Abstract
Aims: The aim of this study was to evaluate very long-term clinical outcomes and potential predictors after percutaneous coronary intervention (PCI) with bare metal stents (BMS) for unprotected left main coronary artery disease (ULMCAD).
Methods and results: From March 1991 to August 2001, 151 patients who underwent PCI with BMS for ULMCAD were investigated retrospectively. The patient-oriented major adverse cardiac events (MACE) were defined as the occurrence of all-cause death, any MI, and any coronary revascularisation. The median follow-up duration was 10.5 years. The mean age was 69.9±11.5 years, and 106 patients (70.2%) were male. At 10 years, the incidences of cardiac death (CD), target lesion revascularisation (TLR) and patient-oriented MACE were 11.1%, 25.2% and 81.9%, respectively. In multivariate analysis, the pre-reference diameter of the left main trunk (LMT) was significantly associated with TLR (adjusted hazard ratio [HR] [95% confidence interval (CI)], 0.28 [0.14-0.54], p<0.001) and the SYNTAX score remained an independent predictor of patient-oriented MACE (adjusted HR [95% CI], 1.03 [1.007-1.05], p=0.009).
Conclusions: The pre-reference diameter of LMT was significantly associated with TLR, and the SYNTAX score significantly predicted the risk of patient-oriented MACE at 10 years. BMS implantation for larger size of ULMCAD with a lower SYNTAX score was feasible for up to 10 years.
Abbreviations
BMS: bare metal stents
DES: drug-eluting stents
PCI: percutaneous coronary intervention
CABG: coronary artery bypass grafting
CI: confidence interval
HR: hazard ratio
CD: cardiac death
MI: myocardial infarction
TLR: target lesion revascularisation
ULMCAD: unprotected left main coronary artery disease
Introduction
The SYNTAX study (SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery) demonstrated that the SYNTAX score1 was an important tool in assessing the optimal revascularisation strategy between percutaneous coronary interventions and coronary artery bypass grafting in patients with complex coronary artery disease2. Furthermore, the SYNTAX score was a useful tool for predicting major adverse cardiac events at one year in patients with unprotected left main coronary artery disease (ULMCAD)3. From the observational analysis of the SYNTAX study, patients with ULMCAD who underwent percutaneous coronary intervention (PCI) using drug-eluting stents (DES) had safety and efficacy outcomes comparable to coronary artery bypass grafting (CABG) at one year4. Since their introduction, DES have become widely used for the treatment of ULMCAD5-8. While DES have shown lower incidences of myocardial infarction and target lesion revascularisation compared with bare metal stents (BMS)7-9, the long-term results of DES implantation for ULMCAD beyond five years have not been well clarified10,11. Furthermore, DES have a potential risk for very late stent thrombosis or late catch-up phenomenon12-15.
We have already reported over 10-15 years of clinical outcomes for patients with successful BMS deployment16,17 and Park et al have also shown long-term outcomes using BMS in patients with ULMCAD compared to CABG10. However, very long-term outcomes and potential predictors, including the SYNTAX score11 in patients with BMS for ULMCAD, remain unclear.
In this study, we analysed very long-term (over 10 years) clinical outcomes after BMS implantation in patients with ULMCAD and evaluated its potential risk factors, including the SYNTAX score, which could be an independent predictor of the clinical outcomes with BMS.
