Abstract
Aims: With newer drug-eluting stents (DES), PCI has appeared as an acceptable alternative to cardiac surgery in the treatment of unprotected left main (ULM) lesions. Using data from the French Left Main Taxus and the LEft MAin Xience registries, we compared two-year outcomes in consecutive patients from 2003-2008 using everolimus-eluting stents (EES) vs. paclitaxel-eluting stents (PES).
Methods and results: We performed a matched comparison according to SYNTAX score, distal LM stenosis, provisional side-branch T-stenting and single stent use, focusing on the primary endpoints of target vessel MI (TVMI) and target vessel failure (TVF). After propensity score matching, there were 172 patients in each group. There was no difference in gender (76.5% male), age (69.5±11.3 years), diabetes (26.2% vs. 24.4%, p=0.71), NSTEMI (40.7% vs. 40.7%, p=1), or LVEF <40% (11.0% vs. 6.7%, p=0.22). Patients with distal LM lesions (75.9%) were treated using provisional T-stenting in 91.1%. The side branch was stented in 22% of all patients (p=0.51). Cumulative two-year events showed significant differences in TVMI (9.9% vs. 4.1%, p=0.04) and TVF (16.3% vs. 7.6%, p=0.01) for PES and EES, respectively.
Conclusions: ULM stenting with EES is safer and more effective than PES with a reduction in TLF by 53% at two years.
Introduction
Despite long-standing opinions that the most appropriate strategy for the treatment of unprotected left main (LM) lesions is coronary artery bypass grafting (CABG)1,2, data are now beginning to emerge from large registries and randomised trials suggesting that PCI is a viable alternative in certain patients. Many studies have shown that PCI is possible in the distal LM, and produces comparable mid and long-term results using first-generation DES3-6. Studies, registries5-8 and a recent meta-analysis9 have compared patients with LM lesions revascularised with PCI versus CABG showing similar outcomes in terms of death, stroke and myocardial infarction; however, the need for repeat revascularisation remains consistently higher in the PCI group. Following this, the ACC/AHA and the ESC updated their recommendations so that PCI may be considered as an alternative to surgery in certain patients10,11. The SYNTAX (SYNergy between PCI with TAXus and Cardiac Surgery) trial recommended CABG as a preferable option to PCI in patients with a SYNTAX score >32, but the study was not powered to address patients with LM disease. An interesting theory hypothesises that the use of a more effective stent might have altered the findings of the study12.
Although the results of PCI using DES in LM disease appear promising, there remains the issue of an increased need for re-intervention in these complex lesions. Second-generation DES were designed to improve safety, efficacy and stent performance; however, there remains the question of which stent to use and whether all stents are equal in LM revascularisation. There is currently limited data reporting the superiority of second-generation DES over first-generation stents4,13-16, but there is sparse data on the use of second-generation DES in the ULM, and the optimal strategy for LMS disease remains uncertain. We wished to compare the outcomes of this new second-generation stent against the TAXUS first-generation stent in patients undergoing ULM stenting.
We compared two large registries using the paclitaxel (PES) and the everolimus (EES) DES using identical strategies, to assess the efficacy and safety of the TAXUS™ Express2™ (Boston Scientific, Boston, MA, USA) and the XIENCE V® (Abbott Vascular, Santa Clara, CA, USA) DES in a real-world population with LM stenosis.
Methods
Between March 2003 and July 2005, 291 patients undergoing LM stenting with PES were entered prospectively into the French Left Main Taxus (FLM Taxus) registry. From December 2007 to May 20093, 173 patients undergoing LM stenting with EES were entered prospectively into the LEft MAin Xience (LEMAX) registry17. We performed a propensity score matching comparison of the two registries in order to avoid confounding factors attributable to different: 1) SYNTAX scores, 2) rate of stenosis involving the distal LM, 3) provisional side-branch T-stenting strategies, and 4) the use of one or two stents in the distal LM and to compare the two-year outcomes after EES vs. PES for LM lesions. One patient was lost to follow-up in the LEMAX registry; therefore 172 patients with two-year follow-up were matched to 172 patients in the FLM registry.
STUDY POPULATION
Inclusion criteria were the presence of stable or unstable angina and/or documented ischaemia and angiographic evidence of a significant coronary lesion including de novo LM >50% diameter stenosis by quantitative coronary analysis (QCA), considered amenable to PCI. The LM was considered to be unprotected in the absence of any patent coronary artery bypass grafts to either the left anterior descending artery or the left circumflex artery. Exclusion criteria were ST-elevation myocardial infarction, cardiogenic shock and patients with a contraindication to prolonged dual antiplatelet therapy.
The study was conducted in accordance with the Declaration of Helsinki and was approved by each institutional review committee. Patients provided written informed consent.
