Abstract
Aims: Limited data are available on the long-term outcome following PCI with paclitaxel-eluting stent (PES) implantation in patients with unprotected left main coronary artery (LMCA). The objective of this study was to evaluate “real world” long-term outcome following paclitaxel-eluting stent (PES) implantation for unprotected LMCA disease in patients enrolled in the TRUE registry.
Methods and results: From March 2003 to October 2004, 93 consecutive patients (81.7% male) underwent PCI for unprotected LMCA disease. Surveillance angiography was performed at 6.8±3.3 months follow-up. The target lesion involved the distal LMCA in 68 (73.1%) patients. Double stenting techniques were performed in 46 (67.6%) distal LMCA, of these 50% were stented using the Crush technique. Clinical follow-up was complete in all patients with 85.8% angiographic follow-up rate. In-segment restenosis occurred in 16 (20.3%) patients and was focal in 72.4% of cases and significantly higher in patients with distal LMCA (36.8% vs. 13.6%, p<0.04). At a median follow-up of 1,450 days (IQR 1281-1595), the overall incidence of MACE was 35.5% and the TLR rate was 25.8% and significantly higher in patients with bifurcation stenting (32.3% vs. 8%, p<0.02). The estimated cardiac survival rate at one and four years was 96.7% and 93.3%, respectively. Total mortality rate was 14.1% and cardiac was 6.5%. There was one (1.1%) definite stent thrombosis (ST) and one (1.1%) probable ST.
Conclusions: Treatment of unprotected LMCA disease with PES, after four years follow-up, appears to be safe and effective with a low rate of cardiac mortality and overall risk of ST. The need for target lesion revascularisation in 25.8% of patients highlights the need for more effective PCI especially in patients with distal LMCA disease.
Introduction
Coronary artery bypass surgery (CABG) remains the recommended therapy for patients with left main coronary artery (LMCA) disease. However, reduced restenosis rates with drug-eluting stents (DES) have raised the possibility of their use in more complex patient subsets. Several studies about DES have demonstrated the safety and feasibility of percutaneous coronary intervention (PCI) for unprotected LMCA disease1-5 and a recent report showed favourable long-term clinical results6,7. Despite these encouraging data, restenosis and target vessel revascularisation are still present when distal LMCA is involved8. Furthermore, limited data are available on the long-term clinical follow-up of patients treated percutaneously6,7. Therefore, the objective of this study was to evaluate the long-term (four years) outcome following paclitaxel-eluting stents (PES) implantation for unprotected LMCA disease in the TRUE registry (Taxus in Real-life Usage Evaluation).
Methods
Study design
The present study included all consecutive patients, from March 2003 to October 2004, with a de novo critical stenosis in an unprotected LMCA electively treated with PCI with PES (Taxus®, Boston Scientific, Natick, MA, USA) in seven centres of the TRUE registry9. Unprotected LMCA critical stenosis was defined as ≥50% angiographic diameter stenosis (visual estimation subsequently confirmed by QCA analysis) within the LMCA without distal protection by previous CABG. Patients with high-grade ostial lesions involving the left anterior descending artery (LAD) or the circumflex artery (LCx) were included if the left main also contained a 50% stenosis requiring stent implantation. Patients were subdivided in two groups on the basis of lesion location within the left main segment: 1) non-bifurcation group, if the lesion was confined to the ostium or body of the left main; 2) bifurcation group, if the lesion involved the bifurcation of the left main.
The decision to perform PCI versus CABG was considered when one of these two conditions was present: 1) preference by the patient and by the referring physician for a PCI approach, both of them being aware of the procedural risks; 2) contraindication to surgery on the basis of the presence of comorbidity evaluated by a cardiac surgeon. Exclusion criteria were: ongoing (<48 hours) ST-elevation and non-ST elevation acute myocardial infarction, cardiogenic shock, contraindication for antiplatelet therapy, stenting of LMCA due to dissection of ostial LMCA induced by guiding catheter or dissection induced by LAD or LCx stenting. The primary endpoint of the study was the incidence of major adverse cardiac events (MACE) at four years follow-up. MACE were defined as the occurrence of: cardiac death, myocardial infarction (Q-wave and non-Q wave), target lesion revascularisation and target vessel revascularisation, either percutaneous or surgical including the ostia of LAD or/and LCx. Secondary endpoints were: 1) incidence of binary in-segment restenosis and 2) in-segment minimum lumen diameter, late lumen loss, and loss index at angiographic follow-up. The study protocol was approved by the Ethics Committee of each participating centre and all patients provided written informed consent.