Methods
PATIENT SELECTION
From March 1991 to August 2001, 163 consecutive patients underwent PCI with BMS for ULMCAD at Kokura Memorial Hospital, Japan. Of these, the left main trunk was haemodynamically protected by CABG in 12 patients. This study population comprised 151 patients who underwent PCI with BMS for ULMCAD. All patients were informed about the risk of the procedure and alternative treatment methods, and then provided written informed consent. Because of the retrospective enrolment, written informed consent for the follow-up analysis was waived. The study protocol was approved by the institutional review board of Kokura Memorial Hospital. Stent implantation was performed according to standard techniques18. The SYNTAX score was calculated by the software downloaded at the website (http://www.syntaxscore.com). The SYNTAX score was evaluated by two cardiologists who were not informed of the clinical outcomes. In cases in which the cardiologists did not concur, they rechecked the angiography together and recalculated the score. All clinical information was collected from hospital records or telephone contact with the patients, the family members or the primary care physician. In cases of any cardiovascular events such as death, myocardial infarction (MI), or coronary revascularisation, we reviewed the hospital records or sent inquiries to the attending physician. Data on the angina status, according to the Canadian Cardiovascular Society (CCS) classification, were collected during late follow-up angiography19. Quantitative coronary angiographic analysis at the index procedure and follow-up angiography were performed with the Cardiovascular Angiography Analysis System II. A detailed description of the method and reproducibility of quantitative angiographic analysis in our laboratory has been reported previously20.
DEFINITIONS
The unprotected left main coronary artery was defined when there were no patent coronary artery bypass grafts to the left ascending artery (LAD) or left circumflex artery (LCX). The left main disease was defined as stenosis in the left main coronary artery of at least 50% by visual assessment, or left main equivalent (defined as at least 50% stenosis of the ostium of the left anterior descending artery or the left circumflex) with or without stenosis in other vessels. Cardiac death was defined as any death with cardiovascular cause, all procedure-related deaths or any death with unknown cause within four years after index PCI. MI was defined as a clinical event with typical electrocardiographic change, or elevation of troponin or creatine kinase. Target lesion MI was defined as MI that was not clearly attributable to a non-target vessel. Target lesion revascularisation (TLR) was defined as any repeat revascularisation (regardless of PCI or coronary artery bypass graft) performed for restenosis inside the placed stent or within the 5 mm segments adjacent to the stent. Stent thrombosis (ST) was defined according to the Academic Consortium definitions21, and definite ST was evaluated on a patient-level basis in the current analysis. Any MI was defined as MI that occurred in the target and non-target vessel territory, and any coronary revascularisation was defined as any repeat revascularisation for all target or non-target vessels21. The patient-oriented major adverse cardiac events (MACE) were defined as the occurrence of all-cause death, any MI or any coronary revascularisation. Diabetes mellitus was diagnosed when a patient was treated with insulin or oral hypoglycaemic drugs, when casual levels of plasma glucose were higher than 200 mg/dl, fasting levels of plasma glucose were higher than 126 mg/dl or HbA1c was higher than 6.5% in patients without need for treatment with insulin or oral hypoglycaemic drugs. Dyslipidaemia was diagnosed when a patient was treated with lipid-lowering agents, when the casual total cholesterol level was higher than 220 mg/dl or the casual low-density lipoprotein level was higher than 140 mg/dl. Chronic kidney disease (CKD) was defined as an estimated glomerular filtration rate less than 60 ml/min/1.73 m2. Current smoking included current smokers and patients who quit smoking within six months. Emergency PCI was defined as PCI performed within 24 hours after clinical diagnosis. Complete revascularisation was defined when all coronary lesions (more than 50% stenosis) were treated by PCI (stent deployment or balloon angioplasty) within one month after the index procedure.
STATISTICAL ANALYSIS
In this study, the incidence of all-cause death, target lesion non-fatal MI, TLR and patient-oriented MACE was evaluated. Potential risk factors were also analysed for each category.
Continuous variables were presented as the mean±SDs or as median and interquartile range (IQR) and were compared using the Student’s unpaired t-test or Wilcoxon rank sum test depending on their distributions, respectively. Categorical variables were presented as counts and percentages and were compared with Fisher’s exact test. Survival curves were generated by the Kaplan-Meier method, and were evaluated by the log-rank test.