PROCEDURE
Patients were preloaded with clopidogrel (300-600 mg) at least three hours before the procedure. Unfractionated heparin (with a target activated clotting time ≥300 secs) was administered during the procedure. Glycoprotein IIb/IIIa inhibitors were given at the operator’s discretion. Following the intervention, patients were advised to take aspirin ≥75 mg daily indefinitely and clopidogrel 75 mg daily (or 150 mg daily if their weight was greater than 80 kg) for at least six months in the PES group and 12 months in the EES group.
All operators used the same technical approach. In distal LM lesions, the preferred strategy was provisional side-branch T-stenting. T-stenting was recommended for stent implantation in the side branch if deemed necessary (TIMI flow <3 and/or residual stenosis >50%). Coverage of the ostium of the left main was advised in order to avoid proximal edge restenosis. Intravascular ultrasound (IVUS) and intra-aortic balloon pump were used at the discretion of the operator.
Treatment of additional lesions during the same procedure was allowed. The number of extra LM lesions revascularised and the type of stent used were at the operator’s discretion. Staged procedures were permitted.
QUANTITATIVE CORONARY ANALYSIS
All coronary angiograms were analysed with a semi-automated edge-contour-detection computer analysis system (QAngio XA version 7.1; Medis, Leiden, The Netherlands) at baseline and at the end of the procedure. Analysis was performed by an independent core laboratory (European Cardiovascular Research Centre, CERC, Massy, France). The baseline diagnostic angiograms were reviewed by two experienced interventional cardiologists who were blinded to other clinical data, and who scored angiograms according to the SYNTAX score algorithm18.
ENDPOINT DEFINITIONS AND FOLLOW-UP
The primary endpoint at two-year follow-up was target lesion failure (TLF), defined as the composite of cardiac death, target vessel MI, and clinically driven TLR. Definitions of clinical events have been previously described7,19. The LEMAX registry was monitored by CERC and events were adjudicated by an independent clinical events committee at one and two years. The FLM Taxus registry was not monitored and follow-up was by telephone at two years. Stent thrombosis (ST) was defined, according to the Academic Research Consortium definitions, as definite, probable or possible19. Cases adjudicated as possible were also further sub-classified as either: 1) sudden cardiac death or acute ischaemia likely; or 2) unexplained death, acute ischaemia unlikely (Table 1). A new category termed “ARC modified possible” included only those cases classified as sudden death or acute ischaemia likely20. Deaths were classified as either cardiac or non-cardiac. Death due to unknown causes was adjudicated as cardiac.
STATISTICAL ANALYSIS
Statistical analysis was performed using STATA 10.1 (StataCorp LP, College Station, TX, USA). Baseline descriptive statistics are presented as frequencies and percentages for categorical variables and mean±SD or median (interquartile range) for continuous variables. The normality of data was assessed using the skewness and kurtosis normality test. The differences between the groups were assessed with the chi-square test or Fisher’s exact test for categorical data and Student’s t-test for continuous data. Survival analysis was performed by applying the Kaplan-Meier method. Differences in survival parameters were assessed for significance, and relative risks were calculated by means of the log-rank test.
Patients were also analysed post hoc by baseline SYNTAX score tertile (low <22, intermediate 23 to 32, and high >33) for two-year TLF outcomes. Differences between groups were considered statistically significant if the 95% confidence interval (CI) around the difference of the means did not contain zero. In a prespecified analysis, baseline predictors for two-year TLF were identified using multivariate logistic analysis including variables showing a p-value <0.10 in association with two-year TLF by univariate analysis.
Logistic regression was used to generate a model to calculate propensity scores. The reliability of the model was evaluated using the Hosmer-Lemeshow goodness-of-fit statistical and residual analyses. Each patient treated by EES was matched with a PES patient using the closest propensity score. Patient and procedural variables were used to calculate the propensity score.
