Abstract
Aims: Limited long-term data are available to support drug-eluting stent (DES) unprotected left main (LM) intervention. We sought to evaluate long-term outcomes of LM intervention with paclitaxel-eluting stents.
Methods and results: In this prospective multicentre registry, 291 patients with unprotected LM stenosis underwent percutaneous revascularisation with the TAXUS® Express® stent, using a consistent technical approach for both ostial/shaft and bifurcation lesions (provisional side branch stenting). At five years (n=263), the cumulative incidence of major adverse cardiac events (MACE) and cardiac death were 23.6% and 12.5%, respectively. Myocardial infarction (MI) occurred in 16 patients (6.1%), definite stent thrombosis in 0.4%, and target lesion revascularisation (TLR) was required in 10.3%. Patients with distal LM lesions requiring two-stent procedures had increased MACE compared with those with single-stent interventions (34.1% vs. 17.8%, p=0.009). This was primarily driven by an increased incidence of cardiac death (18.2% vs. 8.5%, p=0.05). Diabetes was associated with increased TLR and was an independent predictor of MACE at five years (odds ratio [OR] 2.10, 95% confidence interval [CI] 1.10-3.99, p=0.02).
Conclusions: This study confirms the long-term safety and efficacy of the TAXUS® DES in unprotected LM stenting. Diabetes and the need for a second stent in distal LM interventions were associated with an increased risk of adverse outcomes.
Abbreviations
CABG: coronary artery bypass grafting
CAD: coronary artery disease
DES: drug-eluting stent
LM: left main
MACE: major adverse cardiac events
MI: myocardial infarction
PCI: percutaneous coronary intervention
SB: side branch
ST: stent thrombosis
TLR: target lesion revascularisation
SYNTAX: SYNergy between PCI with TAXus and cardiac surgery
Introduction
Percutaneous coronary intervention (PCI) for unprotected left main (LM) coronary artery disease (CAD) has emerged as a viable alternative to coronary artery bypass grafting (CABG). The widespread introduction of drug-eluting stent (DES) technology1, advances in adjunctive antiplatelet therapy and intravascular imaging techniques, combined with improved technical expertise, provided the initial impetus for small non-randomised and observational studies that yielded preliminary evidence supporting LM PCI2-8. More recently, large non-randomised comparisons and multicentre randomised trials have demonstrated the safety and efficacy of LM revascularisation with DES compared to CAGB9-11. These trials and several pooled analyses12-14 have consistently observed similar hard endpoint clinical outcomes (death and myocardial infarction [MI]) for LM revascularisation with DES and CABG. The evolution of LM PCI has been reflected in recent societal guidelines from the European Society of Cardiology15 and the American Heart Association/American College of Cardiology16. These guidelines support the concept of LM intervention with DES as an alternative to CABG in patients at low risk for PCI-related procedural complications or with increased surgical risk.
Despite the encouraging nature of the data supporting LM revascularisation with DES, the long-term durability of these results requires confirmation. Reports of very late stent thrombosis17 and suggestions of reduced DES efficacy over time18 could moderate long-term outcomes of LM PCI with DES. To date, the available long-term data is limited by the heterogeneity of patient selection criteria, stents, and procedural strategies used in the various studies19-21.
The aim of this study was to evaluate the long-term outcomes of patients who underwent unprotected LM stenting using a single type of DES (TAXUS® Express®; Boston Scientific, Natick, MA, USA), and a single stenting technique for both ostial/shaft and distal bifurcation (provisional side branch [SB] stenting) lesions.
Methods
STUDY POPULATION
The design of the French Left Main TAXUS registry has been previously described7. In brief, 291 patients ≥18 years old presenting with stable or unstable angina and/or documented ischaemia, and ≥50% de novo unprotected LM stenosis were selected for PCI in four French centres between May 2003 and June 2005. The only exclusion criteria were presentation with either acute MI or cardiogenic shock, and contraindications to treatment with aspirin, clopidogrel or heparin. All patients provided written informed consent to study involvement.
PROCEDURES
Prior to study initiation, a uniform technical approach to LM intervention was adopted by the four study centres. The TAXUS® Express® stent was selected as the DES of choice as it was thought that this platform provided some potential advantages over the CYPHER™ stent (BX VELOCITY™ Cordis, Johnson & Johnson, Warren, NJ, USA): its availability in larger sizes (stent diameter up to 4 mm) and an “open-cell” design. Left main ostium and shaft lesions were treated with a single stent after meticulous imaging of the proximal LM segment, and particular attention to coverage of the LM ostium by the proximal stent edge. In all distal LM bifurcation lesions, the default strategy was provisional SB stenting, as previously described22. Side branch stenting was only performed in cases of residual SB stenosis ≥50% or in the presence of significant dissection after mandatory final kissing balloon inflation. If necessary, T-stenting was the recommended technique for stent implantation at the SB ostium. The use of intravascular ultrasound (IVUS) was left to the discretion of the physician.
Patients received a loading dose of clopidogrel 300 to 600 mg at least three hours before undergoing PCI. In addition, aspirin 250 to 500 mg was administered intravenously immediately before the procedure, even in patients who had been pretreated with oral aspirin. The use of glycoprotein (GP) IIb/IIIa inhibitors was at the investigators’ discretion.
A bolus of unfractionated heparin (70 IU/kg) was administered intravenously, followed by additional boluses as needed to reach and maintain an activated clotting time (ACT) of 300 seconds during the procedure. In patients treated with GP IIb/IIIa inhibitors, heparin was administered to maintain an ACT of 250 seconds. After the procedure, patients were treated with clopidogrel 75 mg (or 150 mg in patients weighing >80 kg) daily for at least six months and with aspirin ≥75 mg indefinitely.