To adjust for a range of potential confounders, multivariate analysis of independent predictors of all-cause death, target lesion non-fatal MI, TLR and patient-oriented MACE was performed with a Cox-proportional hazard regression model. We included variables that were considered as possible predictors, such as age, male gender, hypertension, diabetes mellitus, dyslipidaemia, current smoking, CKD, poor LV function defined as less than 40% of the left ventricular ejection fraction, previous history of PCI or CABG, clinical presentation at the time of procedure, emergency setting, complete revascularisation, lesion location of the left main trunk (ostium, shaft or distal), the number of implanted stents, stent profile (size and length), quantitative coronary analysis (pre-lesion diameter and length) and the SYNTAX score. Variables with p values <0.1 on univariate analysis were selected in the final model. All statistical analyses were performed using JMP version 8 (SAS Institute Inc., Cary, NC, USA).
Results
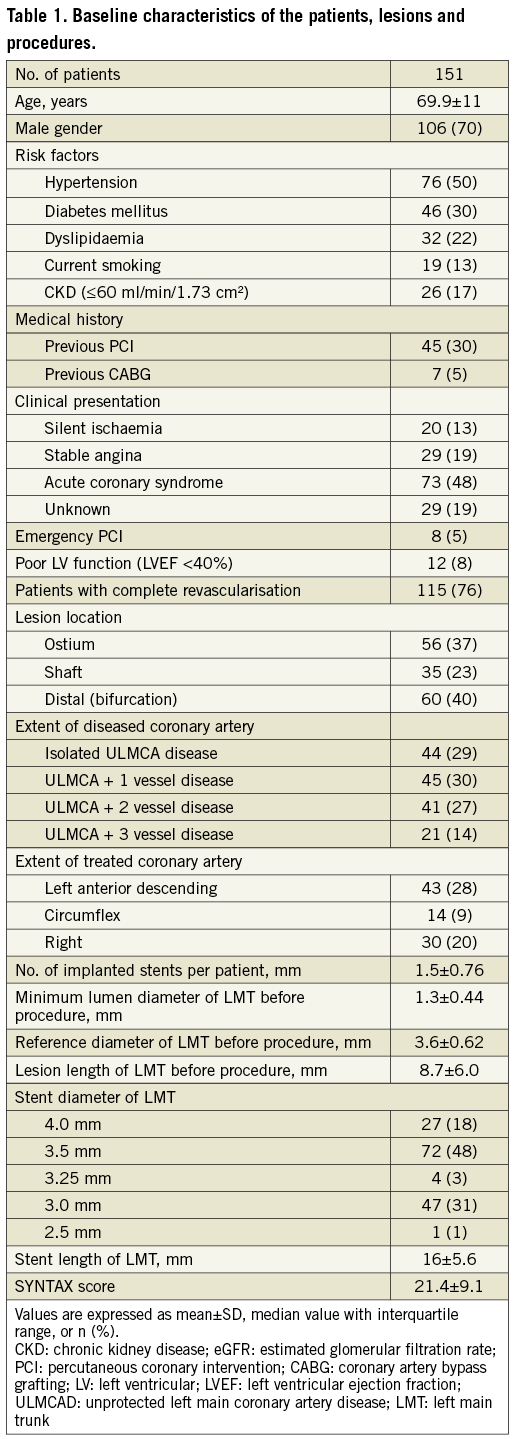
PATIENTS, LESION AND PROCEDURAL CHARACTERISTICS
The baseline characteristics of patients, lesions and procedures are shown in Table 1. Since the patients were selected for the treatment of ULMCAD with PCI, 60% of the left main trunk lesions were anatomically simple lesions, such as the ostium or shaft. As stents were placed in relatively large arteries, 66% of the deployed stents for left main trunk were over 3.5 mm in diameter. The mean SYNTAX score was 21.4±9.1. Although ULMCAD itself was a high-risk clinical feature during the study period, this study population reflected relatively classical indications for coronary stenting.
