mg aspirin and a loading dose of clopidogrel of at least 300 mg before the index procedure. Heparin was administered during the procedure to maintain an activated clotting time ≥250 seconds. After the procedure, all patients received 300 mg aspirin per day for one month, followed by 100 mg per day indefinitely, as well as 75 mg clopidogrel per day for at least 12 months.
CLINICAL OUTCOMES
The primary endpoint was the incidence of major adverse cardiac events (MACE), a composite of cardiac death, myocardial infarction (MI) and repeat revascularisation at five-year follow-up. Death was considered to be of cardiac cause unless a non-cardiac cause could be identified. MI was defined as a rise in plasma level of creatinine kinase (CK)-MB/troponin ≥3 times the upper limit of normal. Stent thrombosis (definite and probable) was defined according to the Academic Research Consortium (ARC) classification13. Routine angiographic follow-up was recommended for all patients at around eight months (or earlier if clinically indicated). Clinical follow-up protocol has been described previously9. In brief, clinical follow-up was conducted with office visits or telephone contacts at one, six, and 12 months, and yearly thereafter. All events were adjudicated by an independent clinical events committee, comprised of interventional and non-interventional cardiologists not participating in the study.
DEFINITIONS AND COMPLETENESS OF REVASCULARISATION
CR included patients who had successful revascularisation of all diseased segments (defined as a diameter stenosis ≥50%, visually assessed) with diameter ≥1.5 mm (the SYNTAX definition) with PCI, either during the index hospitalisation or within 30 days after the index procedure (staged revascularisation), but before a new MI or urgent target lesion revascularisation8. PCR included patients who did not receive revascularisation for the diseased segments with diameters between 1.5 mm and 2.5 mm. ICR included patients who did not achieve revascularisation for all diseased segments with diameters ≥2.5 mm6. The revascularisation classification was performed by two independent experienced analysts in a core laboratory (China Cardiovascular Research Foundation [CCRF], Beijing, China). The SYNTAX score was calculated using the online calculator (www.syntaxscore.com).
STATISTICAL ANALYSIS