STUDY DEFINITIONS
This five-year follow-up study focuses on the incidence of device-driven major adverse cardiovascular events (MACE), defined as the composite of cardiac death, MI, and ischaemia-driven target lesion revascularisation (TLR). All deaths that could not be clearly attributed to a non-cardiac cause were considered cardiac deaths. Q-wave MI was defined as the development of new pathological Q-waves. Non-Q-wave MI was defined as a typical rise and fall of creatine kinase-MB with at least one of the following: ischaemic symptoms, electrocardiographic changes indicative of ischaemia, or association with a coronary artery intervention. Diagnosis of either a spontaneous or periprocedural MI required the creatine kinase-MB to be ≥3 times the upper limit of normal. Stent thrombosis (ST) was defined, according to the Academic Research Consortium, as definite, probable, or possible23. Restenosis was defined as >50% angiographic narrowing of a previously successfully treated lesion and TLR was defined as any repeat percutaneous intervention or surgical bypass of the target lesion performed for >50% restenosis of the treated segment from 5 mm proximal to the stent and 5 mm distal to the stent. All outcomes were confirmed by source documentation from each participating site and were centrally adjudicated by an independent group of clinicians. Patients were followed up by clinical visit or telephonic interview at one month, six to eight months, one year, two years and five years.
The angiographic complexity of the coronary artery disease was defined using the SYNTAX (SYNergy between PCI with TAXus and cardiac surgery) score24, and was retrospectively calculated by two independent physicians. Patients were classified as low-, intermediate- and high-risk for adverse events based on SYNTAX scores of ≤22, 23-32, and ≥33, respectively. The EuroSCORE (European System for Cardiac Operative Risk Evaluation) was used to stratify the risk of death at 30 days25. Patients were stratified as high-risk in the presence of a logistic EuroSCORE of >6.
STATISTICAL ANALYSIS
The primary endpoint of this study was the incidence of MACE at five-year follow-up. Secondary endpoints include the cumulative incidence of all-cause death; cardiac death; MI; and the composite of death, MI and stroke. In the calculation of composite endpoints, events were counted only once, whichever occurred first. Continuous variables are presented as mean±standard deviation or median and range, and were compared with the Student’s t-test or Wilcoxon rank-sum test, according to distribution. Categorical variables are presented as numbers and percentages and were compared using the χ2 test or Fisher’s exact test. The rates of all-cause death, cardiac death, and MACE at five years were analysed by the Kaplan–Meier method. Differences between groups were analysed with the log-rank test. Independent predictors of five-year all-cause death, cardiac death and MACE were analysed using a Cox proportional hazards regression model. All variables that could plausibly be associated with MACE, had a p-value of <0.1 in the univariate analysis, and had an availability in the database >85%, were entered in the model. A probability value <0.05 was considered to indicate statistical significance. The analyses were performed with Stata version 10 (StataCorp, College Station, TX, USA). All authors had full access to the data and take full responsibility for its integrity.
Results
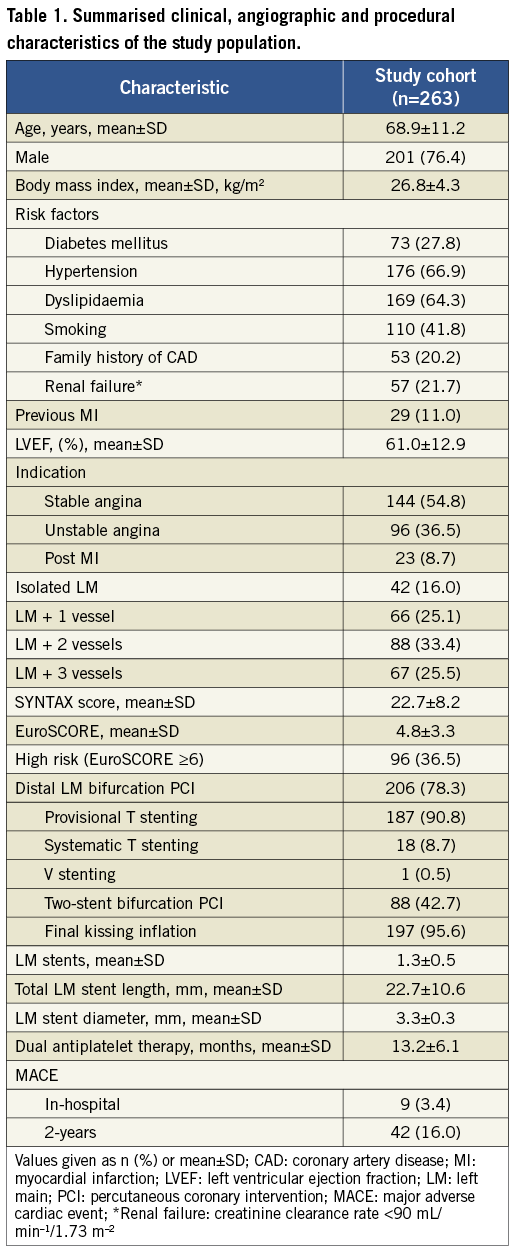
PATIENT CHARACTERISTICS AND PROCEDURAL RESULTS
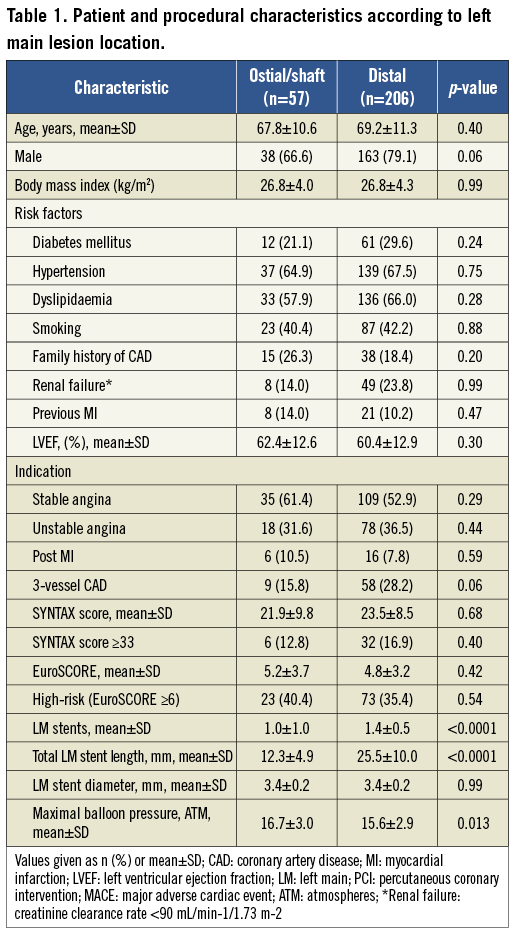
Clinical follow-up was available in 263 (90.4%) of the patients prospectively included in this study, at a mean duration of 62±14 months (Figure 1). The baseline, clinical, lesion, and procedural characteristics of the study patients have been previously described, and are summarised in Table 17. In brief, the mean age at the time of PCI was 68.9±11.2 years, 27.8% were diabetic, 21.7% had renal failure, 25.5% had 3-vessel coronary artery disease (CAD), 78.3% had distal LM disease, and 16.1% had a SYNTAX score ≥33. In cases of distal LM intervention (n=206), the provisional SB stenting technique was performed in 90.8%, SB stent implantation was required in 43% of cases, and final kissing balloon inflation was performed in 95.6%. In total, 78.4% of patients underwent non-LM revascularisation during the index PCI, and the mean number of non-LM vessels treated per patient was 1.34±0.93. The in-hospital outcomes were as follows: MACE 3.4%, cardiac death 0.4%, non–Q-wave MI 3.0%, TLR 0.4%.