Results
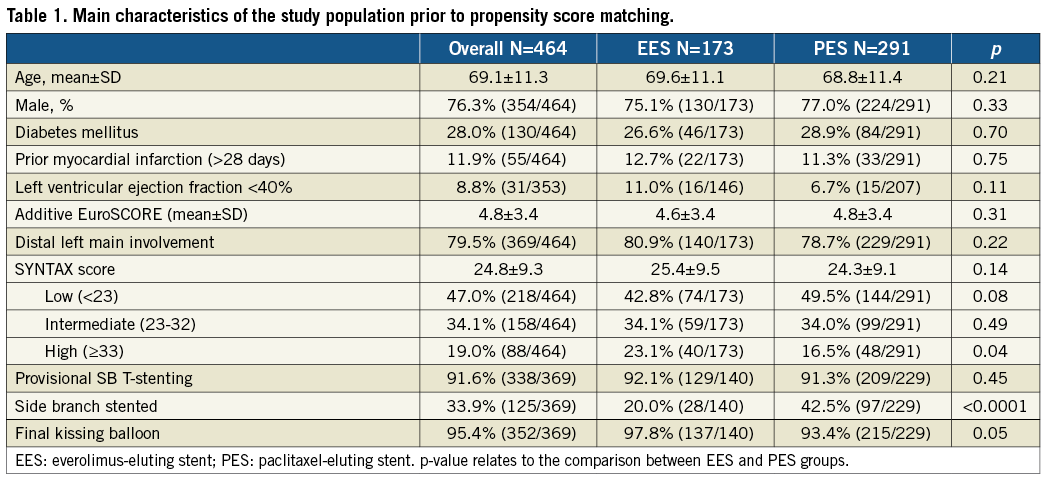
Baseline characteristics of the population are listed in Table 1. Before propensity score matching, patients treated by PES had more favourable angiographic characteristics with lower rates (p=0.04) of high SYNTAX score (>32) compared to patients treated with an EES (16.5% vs. 23.1%, respectively). In these patients, the side branch of the left main stem was more frequently (p<0.0001) treated with an additional stent, compared to those treated with an EES (42.5% vs. 20%) and there was a trend (p=0.05) towards a lower rate of final kissing balloon angioplasty (93.4% vs. 97.8%, respectively).
After propensity score matching, there were 172 patients in each group. The baseline, clinical, lesion and procedural characteristics are summarised in Table 2 and Table 3. Quantitative coronary angiography measurements are reported in Table 3.
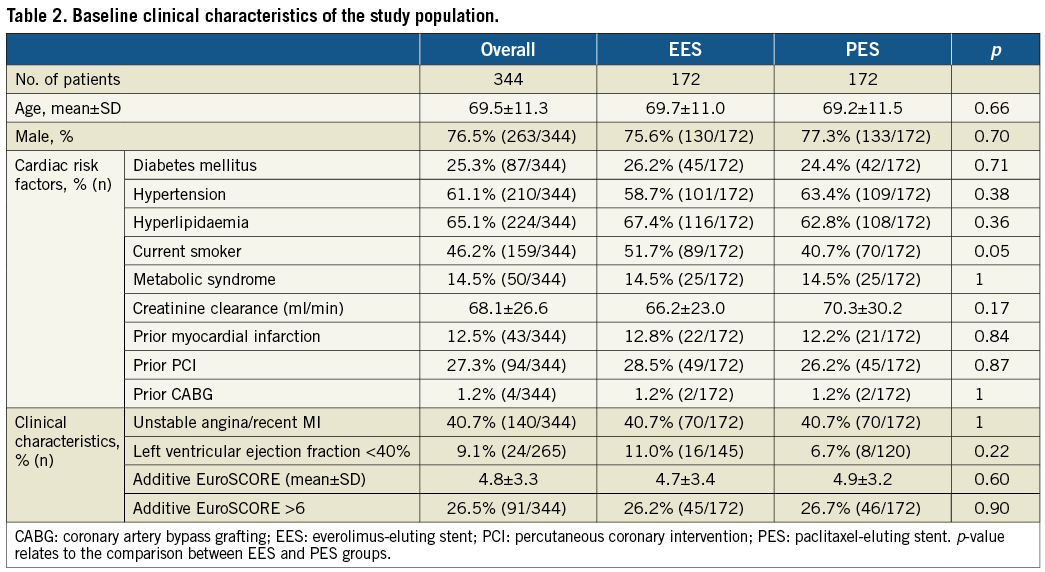
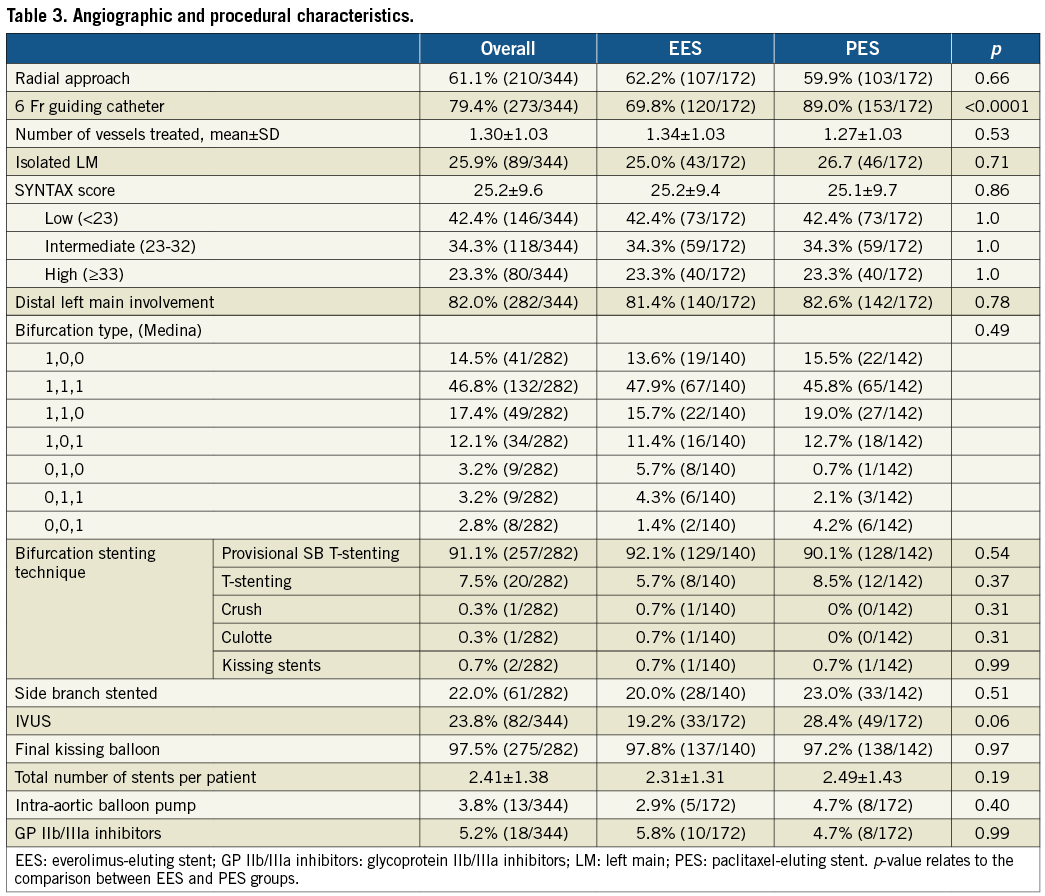
Patients were aged 69.5±11.3 years with 76.5% of patients being male. Diabetes was present in 25.3% of patients and 27.3% had undergone previous PCI. The mean SYNTAX score was 25.5±9.6 with similar distributions between both groups. The distal LM was involved in 82.0%, provisional side-branch T-stenting was performed in 91.1%, with a side-branch stenting rate of 22% in all patients, and final kissing balloons were performed in 97.5%.