Continuous variables are expressed as mean±standard deviation and categorical variables are shown as counts and percentages of the total. Chi-square or Fisher’s exact tests were used for comparison of categorical variables, whereas the Student’s t-test and Kruskal-Wallis test were used to compare normally distributed and non-normally distributed continuous data, respectively. Comparison of five-year clinical outcomes among groups was conducted using the Kaplan-Meier method and the log-rank test.
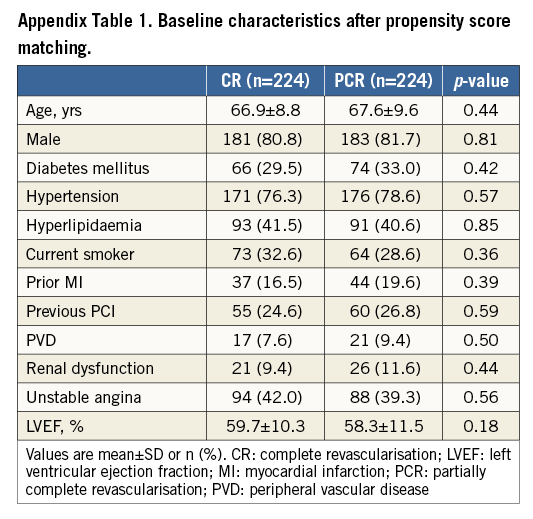
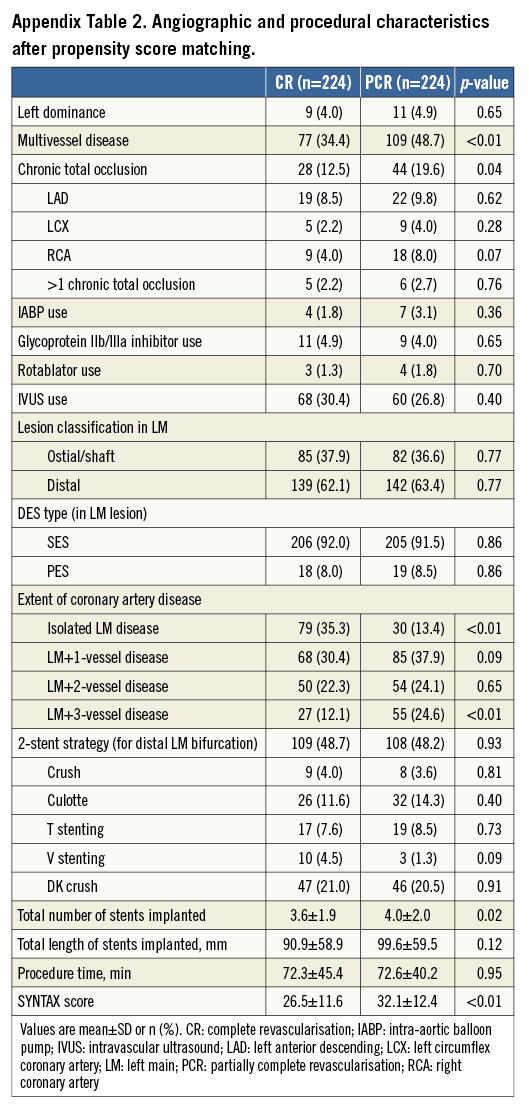
For maximal elimination of the difference of clinical and lesion characteristics between the CR and PCR groups, a propensity score matching was conducted, based on a custom dialogue in SPSS with R plug-in14. For development of propensity score matching pairs with a 1:1 match (nearest neighbour), a hierarchical cluster was used. The following variables were selected to calculate the propensity score by binary logistic regression: age, gender, diabetes mellitus, hypertension, hyperlipidaemia, current smoking status, prior MI, previous PCI, peripheral vascular disease, renal dysfunction, unstable angina, left ventricular ejection fraction, left dominance, multivessel disease, chronic total occlusion, intra-aortic balloon pump used, glycoprotein IIb/IIIa inhibitor use, lesion classification in the left main, DES type, stent strategy for distal left main bifurcation, total number of stents implanted, total length of stents implanted and the SYNTAX score.
To confirm the concept of ICR as an outcome of poor clinical comorbidity and anatomical coronary complexity, a multivariable logistic regression analysis was performed with a stepwise elimination procedure, where the independent variables were entered into the model at the 0.1 significance level. The following variables considered as possible predictors were included for analysis: age, gender, body mass index, diabetes, hypertension, hyperlipidaemia, smoking, history of MI, unstable angina, peripheral arterial disease, renal dysfunction, left ventricular ejection fraction, left arterial dominance, any calcification, any tortuosity, any thrombus, any lesion length >20 mm, any bifurcation/trifurcation, and the presence of CTO, multivessel disease, and distal ULMCA bifurcation. If the two variables were highly correlated with each other (r>0.5 and p<0.05), only the variable with a higher level of significance was included in the multivariable model. A probability value of <0.05 was considered statistically significant. All analyses were undertaken using SPSS, Version 20.0 (IBM Corp., Armonk, NY, USA) and STATA 12.0 (Stata Corp., College Station, TX, USA).
Results
BASELINE AND PROCEDURAL CHARACTERISTICS
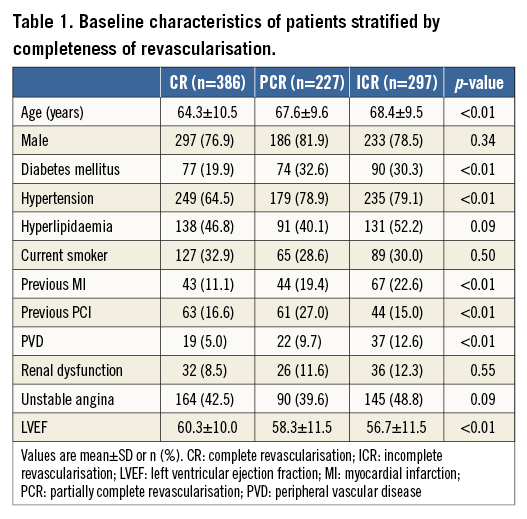