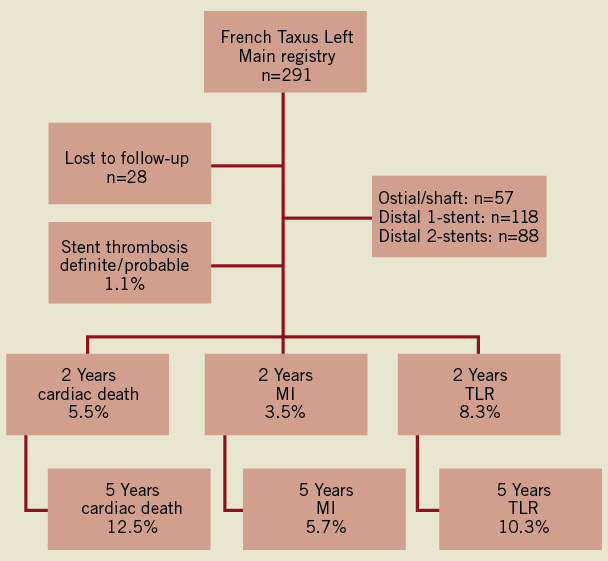
Figure 1. Schematic representation of the study population and cumulative incidence of adverse events at 2 and 5 years. MI: myocardial infarction; TLR: target lesion revascularisation
CLINICAL OUTCOMES AT FIVE YEARS
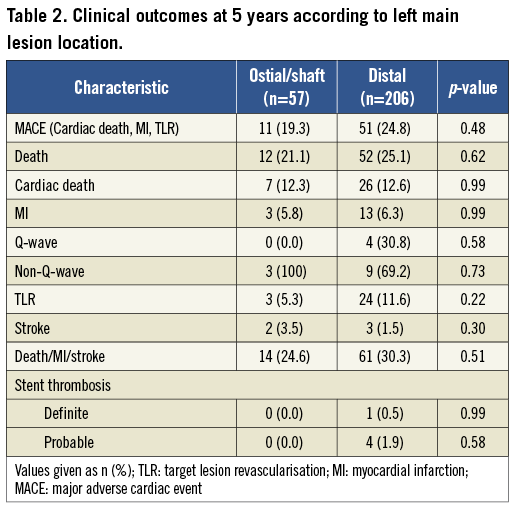
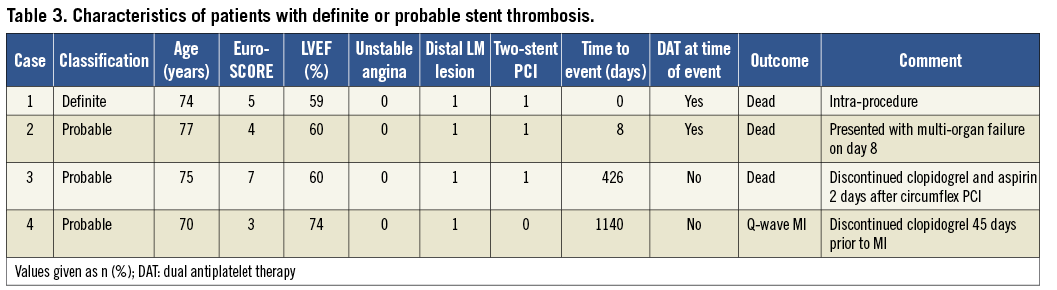
The cumulative incidence of MACE, the primary endpoint of the study, was 23.6% after five-year follow-up (Table 2). The crude rates of all-cause death and cardiac death at five years were 24.3% and 12.5%, respectively. Cardiac deaths were due to: MI (n=8), pulmonary oedema (n=5), and congestive heart failure (n=2). In 18 cases, a death of unknown aetiology was counted as a cardiac death as per the protocol. During follow-up, MI occurred in 16 patients (6.1%): four Q-wave and 12 non-Q-wave. The cumulative incidence of definite ST at five years was 0.4% (Table 3). The only case of definite ST was fatal and occurred during the index PCI. Three cases of probable ST occurred at eight, 426 and 1,140 days, and possible ST occurred in 6.5%. The composite of death/MI/stroke occurred in 28.5%. The incidence of ischaemia-driven TLR was 10.3% at five years, and revascularisation was primarily by repeat PCI (74.1%) rather than CABG (25.9%). Target vessel revascularisation was required in 12.9%, and further non-LM revascularisation was performed in 18.6%. Any type of revascularisation was required in 24.3% and stroke occurred in 1.9% during follow-up. The rate of MACE up to two years was 7.9% per year, but decreased to 2.4% per year between years two to five (Figure 2).