QUANTITATIVE CORONARY ANALYSIS
As shown in Table 4, the preprocedural measurements were similar in both groups. Post-procedurally, the LM reference diameter was significantly higher in the EES group (4.02±0.44 vs. 3.80±0.44, p<0.0001).
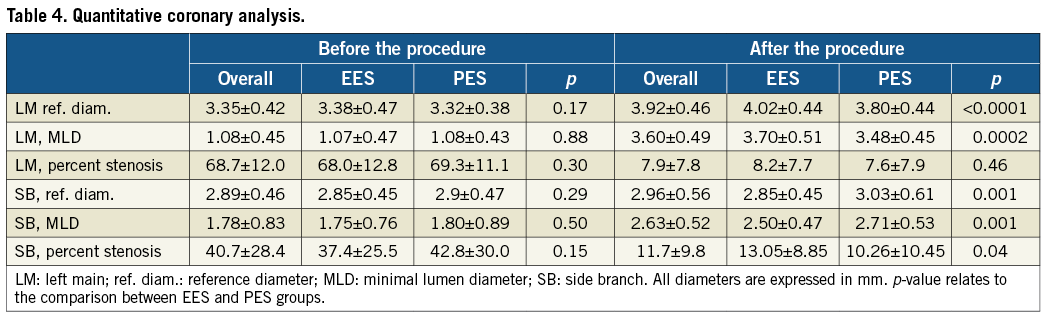
There was a notable, though non-significant difference in the use of IVUS between the two groups. IVUS was used in 28.4% of patients in the PES group and 19.2% in the EES group (p=0.06). IVUS was used more frequently in the early days of LMS PCI and, as operator experience increased, the use of IVUS was seen to decrease. We feel that this difference in IVUS use does not explain the difference in the post-procedural QCA measurements.
TWO-YEAR OUTCOMES
Clinical follow-up at two years was completed in all patients. Outcomes are described in Table 5 and Figure 1. At two-year follow-up, TLF rates were significantly higher in the PES than in the EES group (16.3% vs. 7.6%; ∆–8.7%; p=0.01; Figure 1D). There were further significant differences between PES and EES in terms of TVMI (9.9% vs. 4.1%; ∆–5.8%; p=0.04; Figure 1B) and definite, probable or possible ST (7.0% vs. 1.7%, p=0.02; Figure 1E) for PES and EES, respectively. There was a strong trend towards increased cardiac death in the PES group (6.4% vs. 2.3%; ∆–4.1%; p=0.06; Figure 1A). There was no difference between the stents for the outcome of clinically indicated TLR.