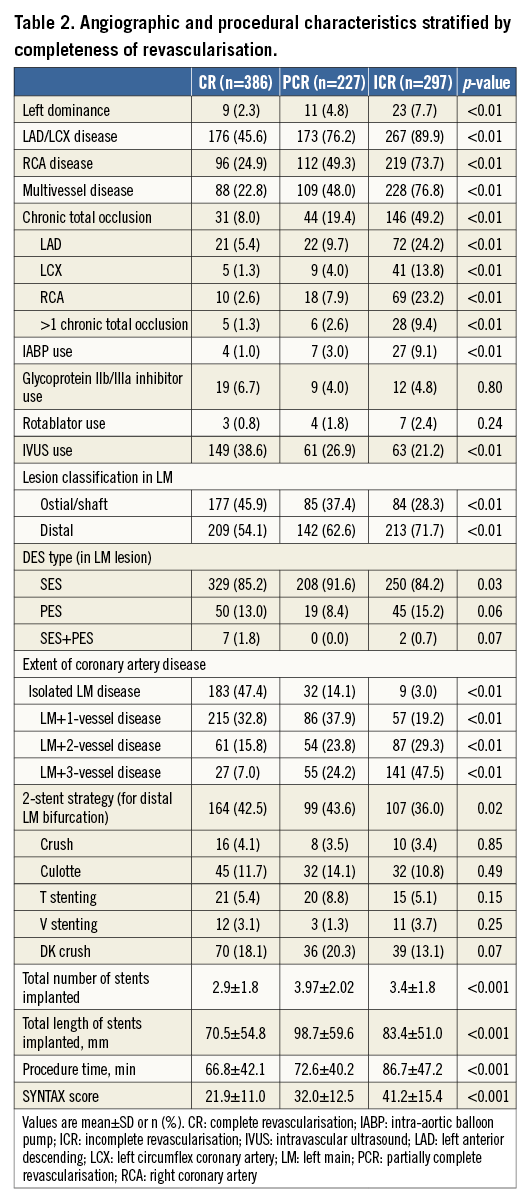
Out of 910 patients included in this study, CR was achieved in 386 (42.4%), PCR in 227 (25.0%), and ICR in 297 (32.6%) (Figure 1). The baseline, angiographic, and procedural characteristics of patients in these groups are shown in Table 1 and Table 2. Patients achieving CR were younger, had a higher left ventricular ejection fraction (LVEF), fewer comorbidities and lower SYNTAX score, and subsequently had a lesser number of DES implanted compared with the PCR and ICR groups.
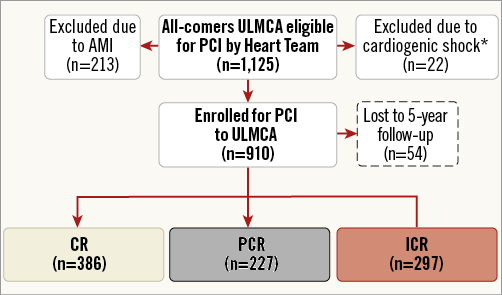
Figure 1. Study flow chart. *20 patients with cardiogenic shock presented as AMI. AMI: acute myocardial infarction; CR: complete revascularisation; ICR: incomplete revascularisation; PCI: percutaneous coronary intervention; PCR: partially complete revascularisation; ULMCA: unprotected left main coronary artery
IMPACT OF REVASCULARISATION STRATEGIES
ICR was associated with a significantly higher rate of adverse outcomes compared with the CR and PCR groups at five-year follow-up (Figure 2, Figure 3). Patients with CR had a significantly lower rate of MACE compared with PCR (15.5% vs. 22.5%, p=0.02) (Figure 3A); however, the incidence of all-cause death in patients with CR and PCR was similar (6.2% vs. 7.0%, p=0.62) (Figure 3B).
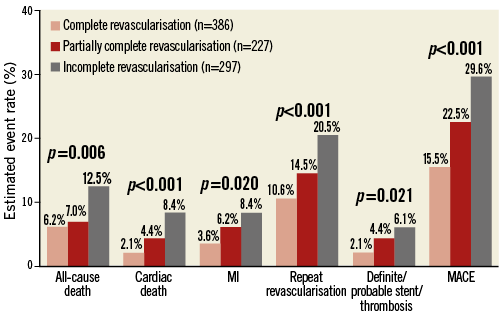
Figure 2. Five-year clinical outcomes. Comparison (log-rank tests) of clinical outcomes at five-year follow-up among complete, incomplete, and partially complete revascularisation groups. MACE: major adverse cardiac events; MI: myocardial infarction
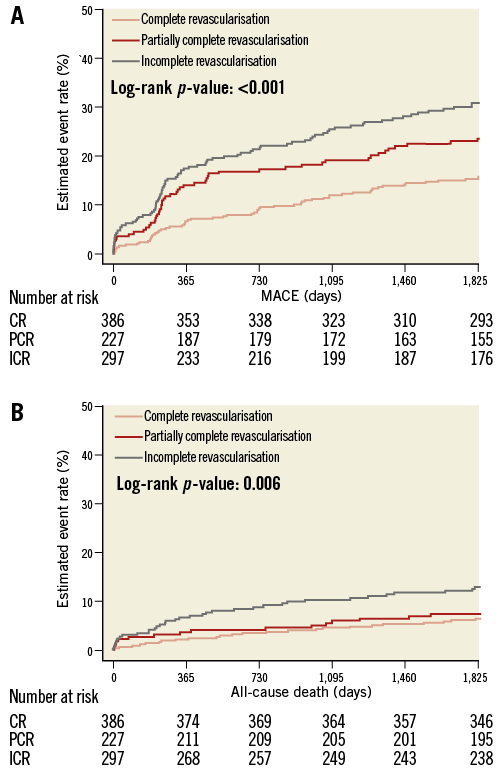
Figure 3. Time-to-event curves for five-year MACE and mortality. A) A lower incidence of MACE was observed in patients achieving angiographic CR or PCR. B) The incidence of all-cause death in the CR and PCR groups was similar, and significantly lower than in the ICR group. CR: complete revascularisation; ICR: incomplete revascularisation; MACE: major adverse cardiac events; PCR: partially complete revascularisation
PROPENSITY SCORE MATCHING BETWEEN CR AND PCR
After propensity score matching, the clinical and lesion characteristics between the CR and PCR groups were well matched (Appendix Table 1, Appendix Table 2). There were no significant differences in all clinical outcomes between the CR and PCR groups (Table 3, Appendix Figure 1). The PCR group had similar incidences of MACE and mortality compared with the CR group (HR: 1.16, 95% CI: 0.78-1.74, p=0.46; HR: 1.27, 95% CI: 0.61-2.63, p=0.53, respectively).