CLINICAL OUTCOMES
The median follow-up period of 95 survivors out of 151 patients at 10 years was 10.5 years (interquartile range [IQR], 7.4 to 12.2 years), and clinical follow-up information was obtained from 137 (91%) and 122 patients (81%) at five and 10 years, respectively.
The cumulative incidences of each clinical event are shown in Table 2. At 10 years, the incidences of cardiac death, target lesion non-fatal MI and TLR were 11.1%, 2.3% and 24.5%, respectively, and the cumulative incidence of cardiac death, target lesion non-fatal MI or TLR was 35.9% (Figure 1A). Clinical presentations at the time of TLR were as follows: CCS more than three in 12 patients (36%), CCS less than two with angiographic binary restenosis in three patients (9%), asymptomatic with positive treadmill stress test in one patient (3%), and asymptomatic with angiographic binary restenosis in 17 patients (52%). Target lesion CABG was performed in 17 patients during the study period. On the other hand, the incidences of all-cause death, any MI, and any coronary revascularisation were 41.2%, 4.5%, and 67.8% respectively, and the cumulative incidence of the patient-oriented MACE was 81.2% (Figure 1B). Definite ST occurred in six patients during the study period and the incidences at one, five and 10 years were 2.7%, 3.7% and 4.7%, respectively. In patients with definite ST, three patients died of acute MI, and three patients were successfully recanalised by emergency PCI.
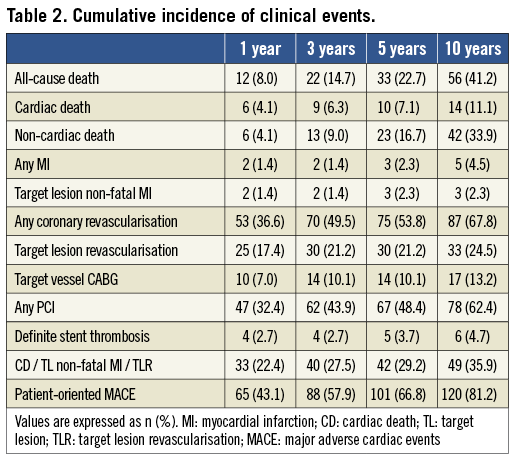
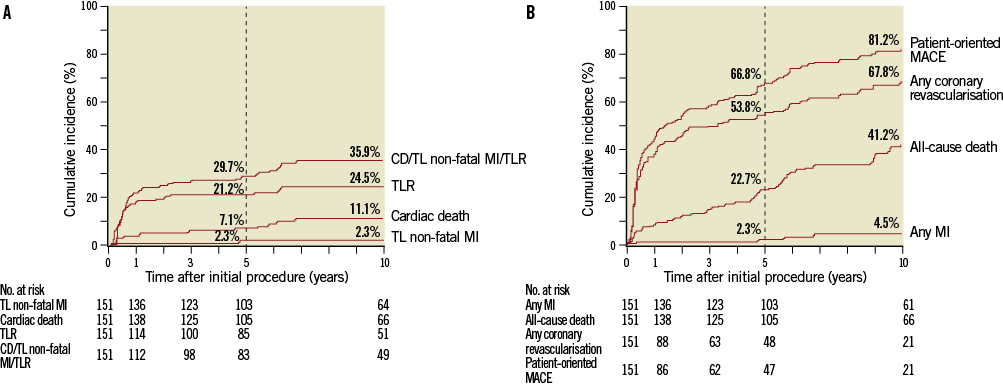
Figure 1. Cumulative incidences of the device-oriented (A) and patient-oriented (B) outcomes. Patient-oriented MACE included all-cause death, any MI, or any coronary revascularisation. MI: myocardial infarction; CD: cardiac death; TL: target lesion; TLR: target lesion revascularisation; MACE: major adverse cardiac events
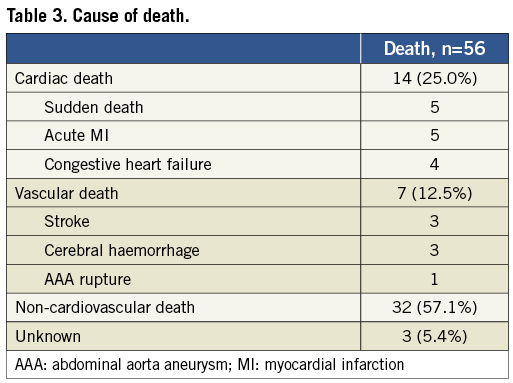
The causes of death are shown in Table 3. Among the 56 patients who died during the study period, cardiac death occurred in 14 patients (25.0%), including five patients (8.9%) with sudden death. Because three patients died due to an unknown cause more than four years (2,027, 2,083 and 3,277 days, respectively) after index PCI, they were included in non-cardiac death. Vascular death occurred in seven patients (12.5%) and non-cardiovascular death occurred in 32 patients (57.1%).