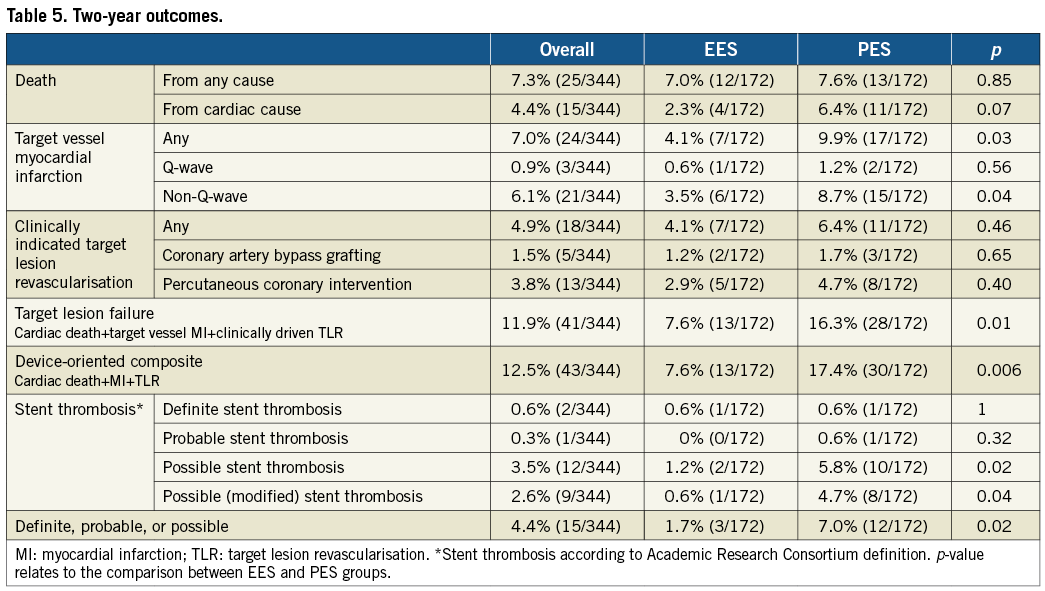
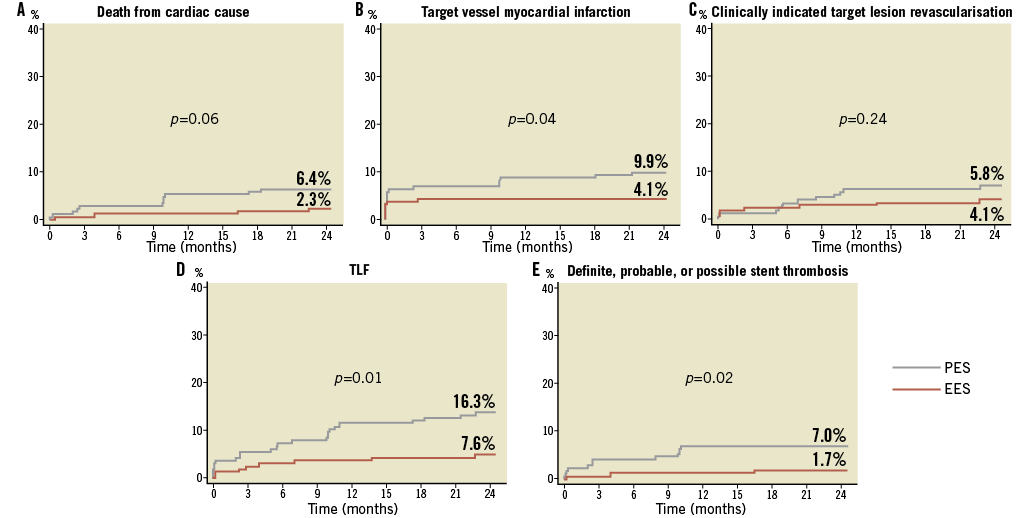
Figure 1. Kaplan-Meier estimates of cardiac death, target vessel myocardial infarction, clinically indicated TLR, TLF and definite, probable, or possible ST for patients treated by PES vs. EES for ULM disease. p-values from log-rank tests.
OUTCOMES STRATIFIED BY BASELINE SYNTAX SCORE
Patients were stratified according to the three SYNTAX score subgroups described in the SYNTAX trial7 (Figure 2). Patients with low and intermediate SYNTAX scores had similar TLF outcomes at two years. However, the high SYNTAX score group demonstrated a significantly lower rate of TLF in the EES group (10.3% vs. 30.0%, p=0.01) (Figure 2 and Figure 3), which was driven by a reduction in TVMI and clinically-driven TLR.