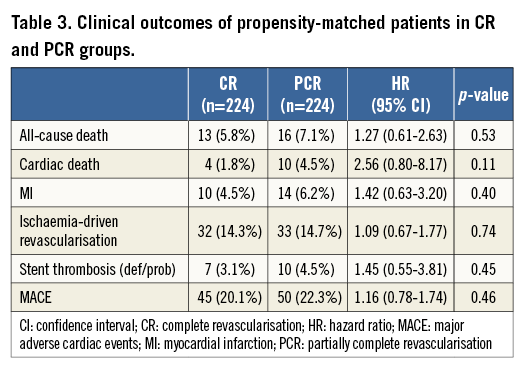
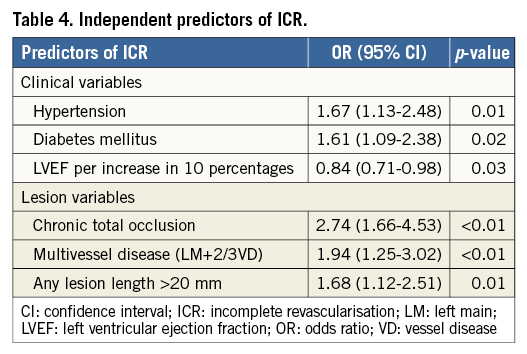
PREDICTORS OF INCOMPLETE REVASCULARISATION
The results of multivariable logistic regression analysis showed that ICR is a marker of worse baseline clinical and anatomical characteristics (Table 4). Of all the clinical risk factors, diabetes, hypertension and left ventricular ejection fraction appeared to be independent predictors of ICR. Among the anatomical risk factors, chronic total occlusion (odds ratio [OR]: 2.74, 95% CI: 1.66-4.53, p<0.01), multivessel disease (OR: 1.94, 95% CI: 1.25-3.02, p<0.01) and any lesion length >20 mm (OR: 1.68, 95% CI: 1.12-2.51, p<0.01) were independent predictors of ICR.
Discussion
This post hoc analysis of prospectively collected and independently adjudicated registry data has confirmed our hypothesis that patients with ULMCA disease achieving partially complete revascularisation with DES have long-term prognosis similar to those achieving complete revascularisation. Conversely, patients with incomplete revascularisation had a significantly higher rate of adverse events.
PCI has become an acceptable alternative to CABG for the treatment of ULMCA stenosis in international guidelines15. It is not an uncommon practice to prefer PCI for the treatment of patients with ULMCA disease, especially in Asia1,16. The CREDO-Kyoto registry reported that patients with ULMCA disease in the PCI arm have similar long-term clinical prognosis compared with the CABG arm, especially in patients with a low or intermediate SYNTAX score4.
The concept of ICR has gained significant attention as it has been shown to correlate with poor outcomes5,8. These studies have used a very stringent definition of CR, which may not be readily achieved in routine clinical practice. Although there are studies challenging the correlation between ICR and adverse clinical outcomes after either PCI or CABG6,7,17-19, recent meta-analyses have demonstrated that CR is associated with better outcomes20. In the present study, we have confirmed that ICR is associated with significantly adverse clinical outcomes in patients with ULMCA disease at five-year follow-up. Moreover, we also demonstrated that ICR is an outcome of poor clinical and anatomical characteristics. Indeed, the SYNTAX trial reported that the presence of CTO, the number of lesions and the presence of bifurcation/trifurcation lesions were the strongest predictors for angiographic ICR8. Thus, it may be inappropriate to compare the clinical outcomes between CR and ICR by adjusting the baseline variables.