Definitions
Angiographic success was defined as the achievement of residual stenosis <20% with at least TIMI flow III10. Procedural success was defined as the achievement of angiographic success in the absence of any in-hospital MACE. A non–Q-wave myocardial infarction was defined as elevation of CK-MB or troponin I or T levels to >3 folds the upper limit of the normal value in the absence of pathological Q waves. Deaths were classified as either cardiac or non-cardiac. Deaths that were unexplained were considered to be cardiac. Target lesion revascularisation was defined as any repeat PCI in the target segment or CABG of the target vessel performed for restenosis or other complications related to the target lesion, including the ostium of the LAD and/or LCx. Target vessel revascularisation was defined as any repeat intervention (percutaneous/bypass surgery) within the treated vessels. A revascularisation was considered clinically indicated according to the Academic Research Consortium (ARC) definition11. The Parsonnet score and European system for cardiac operative risk evaluation (EuroSCORE) were used to stratify the risk of death at 30 days. Patients were stratified as high risk in the presence of a EuroSCORE ≥6 and/or Parsonnet ≥15 and as very high risk if EuroSCORE was ≥13 and/or Parsonnet was ≥2012,13. Bifurcations were classified according to the more recent classification proposed by Medina et al (Figure 1)14, and trifurcations were defined as previously reported15,16. Stent thrombosis (ST) definition used in this study is consistent with the newest consensus of ARC11.
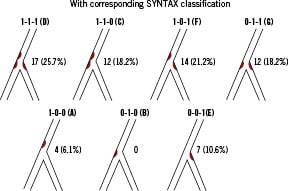
Figure 1. Bifurcation classification according to the definition proposed by Medina14. To facilitate comparison with previous reports, bifurcations are categorised using the SYNTAX classification35. Each combination with side branch disease can be distinguished in ostial (O) or diffuse (d). True bifurcation 111-d (6.1%) or 111-O (19.7%).
Interventional procedure
Before the procedure, all patients received oral aspirin once daily and clopidogrel (a loading dose of 300 mg at least two hours before the procedure). Patients who had been pre-treated with ticlopidine (250 mg twice a day) or clopidogrel (75 mg once daily) for at least 72 hours did not receive a clopidogrel loading dose. Balloon pre-dilatation, post-dilatation, rotational atherectomy, directional atherectomy, or intravascular ultrasound evaluation (IVUS), and the use of glycoprotein IIb/IIIa inhibitors were left to the discretion of the operator. IVUS was performed for lesions with poor visualisation by angiography only (e.g., pre-procedurally for highly eccentric, but non-critical, stenoses and periprocedurally to clarify the nature of luminal haziness).
When the distal LMCA was stenosed, we considered the main vessel (MV) to be the LMCA towards the LAD and the side branch towards the LCx. The LMCA lesions at the ostium or shaft without involvement of bifurcation were usually treated with a single stent. Bifurcation lesions were treated at operator’s discretion. At discharge patients received a regimen of aspirin (100 mg once daily indefinitely) and clopidogrel (75 mg once daily) or ticlopidine (250 mg twice a day) for at least six months.
Clinical follow-up
Clinical follow-up was conducted by telephone contact or office visit at one and seven months and at one, two, three and four years following the index procedure. Angiographic follow-up was planned for six months after the procedure, or earlier if a non-invasive evaluation or the clinical history suggested the presence of recurrent myocardial ischaemia. The TRUE study is based on a dedicated web-based data entry system, enabling real time data access, monitoring, and event adjudication as previously reported9.