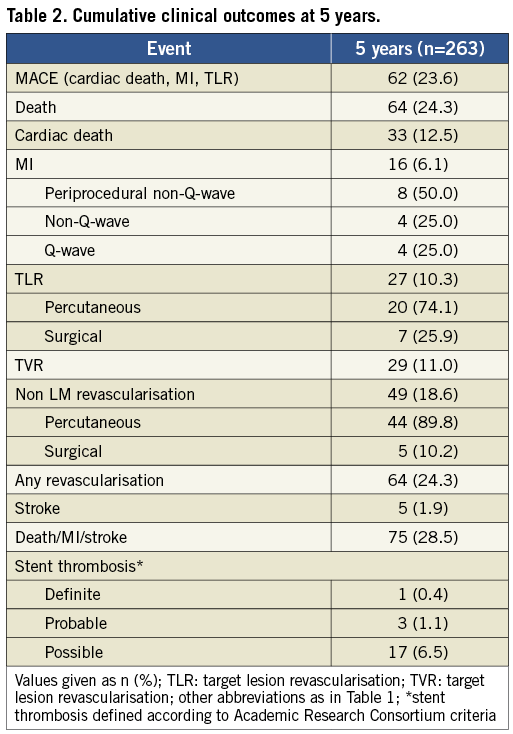
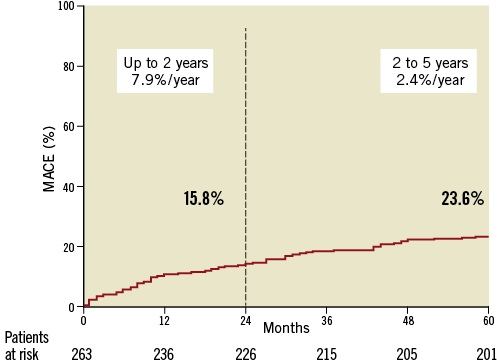
Figure 2. Incidence of MACE following unprotected left main PCI up to 2 years, and between 2 and 5 years of follow-up.
CLINICAL OUTCOMES ACCORDING TO LEFT MAIN LESION LOCATION
Of the 263 patients who underwent LM intervention, 57 (21.7%) had ostial/shaft lesions and 206 (78.3%) had distal lesions (Online Table 1). Patients with ostial/shaft lesions had shorter total stent lengths and higher maximal balloon inflation pressures than patients with distal bifurcation stenoses. There was no difference in the cumulative incidence of MACE, death, cardiac death or MI between patients with ostial/shaft lesions and those with bifurcation stenosis (Figure 3). Although not statistically different, the incidence of TLR in distal lesions was numerically increased compared to that observed in ostial/shaft lesions (11.6% versus 5.3%; p=0.22) (Online Table 2).
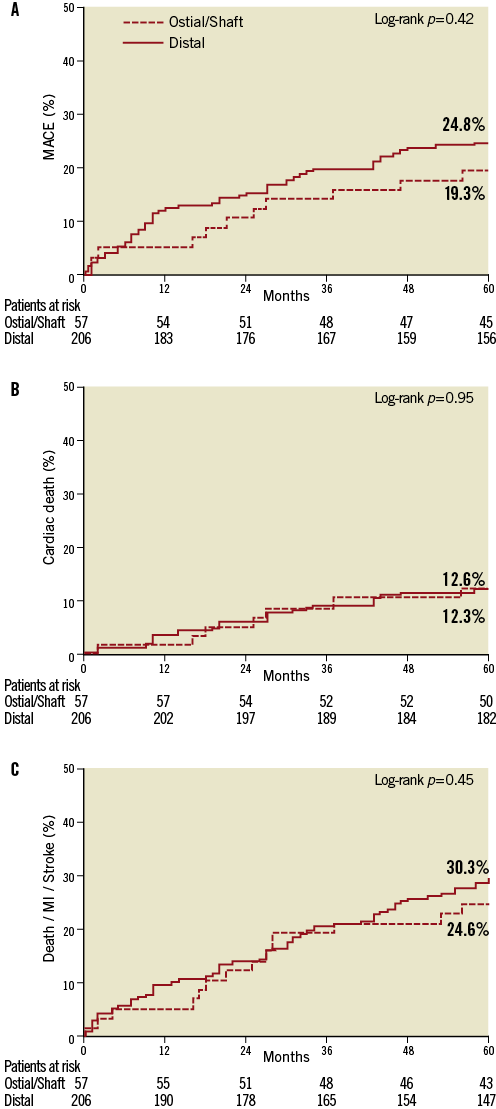
Figure 3. Kaplan–Meier incidence curves of: A) MACE; (B) cardiac death; and (C) cardiac death, MI and stroke in patients with ostial/shaft or distal LM lesions.