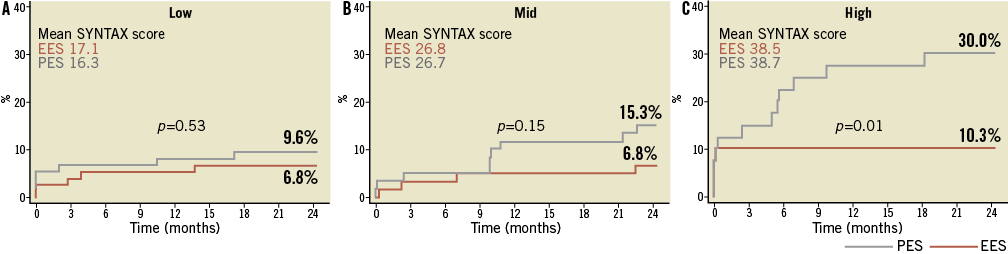
Figure 2. Kaplan-Meier estimates of 2-year TLF by baseline SYNTAX score tertile. A) Patients with low baseline SYNTAX score (0 to 22); B) intermediate baseline SYNTAX score (23 to 32); and C) high baseline SYNTAX score (≥33). p-values from log-rank tests.
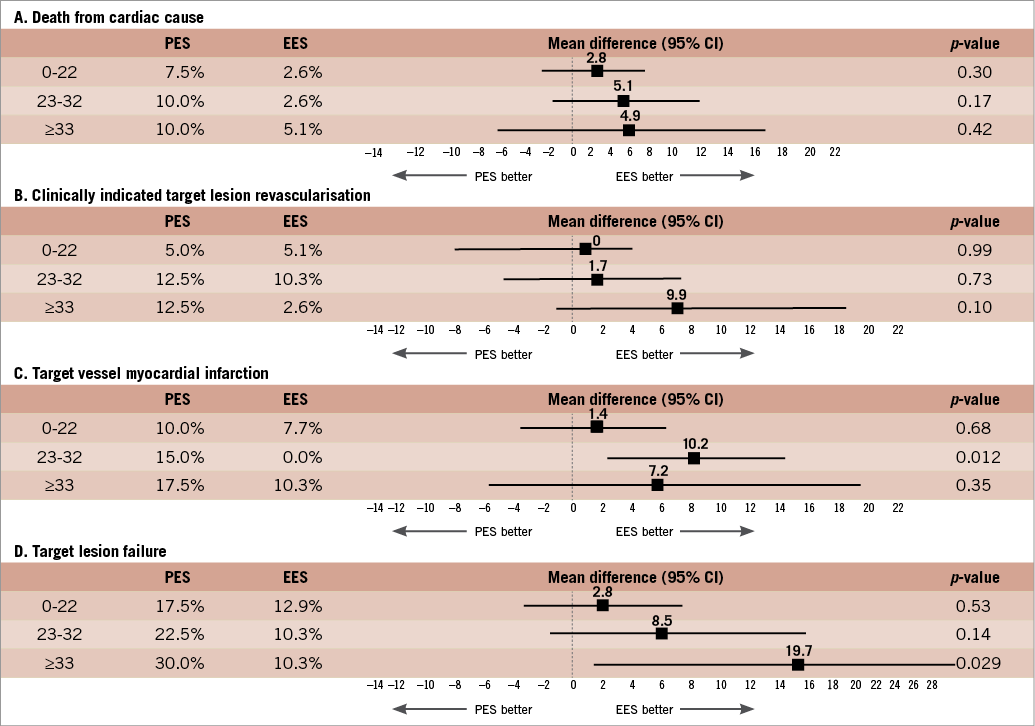
Figure 3. 2-year incidence of A) death from cardiac cause; B) clinically indicated TLR; C) target vessel myocardial infarction; and D) TLF in patients with low (0 to 22), intermediate (23 to 32) or high (≥33) baseline unadjusted SYNTAX score. Values are binary means presented with the 95% CI around the difference of the means.
TVMI was notably higher in patients with an intermediate SYNTAX score in the PES group (6.8% vs.0.0%, p=0.04). Patients with low (≤22) SYNTAX score had similar outcomes for MACE at one year (9.6% vs. 6.8%, p=0.67) for PES and EES, respectively. The subgroup containing intermediate (22 to 33) SYNTAX scores demonstrated higher MACE rates in those patients with PES compared to EES (15.3% vs. 5.1%). This was similar in those patients with a high (≥33) SYNTAX score for PES and EES (30.0% vs. 15.4%), respectively, although these were not significant.
STENT THROMBOSIS
Overall rates of ST were low with only one confirmed case (0.6%) in each group. Patients had a significantly lower rate of the combined endpoint of definite, probable and possible ST in the EES group (1.7% vs. 7.0%, p=0.02).