UNIVARIATE AND MULTIVARIATE ANALYSIS
Potential predictors of all-cause death, target lesion non-fatal MI, TLR and patient-oriented MACE were evaluated by the Cox-proportional hazard regression model (Table 4). Regarding target lesion non-fatal MI, there was no significant potential confounder based upon the univariate analysis.
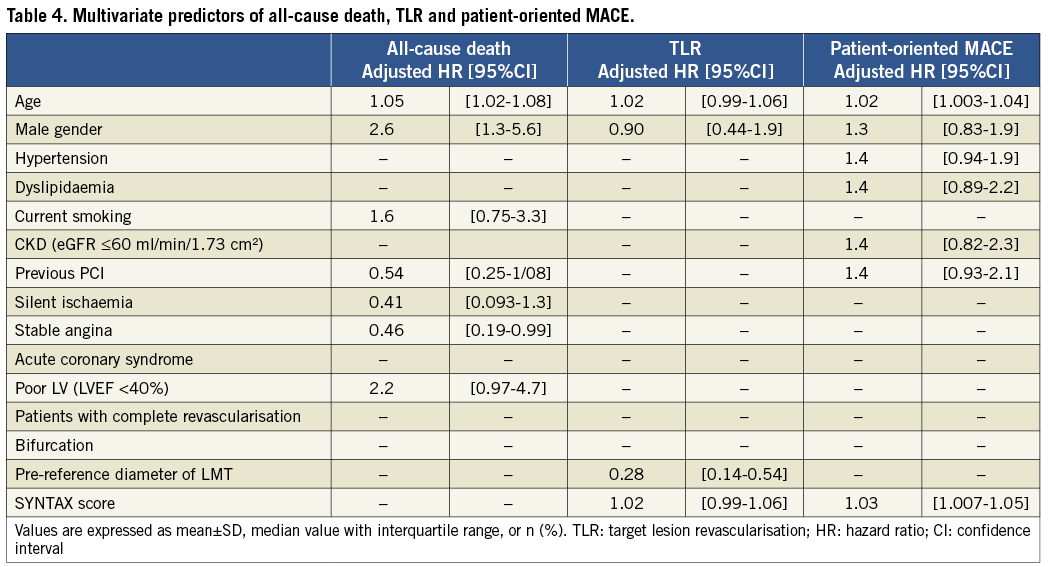
After adjustment for potential confounders, older age (p=0.001), male gender (p=0.005) and the presence of stable angina (p=0.048) were significantly associated with all-cause death, the pre-reference diameter of the left main trunk (p<0.001) significantly predicted the risk of TLR, and older age (p=0.02) and the SYNTAX score (p=0.009) remained independent predictors of patient-oriented MACE at 10 years.