Quantitative coronary angiography
Coronary angiograms were analysed in an independent core angiographic laboratory (Angiographic Core Laboratory, Mediolanum Cardio Research, Milano, Italy) with a semi-automated edge contour detection computer analysis system (Content Management System version 6.0, Medis, Leiden, The Netherlands) at baseline, after the procedure and at follow-up. The target lesion was defined as involving the distal LMCA if it was within 3 mm of the branch ostia. Binary restenosis was adjudicated in case of >50% diameter stenosis (by quantitative coronary angiography analysis) at the target site or ostium of the LAD and/or LCx demonstrated at the follow-up angiography, irrespective of clinical symptoms of the patient.
Quantitative analysis was performed in the ‘in-stent’ area (‘in-stent’ analysis, including only the stented segment) and in the ‘in-segment’ area including the stented segment as well as both 5 mm areas proximal and distal to the stent (‘in-segment’ analysis). Focal restenosis was defined as a restenotic lesion <10 mm long and diffuse restenosis as ≥10 mm long17.
Statistical analysis
Continuous variables were reported as mean±standard deviation (SD) or median (interquartile range, IQR) and compared with Student’s t test or Mann–Whitney or Wilcoxon tests, when appropriate. Categorical variables (as frequencies or percentage) were compared with χ2 statistics or Fisher exact test. Clinical events were analysed on a per-patient basis; and Quantitative Coronary Angiography data, on a per-lesion basis. Event-free survival during follow-up at four years (97.8% of patients) was evaluated according to the Kaplan-Meier method and survival among groups was compared using the log rank test. Factors that predicted MACE and angiographic outcomes were identified by univariate and logistic regression analyses (backward stepwise algorithm cut-off for entry 0.05, for removal 0.10). To avoid overfitting of the multivariate model, the convention of limiting the number of independent variables entered to approximately 10% of the number of events was followed. In our analysis, independent variables for entry into the multivariate model were selected according to their weight on univariate testing (p values <0.1 and shorter 95% confidence intervals). Goodness of fit of the logistic regression analysis was also assessed with the Hosmer-Lemeshow statistic. All statistical analysis was performed using SPSS 16.0.2 (SPSS Inc., Chicago, IL, USA), with significance set at the 2-tailed 0.05 level.
Results
Clinical characteristics
Among the complete patient cohort of the TRUE registry (1,065 patients with 2,116 lesions), we identified a consecutive series of 190 patients treated with PES implantation in LMCA (112 with unprotected LMCA). Of these only 93 patients that had a significant angiographic coronary stenosis (confirmed by QCA analysis) involving an unprotected LMCA and/or ostium of LAD-LCx, entered onto this study in accordance with the inclusion criteria. Baseline clinical characteristics of the patients who entered the study are reported in Table 1.
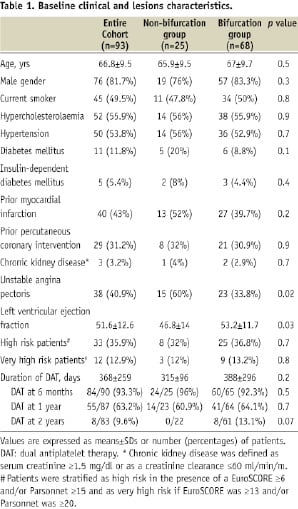
The mean age of the patients was 66.8±9.5 (range, 40 to 88); 18.3% had 3-vessel disease, 3.2% had chronic kidney disease, 35.9% were at high risk and 12.9% at very high risk according to EuroSCORE and Parsonnet. The lesion involved the distal LMCA in 68 patients (73.1%). Five patients (5.3%) underwent PCI with PES for unprotected LMCA true trifurcation disease (according to modified Medina classification the trifurcation was type 1,111 in three patients and 1,011 in two).
Lesion characteristics and procedural outcomes
Lesion and procedural characteristics are reported in Table 2.