Recently, the concept of “residual” SYNTAX score (rSS) has been proposed to quantify the residual burden of disease after PCI and has been shown to correlate with clinical outcomes21. The study of quantification of incomplete revascularisation from our group validated the prognostic value of rSS in the SYNTAX trial22. However, calculation of rSS used a definition of 1.5 mm. The definition of CR based on the SYNTAX definition may not reflect real-world interventional practice. The area of myocardium supplied by small vessels is limited, and trying to salvage this small area with an aggressive procedure may be counterproductive. The operator has to judge the technical difficulties, clinical risk profile and risk of complications on a case-by-case basis23,24. Our study, for the first time, has demonstrated that PCR has similar clinical outcomes compared with CR. These findings may have important clinical implications for the revascularisation strategy in routine practice and future clinical trials.
STUDY LIMITATIONS
This study has several limitations. First, it is a post hoc analysis of a registry with the inherent limitations of such data. However, it is a large-scale study with five-year follow-up. All data were collected prospectively and events were adjudicated independently. Second, the SYNTAX score and the definition of CR based on the SYNTAX classification were not assessed prospectively. However, this was analysed by two independent experienced operators blinded to the clinical outcomes: this approach has been shown to provide higher accuracy than prospectively calculated scores by site25. Third, the incidence of repeat revascularisation may be influenced by the scheduled angiographic follow-up at eight months; however, it would have affected all groups equally, so its impact on the comparison between revascularisation strategies is likely to be limited. Finally, procedural factors, such as the use of IVUS or glycoprotein IIb/IIIa inhibitors, which were left at the discretion of the operators, may also influence ICR. However, we included these procedural factors into a multivariable regression model and no procedural factor was found to be an independent predictor of ICR.
Conclusions
PCR has clinical outcomes similar to CR in patients with ULMCA disease treated with DES. ICR has worse long-term clinical outcomes than CR and PCR, indicating that at least all vessels larger than 2.5 mm should be revascularised.
| Impact on daily practice Incomplete revascularisation has been shown to correlate with poor outcomes after PCI. However, overzealous attempts to achieve complete revascularisation for diffuse disease in distal or small calibre vessels may also lead to adverse outcomes. Our data, whilst confirming the importance of the completeness of revascularisation, have shown that patients who did not receive revascularisation for the diseased segments with diameters <2.5 mm had acceptable outcomes. However, it could be argued that a cut-off of 2.25 mm may be more appropriate. Further prospective studies are warranted to evaluate the concept of partially complete revascularisation, especially in the era of new-generation DES. |
Guest Editor
This paper was guest edited by Antonio Colombo, MD; S. Raffaele Scientific Institute, Milan, Italy.
Acknowledgements
We express our gratitude to all of the participants for their active and long-term cooperation. We are also thankful to Hai-Mei Xue, Jing Kan, Yin-Yin Zhao, and Ling Lin for their invaluable work in collecting the data.
Funding
This study was funded by the Jiangsu Provincial Outstanding Medical Program (JPOMP-20041230).
Conflict of interest statement
The authors have no conflicts of interest to declare. The Guest Editor has no conflicts of interest to declare.
Supplementary data
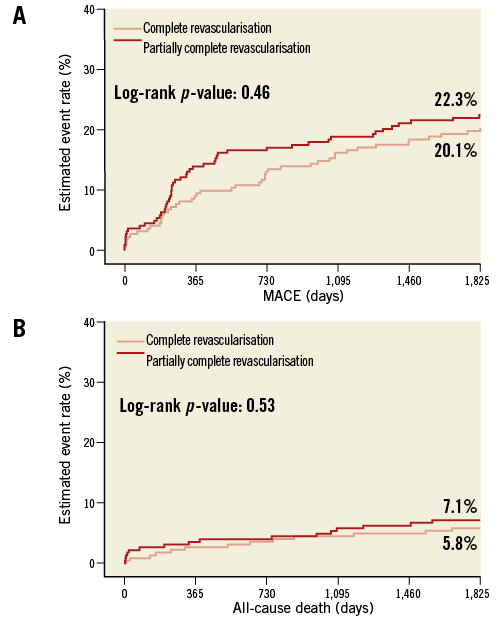
Appendix Figure 1. Time-to-event curves for 5-year MACE and mortality after propensity matching. Similar incidences of MACE (A) and all-cause mortality (B) were observed in patients achieving angiographic CR or PCR after propensity matching. CR: complete revascularisation; MACE: major adverse cardiac events; PCR: partially complete revascularisation