ANALYSIS OF THE SYNTAX SCORE TERTILES
The cumulative incidences of TLR and patient-oriented MACE across the lower and higher SYNTAX score groups are shown in Figure 2A and Figure 2B, respectively. The lower and higher SYNTAX score groups were defined as a lower-score group, 0 to 22, and a higher-score group, more than 22, according to the SYNTAX trial4. At 10 years, the incidences of TLR were 16.9% and 37.3% in patients in the lower and higher SYNTAX score groups, respectively (log-rank test, p=0.008). In the same period, the incidence of patient-oriented MACE was 75.4% in the lower SYNTAX score group and 90.1% in the higher SYNTAX score group (log-rank test, p=0.001). Compared to patients with a higher SYNTAX score, patients with lower SYNTAX scores had higher incidences of complete revascularisation (p<0.001), were less likely to be implanted for distal bifurcation lesion (p=0.006), required fewer stents for the left main trunk lesion (p<0.001) and were implanted with bigger (p<0.001) and shorter (p<0.001) stents for the left main trunk lesion.
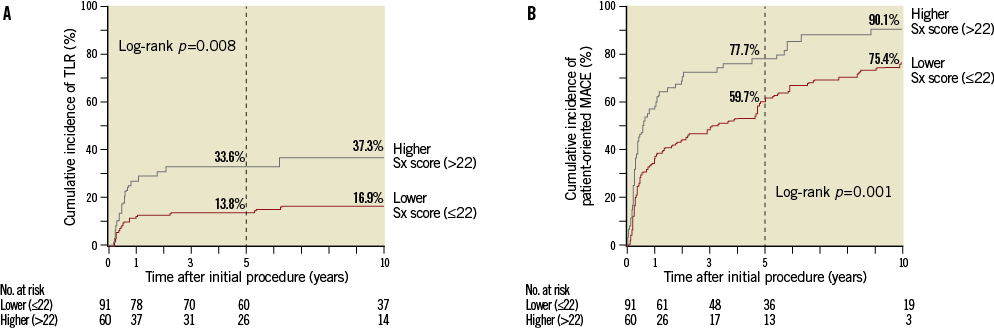
Figure 2. Cumulative incidences of target lesion revascularisation (TLR) (A) or patient-oriented MACE (B) according to the SYNTAX score. Regarding the SYNTAX score tertiles, the lower score group was defined as the one where the SYNTAX score was from 0 to 22, and the higher score group more than 22. Sx score: SYNTAX score.
Discussion
In this study, we investigated very long-term clinical endpoints in patients treated with BMS for ULMCAD. The incidences of all-cause death, cardiac death, target lesion non-fatal MI, TLR and patient-oriented MACE at 10 years were obtained, and potential predictors were also revealed.
The most important findings are as follows: (1) BMS implantation for ULMCAD showed favourable results even at 10 years; (2) the SYNTAX score was an independent predictor for patient-oriented MACE at 10 years in patients with ULMCAD after BMS implantation; (3) the pre-reference LMT diameter was associated significantly with the risk of TLR at 10 years.
The event-free incidence of the device-related composite, including cardiac death, target lesion non-fatal MI and TLR, was favourable (64.1%) at 10 years, although the event-free incidence of the patient-oriented composite endpoint, including all-cause death, any MI and any coronary revascularisation, was low (18.8%) at 10 years. Furthermore, the major component of the device-related composite was TLR, which was driven by initial follow-up angiography in asymptomatic patients. Although this favourable outcome in this study might be related to the characteristics of short lesions with large artery size in our patients, these were not significant variables in multivariate analysis. In addition, Park et al10 reported a long-term clinical follow-up study of patients with BMS and CABG patients, up to 10 years, and the cumulative incidences of each long-term outcome were: all-cause death, 15.9%; cardiac death, 6.9%; and TLR 24.9%. The incidence of TLR was consistent with the present study, although the incidences of all-cause death or cardiac death in the previous report were relatively low, due primarily to the younger patient cohort.