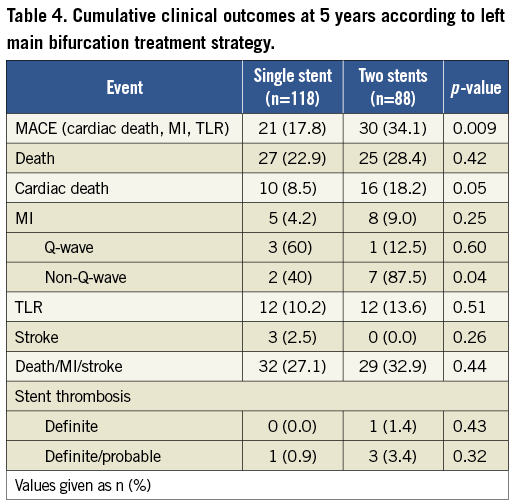
CLINICAL OUTCOMES ACCORDING TO LEFT MAIN BIFURCATION TREATMENT STRATEGY
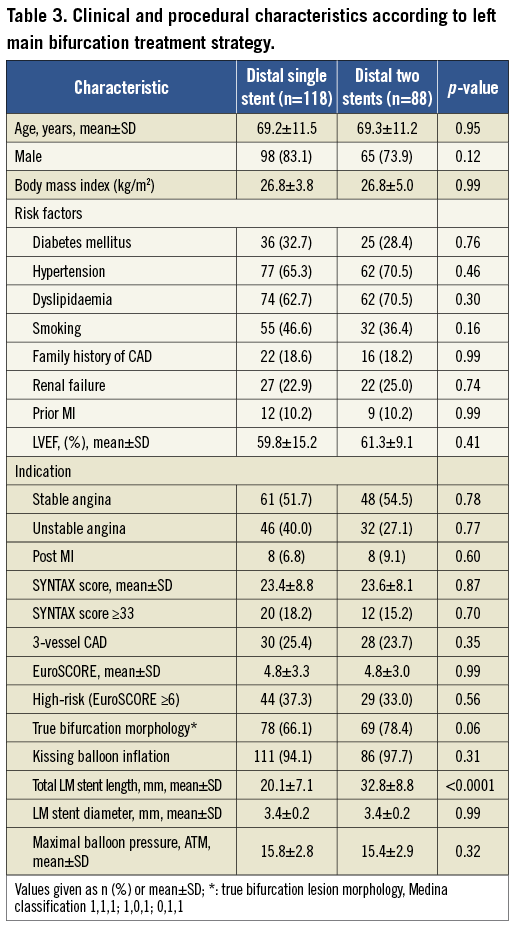
Among the 206 patients with distal LM bifurcation lesions, 118 (57.3%) underwent single-stent PCI and 88 (42.7%) benefited from a two-stent strategy (Online Table 3). Of the patients with the more complex interventions, a two-stent strategy was planned prospectively in 19 (21.6%) cases and was a bailout following provisional SB stenting in 69 (78.4%) cases. In patients requiring two stents there was a trend towards a higher incidence of true bifurcation morphology (78.4% versus 66.1%; p=0.06), and a significantly higher rate of MACE at five years was observed in these patients compared to those who underwent single-stent PCI (34.1% versus 17.8%; p=0.009) (Figure 4). This was primarily driven by an increased incidence of cardiac death (18.2% versus 8.5%; p=0.05) and non-Q-wave MI (8.0% versus 1.7%; p=0.04) in the two-stent cohort (Table 4). There was no significant difference in the rate of TLR between two-stent and single-stent strategies after five years (13.6% versus 10.2%; p=0.51).
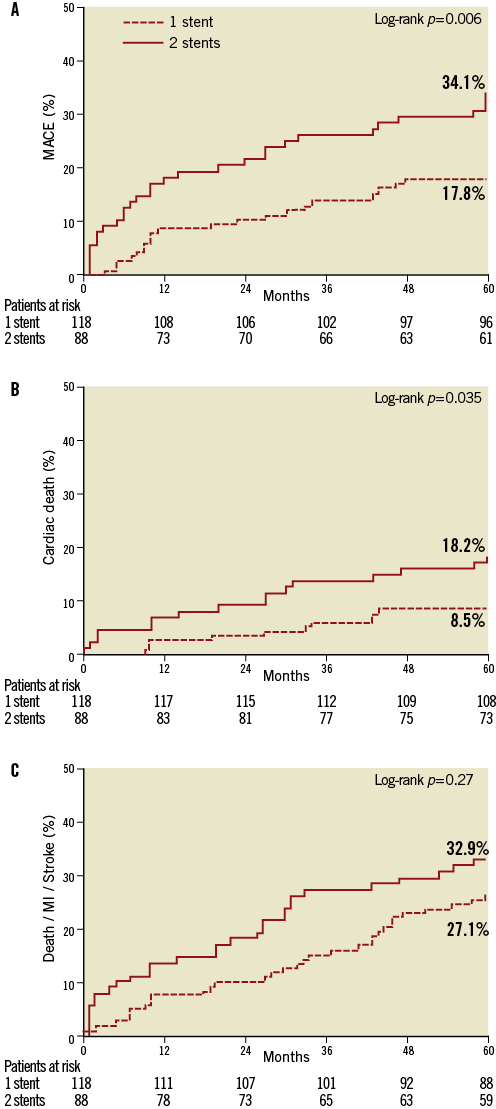
Figure 4. Kaplan–Meier incidence curves of: A) MACE; (B) cardiac death; and (C) cardiac death, MI or stroke in patients with distal LM lesions treated with single- or two-stent procedures.