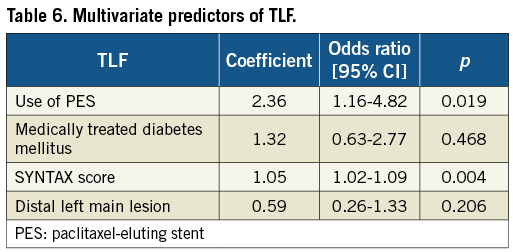
MULTIVARIATE PREDICTORS OF TLF AT TWO YEARS
Multivariate analysis was performed to identify the predictors of TLF (Table 6). Importantly, use of PES was the strongest predictor of TLF, followed by high SYNTAX score.
Discussion
The main finding of this large multicentre comparison of two left main stem registries is that EES use in LMS disease is associated with a decreased rate of TLF at two years, driven mainly by decreased ST and target vessel MI.
In addition, use of PES in ULM disease and increased SYNTAX score were demonstrated to be independent predictors of TLF. EES were shown to be significantly beneficial in patients with a high SYNTAX score with regard to the composite endpoint of TLF, with a trend towards significance in the intermediate SYNTAX score group. PES did not demonstrate superiority over EES with regard to any of the clinical endpoints.
First-generation DES have been associated with encouraging mid and long-term outcomes, results that have been additionally validated in ULM disease3-6,21. Many observational studies have compared mid-term outcomes using PES and sirolimus-eluting stents (SES) in the ULM. The MAIN-COMPARE study compared LM outcomes in 669 patients with a SES versus 189 patients treated with a PES22. At three-year follow-up there was no difference in death, MI, repeat revascularisation or ST. These results were matched by the smaller RESEARCH and T-SEARCH registries, which showed comparable outcomes at two-year follow-up23.
A randomised study by Mehilli showed SES and PES were equally effective and safe in this setting4. Six hundred and seven patients were randomly assigned to receive either SES or PES for ULM disease. Results for both groups at one-year follow-up showed no significant differences in terms of the cumulative endpoint of death, myocardial infarction or TLR (13.6% vs. 15.8%, p=0.44), nor mortality (19.7% vs. 8.7%) at two-year follow-up for PES and SES, respectively. Definite ST at one year was low and comparable with previous published data. However, even with these encouraging results, there remain outstanding issues concerning ST and the need for repeat revascularisation. The multicentre TRUE (Taxus in Real-life Usage Evaluation) registry provided similar results24.
The XIENCE V® (Abbott Vascular, Redwood City, CA, USA) everolimus-eluting stent was introduced to address the limitations of first-generation DES. The cobalt-chromium stent platform with its open-cell design offers excellent deliverability. Moreover, the combination of a thin fluoropolymer eluting the antirestenotic drug everolimus provides both an effective suppression of neointimal tissue and rapid re-endothelialisation above and between stent struts and should help to decrease ST.
The XIENCE V has been compared with PES in two randomised trials15,16. The COMPARE study demonstrated that EES was superior to the TAXUS Liberté® stent with significant differences in the composite endpoint of death, non-fatal MI and TVR at two years. SPIRIT IV investigators randomised 3,690 patients in a 2:1 fashion to the XIENCE V or the TAXUS Express® stent. At two years, treatment with the EES resulted in a 30% relative risk reduction in TLF, and the composite endpoint of cardiac death, TVMI and ischaemia-driven TLR.
Our registry comparison shows that, in two matched groups of patients undergoing ULM stenting, there are notable differences between the stents at two years. EES were associated with significantly lower rates of TLF (7.6% vs. 16.3%, p=0.01), TVMI (4.1% vs. 9.9%, p=0.03) and clinically indicated TVR (8.7% vs. 12.8%, p=0.02) when compared with PES. The use of EES was associated with a reduction in cardiac death (2.3% vs. 6.4%, p=0.07) but was non-significant. In addition, EES were seen to perform more favourably with regard to the device-orientated composite (7.6% vs. 17.4%, p=0.006). The heterogeneity of inclusion criteria and technical approaches in LM stenting trials with other DES preclude us from making any fair comparisons with other DES, but it is noteworthy that our TVR and TLR rates are among the lowest reported2-6,21,25. Though in this matched registry where the inclusion criteria and technical approaches are matched, it seems reasonable to preclude that the favourable results are attributable to the EES alone. Moreover, multivariate analyses showed the use of PES to be an independent predictor of TLF.
The recently published study by Valenti26 compared one-year outcomes in patients with left main stem disease treated with PES and EES. Their findings provide further support for our results with a significant reduction in restenosis, TVF and MACE, driven largely by a reduction in TVR. It is noticeable that the events in the PES group are higher than those reported in our study. The SYNTAX score is not reported, though the patients in this study had a higher EuroSCORE than in our registry so may have been a higher SYNTAX score population.