The SYNTAX score effectively allowed for stratification of the clinical risk in the patients with ULMCAD, even with BMS implantation. With regard to the SYNTAX score, the patients with a lower score showed a significantly lower event incidence at 10 years than those with a higher score. According to the studies using DES for ULMCAD, Mehilli et al22 reported that the two-year composite endpoint, including death, MI and reintervention in patients with ULMCAD was 20.6-21.3% using sirolimus-eluting stents or paclitaxel-eluting stents (PES), and Morice et al4 reported that, in the SYNTAX trial of patients for ULMCAD, repeat revascularisation at one year was 12.0%. Although this study had no control group, implantation for ULMCAD with a lower SYNTAX score was comparable to DES.
Baseline characteristics showed apparent differences between the lower and the higher SYNTAX score groups. The larger and shorter stents were implanted in patients with the lowest SYNTAX score tertile rather than higher SYNTAX score tertiles. In this study, the mean stent diameters of the lower and the higher SYNTAX score groups were 3.51 mm and 3.28 mm, and the mean stent lengths of the lower and the higher SYNTAX score groups for left main trunk were 13.8 mm and 18.1 mm, respectively. These differences could effectively relate to clinical endpoints in patients with BMS for ULMCAD between the SYNTAX score tertiles. Capodanno et al3 have suggested the efficacy of the SYNTAX score for predicting clinical endpoints such as cardiac death and a composite of major adverse cardiac events at one year; however, data on the effectiveness of the SYNTAX score and dividing the groups by the SYNTAX score has been lacking, especially long-term results. This study was important for being the first to point out the association between very long-term clinical outcomes and the SYNTAX score in patients with BMS for ULMCAD, and could provide baseline data to compare with future studies.
The variable of pre-reference LMT diameter was significantly associated with TLR in multivariate analysis in this study. Some studies have reported that the coronary stenting for a large coronary artery with BMS has shown similar clinical outcomes compared to those with DES23-25, and those results have also shown the favourable clinical results of both stents over 3 mm in diameter. Late lumen loss is a critical problem after BMS implantation26; however, the larger pre-reference diameter of a target artery could cancel such a negative effect even for ULMCAD, and was able to decrease the incidences of TLR and device-related composite endpoints21.
It is an interesting point that pre-reference LMT diameter and the SYNTAX score are evaluated or calculated based only on coronary angiography. In fact, it could be possible to predict clinical outcomes in patients with ULMCAD before performing the treatment procedure. Additional data would help to establish the efficacy of measuring the pre-reference diameter or the SYNTAX score to distinguish the group with good clinical outcomes, even when BMS is used for ULMCAD.
Study limitations
This study has some limitations. First, we could not use a potentially effective scoring system such as the EuroSCORE or STS score in this study. A decade ago, coronary interventions for ULMCAD had been performed in highly selected patients. Moreover, the study population might include those patients who were thought to be at high risk for CABG because of comorbidities or adverse systemic conditions (such as patients with a high EuroSCORE or those with a high STS score). This selection bias should be taken into consideration. Second, the average risk was relatively low according to the SYNTAX score. Third, our study was observational, and almost all choices of revascularisation were at the discretion of the operator and/or patient. Fourth, the current study was a single-centre study. Fifth, we did not evaluate re-repeat revascularisation in this long follow-up study.
Conclusions
In multivariate analysis, the pre-reference diameter of the left main trunk was an independent predictor of TLR, and the SYNTAX score significantly predicted the risk of patient-oriented MACE for patients with ULMCAD after BMS implantation at 10 years. BMS for ULMCAD showed favourable very long-term clinical outcomes, especially in patients with larger pre-reference diameter of the left main trunk or lower SYNTAX scores.
Acknowledgements
The authors are indebted to Naoka Katsumi, Akiko Egami, Natsue Nagata, Yukie Ochi, Masako Hosono, Yoshiharu Ohata, and Itsuo Yuda for assistance in collecting follow-up information.
Conflict of interest statement
The authors have no conflicts of interest to declare.