OUTCOMES ACCORDING TO DIABETES STATUS
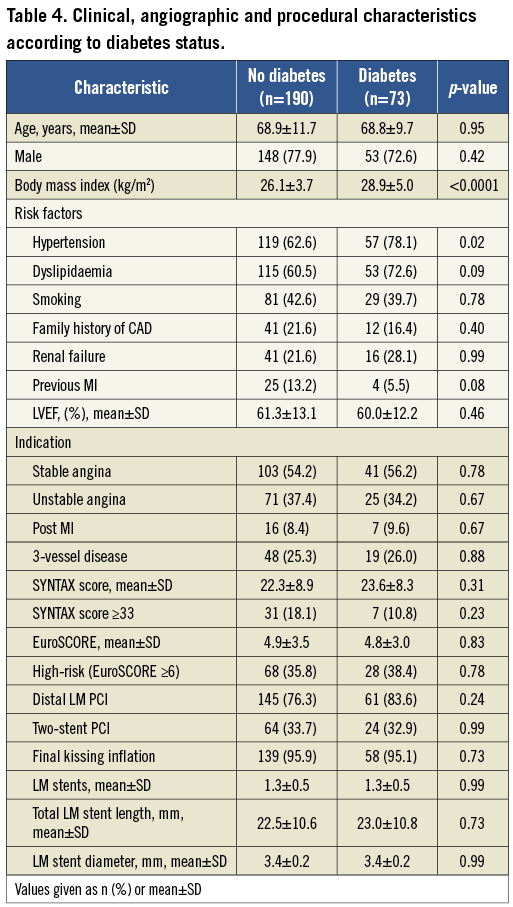
Clinical outcomes were compared between the subgroup of patients with diabetes mellitus (n=73) and non-diabetic patients (n=190) (Online Table 4). At five years, the cumulative incidence of MACE was significantly higher in diabetic patients compared to non-diabetic subjects (32.9% versus 20.0%; p=0.03) (Figure 5). This difference was primarily driven by an increase in TLR in diabetic patients (19.2% versus 6.8%; p=0.005), although the rate of cardiac death (15.1% versus 11.6%; p=0.53), definite/probable stent thrombosis (4.2% versus 0.5%; p=0.06), and the composite endpoint of death, MI or stroke (37.0% versus 25.3%; p=0.07) tended to be higher in the diabetic cohort (Table 5).
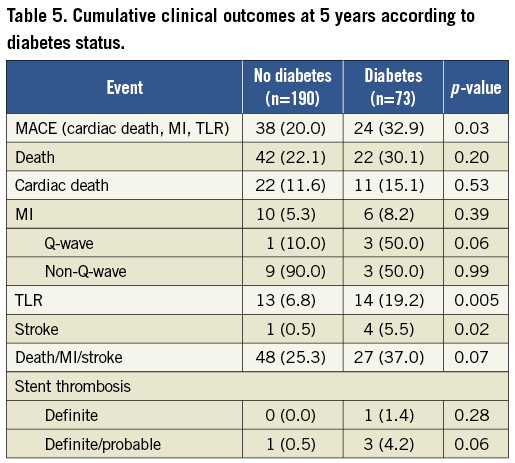
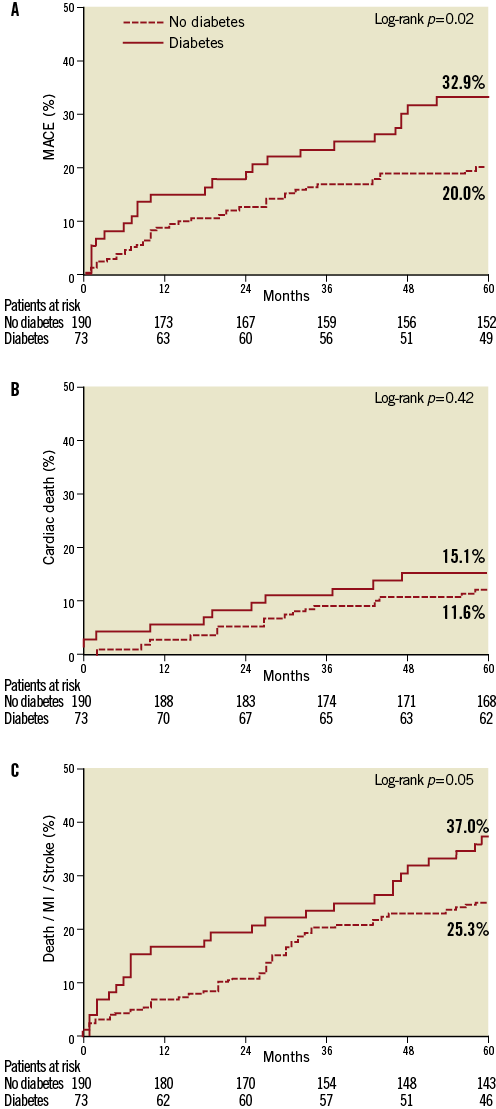
Figure 5. Kaplan–Meier incidence curves of: A) MACE; (B) cardiac death; and (C) cardiac death, MI or stroke in patients with diabetes mellitus and those without.
OUTCOMES ACCORDING TO SYNTAX SCORE AND EUROSCORE
Baseline SYNTAX scores were calculated retrospectively in all cases and patients were subdivided according to disease complexity: low (≤22), intermediate (23 to 32), and high (≥33) (Table 6). The incidence of MACE at five years was not significantly different between these groups (Figure 6). Both all-cause death (44.7% versus 26.8% versus 17.6%; p=0.002) and the composite of death, MI or stroke (47.4% versus 31.7% versus 21.7%; p=0.006) were increased in patients with SYNTAX scores ≥33 compared to those with lower scores. There was a trend towards increased cardiac death in those with higher SYNTAX scores (21.1% versus 15.9% versus 8.5%; p=0.06).