STENT THROMBOSIS
Concerns have been raised regarding the risk of late and very late ST following DES implantation. This is of particular concern in LM stenting where acute ST could prove fatal. Registry data of PCI with DES used in ULM lesions have shown that at mid-term clinical follow-up this is safe and feasible27. A retrospective multicentre analysis of 731 patients with either PES or SES implanted into ULM lesions showed a reassuring 0.9% incidence of definite and probable ST at 30 months28. Our rates of 0.6% (EES) and 1.2% (PES) of definite or probable ST are consistent with these findings. The difference is not significant due to the small number of patients; however, this becomes significant when all ST are considered between the groups. All our patients were taking dual antiplatelet therapy at six-month follow-up though previous studies have shown low very late ST rates in patients with EES with or without dual antiplatelet therapy at two-year follow-up13,14.
Due to concerns with the over-reporting of possible ST, we evaluated our outcomes, taking into account the definition of possible (modified) ST as described by Cutlip et al20. This did identify a significant difference in favour of the XIENCE stent in terms of possible (modified) ST (p=0.04) but no differences in definite or probable ST.
PCI OF DISTAL LM LESIONS
The distal LM is involved in 60-90% of patients with LM lesions. Stent implantation in these patients is a major challenge and provides less optimal outcomes than those achieved after non-distal LM stenting. The ideal approach for stenting the distal LM is unknown but evidence suggests that less favourable results are achieved when a two-stent strategy is used29. Our findings support this with side-branch stenting identified as an independent predictor of MACE (OR 2.31; 95% CI: 1.00-5.31, p=0.049). We know from clinical practice that use of a two-stent technique usually represents a more complex lesion and, as our patients were not randomised to either approach, we cannot draw any conclusions from this. A simple one-stent approach is preferable when the side branch is small and/or mildly diseased. However, in our registry with 46% of patients with Medina 1,1,1 lesions, the choice of strategy was more difficult. Therefore, we chose to perform a provisional side-branch T-stenting technique followed by final kissing balloons. If this yielded a suboptimal result at the side-branch ostium, a second stent was used.
RISK STRATIFICATION AFTER PCI FOR LM DISEASE
In patients with ULM disease, the ability to predict individual outcomes can assist the assessment of different treatment strategies. EuroSCORE has been used to stratify patients undergoing PCI though it does not incorporate information regarding anatomy and extent of coronary artery disease. SYNTAX score is emerging as an important determinant of outcomes after PCI18, and has been shown to be instrumental in the short and long-term risk stratification of patients with multivessel disease30. Recent analyses have demonstrated the concordance between clinical outcomes and SYNTAX score after LM PCI6,31 and the SYNTAX score is now included in the ESC guidelines in the decision-making process for revascularisation in LM disease10. We found an increase in TLF at two years in the subgroup of high SYNTAX score compared with intermediate and low scores for both stents. PES had numerically more events in each group but this was only significant in the high SYNTAX score patients (30.0% vs. 10.3%, p=0.03). SYNTAX score was found to be an independent predictor of TLF. EuroSCORE was not predictive of events.
We acknowledge that the SYNTAX score was validated for MACCE and not TLF. However, we can conclude that the difference between the stents with respect to TLF progressively increases as the complexity of the procedure (by default the SYNTAX score) increases. We also acknowledge that the SYNTAX score has been validated for cardiac mortality but the number of cardiac deaths reported in our study is too small to allow us to determine whether such a difference exists in our study. Our data would suggest that, in these patients, the SYNTAX score may be stent-dependent and the definition of “high” is different between PES and EES. Thus, it may be possible to raise the boundaries for “high SYNTAX score” in those patients undergoing ULM stenting with EES.
The present data suggest an important difference between the newer second-generation DES and first-generation stents. In addition to other studies, including the EXCEL study (Clinical Trials.gov Identifier: NCT01205776), which will include only recipients of EES, this could have important implications for clinical decision making.
LIMITATIONS
The non-randomised nature of this multicentre registry constitutes its limitation. Because of the exploratory nature of the present study, no a priori sample size was calculated. Angiographic follow-up was not routinely performed and therefore the restenosis rate may be underestimated in both groups. The TAXUS registry events were not validated by a CEC but, had this been performed, we would have expected the number of clinical events to rise and the differences between the stents to be more marked.
We noticed a significant difference with regard to the post-PCI QCA measurements. We felt that this difference was likely related to the diameters of stents available when the registry was performed, which for EES was 4 mm and PES 3.5 mm. In the LEMAX registry, the 4 mm stent was used in 38.4% of patients; however, this could have affected the outcome in favour of EES.
Conclusion
In this matched comparison of EES versus PES for the treatment of LM disease, second-generation stents were safer and more effective than PES. This difference in safety and efficacy was progressively more pronounced as the lesion complexity increased.
Funding
Stents for the study were provided by Boston Scientific, Natick, MA, USA, and Abbott Vascular, Santa Clara, CA, USA.
Conflict of interest statement
The authors have no conflicts of interest to declare.