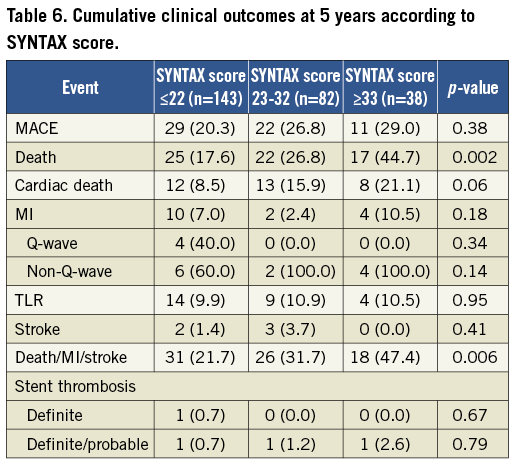
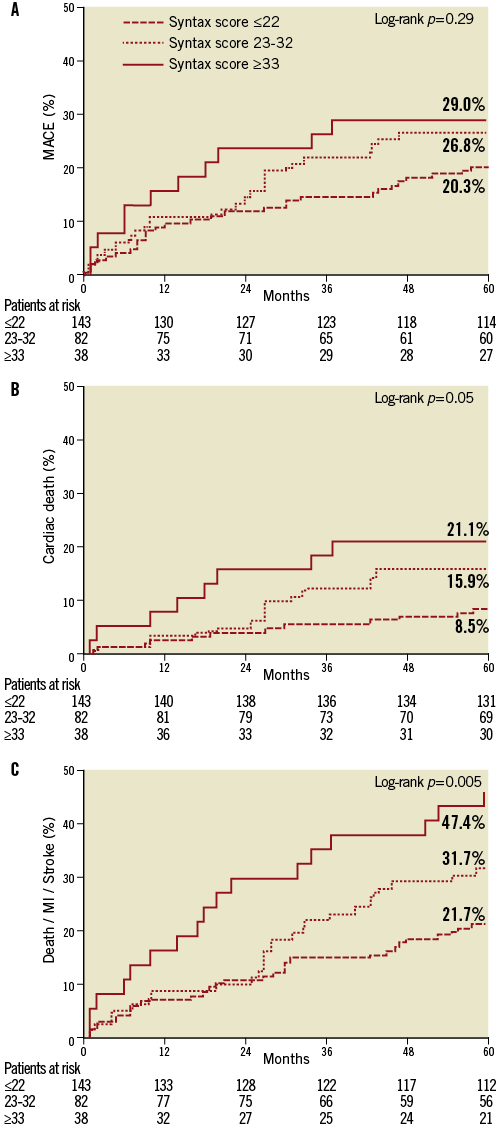
Figure 6. Kaplan–Meier incidence curves of: A) MACE; (B) cardiac death; and (C) cardiac death, MI or stroke according to baseline SYNTAX score.
High-risk patients with a baseline EuroSCORE of ≥6 had increased rates of cardiac death (22.9% versus 6.6%; p=0.0002), all-cause death (44.8% versus 12.6%; p<0.0001), and the composite of death, MI or stroke (49.0% versus 16.8%; p<0.0001) compared to those with a EuroSCORE of <6.
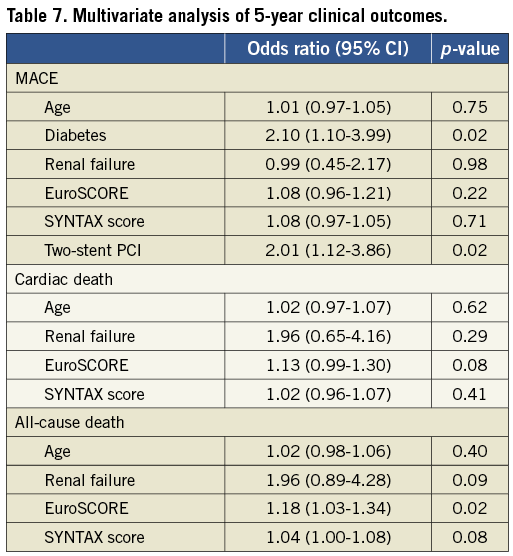
MULTIVARIATE ANALYSIS OF FIVE-YEAR CLINICAL OUTCOMES
In the multivariable Cox regression analysis, diabetes mellitus (OR 2.10, 95% CI 1.10-3.99, p=0.02)] and the presence of two stents in the distal LM (OR 2.01, 95% CI 1.12-3.86, p=0.02) were associated with MACE at five years (Table 7). Only the EuroSCORE (OR 1.18, CI 1.03-1.34, p=0.02) was associated with all-cause death at five years.
Discussion
This study presents the five-year follow-up of a large series of patients with unprotected LM stenosis treated with a single DES, using a common PCI strategy. The main findings of the present study are: 1) unprotected LM stenting with paclitaxel-eluting stents is associated with acceptable long-term safety and efficacy; (2) the risk of late and very late ST in LM intervention is low; (3) subgroup analyses suggest that both the necessity to use a second stent for distal LM interventions and diabetes mellitus are associated with an increased rate of MACE at five years.
Aortocoronary bypass grafting has been the dominant strategy for treating obstructive LM CAD for decades. Historical comparisons between surgical and bare metal stent revascularisation suggested that patients had better outcomes with CABG26. More recently, large observational studies, pooled analyses and randomised trials have shown similar medium-term outcomes between DES and surgical revascularisation for LM disease2-14. However, data supporting the long-term safety and efficacy of LM intervention with DES are relatively sparse.
To date, three studies have reported long-term follow-up from comparative analyses of LM revascularisation with DES or surgery19-21. In the MAIN-COMPARE (Revascularization for Unprotected Left Main Coronary Artery Stenosis: Comparison of Percutaneous Coronary Angioplasty Versus Surgical Revascularization) registry, LM revascularisation with mixed type DES (n=784) yielded five-year mortality and TVR rates of 12.1% and 15.7%, respectively21. Outcomes from the mixed DES cohort of the ASAN-MAIN (ASAN Medical Center-Left MAIN Revascularization) registry (n=176) were somewhat better, with five-year mortality of 5.9%, of which 3.7% was deemed of cardiac origin. In this analysis, the rates of MI and TLR were 15.7% and 13.2%, respectively19. Finally, the Milan experience (n=107) observed five-year all-cause and cardiac mortality rates of 15.9% and 7.5%, respectively, and the five-year incidences of TLR and MI were 18.7% and 0.9%20.
Compared to these studies, all-cause death (24.3%) and cardiac mortality (12.5%) in the current study are greater. These seemingly disparate results are likely due to different endpoint definitions and considerable differences in the baseline risk of patients recruited. The mean EuroSCORE in the current study (4.8±3.3) was considerably higher than that in either the ASAN-MAIN (3.3±2.7) or Milan experience (4.4±3.6). Similarly, the mean age in the current study (68.9±11.2) was far greater than the MAIN-COMPARE (62.5±11.1), ASAN-MAIN (61.1±11.1), and the Milan experience (63.6±10.3). Both of these factors have been associated with adverse patient outcomes27. Furthermore, long-term follow-up studies tend to overestimate cardiac mortality as natural history and non-procedural events that arise during follow-up can be incorrectly categorised as MACE in the absence of definitive evidence. Over half (54.5%) of the cardiac deaths in the current study were deaths of uncertain aetiology.
Reassuringly, the rates of stent thrombosis observed in the current study are low (0.4%): only one patient had definite ST (intra-procedure), and three patients had probable stent thrombosis. Low rates of LM definite/probable stent thrombosis have previously been reported in registries of LM PCI with long-term follow-up: MAIN-COMPARE (1.5%), ASAN-MAIN (1.8%) and the Milan experience (0.93%)19-21. Further reductions in stent thrombosis and MACE could perhaps be achieved by avoiding certain bifurcation stenting techniques28, using polymer-free DES29, and systematic use of intravascular ultrasound30.
The necessity for repeat revascularisation following LM intervention with DES has been consistently reported to be higher than that for CABG10,11,21. However, the rate of TLR following LM stenting with DES is dependent on patient31 and lesion32 characteristics, and the stenting technique employed33. Not surprisingly therefore, the reported incidence of TLR at five years following LM intervention with mixed DES varies considerably (9.7-18.7%)20,21. In contrast to the mortality data, the rate of TLR (10.3%) in the current study was considerably lower than those described in other long-term studies19-21, and may reflect the per-protocol use of the provisional SB stenting technique. This technique has been associated with less MACE and SB restenosis compared to more complex strategies33,34. Of interest, and perhaps consistent with this hypothesis, is the fact that requirement for any revascularisation during the five years of follow-up (24.3%) in the current study is consistent with the level of repeat PCI (23.0%) observed in the four-year results from the SYNTAX trial35. Thus, although the rate of LM TLR is low, the level of non-LM revascularisation reflects the complexity of this patient population. The absence of mandatory repeat coronary angiography in the current study could also have contributed to a lower rate of TLR compared to other studies with frequent follow-up angiography: MAIN-COMPARE (73.0%) and ASAN-MAIN (76.0%)36.
In non-LM interventions, single- and two-stent PCI strategies have similar safety endpoints34. In contrast, the stenting technique is an important factor in determining outcomes in LM interventions. Although observations derived from subgroup analysis should be interpreted with caution and the interpretation must be speculative, our observation of an increased risk of hard endpoint adverse events (cardiac death, non-Q-wave MI) in patients requiring two-stent procedures for distal LM PCI is consistent with previous data33. In our study, these patients tended to have more complex LM anatomy and were therefore at increased risk of clinical events; however it is possible that the presence of a second stent in the LM may in itself increase the risk of MACE. In keeping with our observations, an analysis of 773 patients treated with DES for unprotected LM stenosis, reported significantly lower cardiac mortality and MI in patients treated with one stent compared to those treated with two stents (hazard ratio: 0.38, 95% CI 0.17 to 0.85, p=0.02)33. While several factors influence the decision to undertake a particular stenting strategy for distal LM lesions, we believe that every effort should be made to avoid SB complications and the necessity for SB stenting when using a provisional SB strategy in the LM. Several new techniques, such as the use of non-compliant balloons for kissing balloon post-dilatation and performing a proximal optimisation technique may reduce the risk of SB stenting37,38.
Patients with diabetes mellitus are characterised by accelerated atherosclerosis, active inflammation, and increased complexity of coronary artery disease compared to non-diabetic subjects. In the present study, patients with diabetes mellitus had a significantly increased cumulative incidence of MACE five years after LM stenting compared to non-diabetic subjects. This result was driven by an increased rate of TLR in diabetic patients, but there was also a trend towards increased cardiac death, MI, and definite/probable stent thrombosis in the diabetic cohort. Similarly, subgroup analysis of the 452 diabetic patients included in the SYNTAX trial demonstrated increased cardiac mortality in diabetic patients compared to non-diabetic subjects31. Interestingly, the increase in MACE observed in diabetic patients was largely observed after four years of follow-up, indicating that very late events continue to occur in this patient population.
The decision to proceed with either percutaneous or surgical LM revascularisation depends on a variety of clinical and anatomical factors, and should always be made following consultation with the patient, an interventional cardiologist and a cardiac surgeon. It is clear that in patients with LM and extensive multivessel disease, CABG is the treatment of choice, however PCI with DES is a real alternative for patients with less diffuse CAD. The results of the ongoing randomised EXCEL (Evaluation of XIENCE PRIME™ Everolimus Eluting Stent System [EECSS] or XIENCE V® EECSS Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization) trial will add considerably to our current understanding of LM intervention and are eagerly awaited.
Limitations
The major limitation of this study is that there is no surgical control group for comparison. However, given the initial exploratory nature of this prospective study, it was not feasible to perform a comparative efficacy analysis at the time of conception. The study population is also of limited size, however the use of a single stent and single stenting technique for bifurcation lesions add strength to the design. Furthermore, the interpretation of anatomic and clinical subgroup analyses should be considered hypothetical and hypotheses generating only. Finally, application of our results may not extend to second generation DES.
Conclusion
This study confirms the long-term durability of unprotected LM revascularisation with paclitaxel-eluting stents. Diabetes mellitus and the necessity to implant a second stent in the SB of the distal LM during a provisional SB stenting technique are associated with an increased risk of adverse events at five years.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Online Table 1. Patient and procedural characteristics according to left main lesion location.
Online Table 2. Clinical outcomes at 5 years according to left main lesion location.
Online Table 3. Clinical and procedural characteristics according to left main bifurcation treatment strategy.
Online Table 4. Clinical, angiographic and procedural characteristics according to diabetes status.