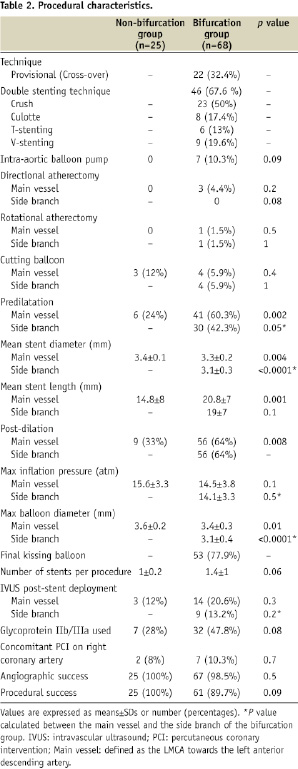
Overall angiographic success was obtained in 92 patients (98.9%) and procedural success in 86 patients (92.5%). When distal LMCA was treated a cross-over stenting approach was performed in 32.4% of the cases. In 67.6% of distal LMCA a double stenting technique was indeed chosen: the Crush technique was preferred in 50% of them. Intra-aortic balloon pump support was used in 7.5% of patients overall and glycoprotein IIb/IIIa antagonists were used in 41.9% (elective in 79.4% of the cases). Nine patients (9.6%) also underwent PCI in the right coronary artery in the same procedure. Final kissing balloon inflation was performed in 77.9% of the bifurcation group and was significantly higher in the bifurcation lesions treated with 2-stents compared to 1-stent (80.4% vs. 36.2%, p<0.0001). Intravascular ultrasound was used in only 18.2% of the cases.
Angiographic outcomes
The quantitative coronary angiography analysis is shown in Table 3.
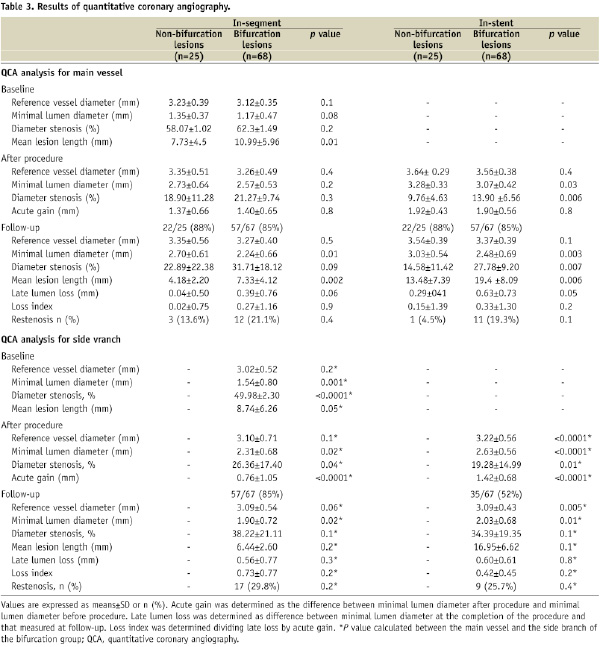
Angiographic follow-up was performed in 85.8% of eligible patients (n=79) at 6.8±3.3, months of follow-up. There were no differences for age, sex and classical risk factors between patients undergoing angiographic follow-up and those who did not. The rate of in-stent binary restenosis per patient was 20.3% (16/79 patients), and per lesion was 18.4% (21/114 stented lesions). Only one patient (4.5%) had restenosis in the non-bifurcation group. The restenosis involved only the proximal or the distal stent edge in 23.8% of cases (5/21 of the in-stent restenosis). Compared to the non-bifurcation group, the bifurcation group had a significantly higher in-stent (26.3%, 15/57 vs. 4.5%, 1/22; p<0.03) as well as in-segment binary angiographic restenosis (36.8%, 29/57 vs. 13.6%, 3/22, p<0.04).
In the bifurcation group, most (72.4%, n=21) of restenotic lesions were focal, (24% diffuse and 3.6% proliferative). No case of occlusive restenosis occurred. Of these restenotic lesions, the majority (58.6%, 17/29) occurred in LCx ostium, 27.5% (8/29) in the MV trunk and in 24.1% (7/29) involved both LAD and LCx ostia.
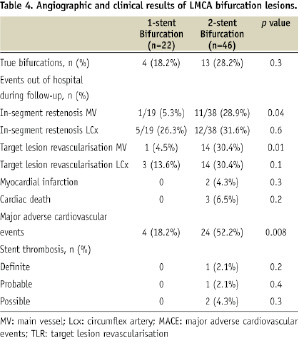
Comparing the 2- to 1-stent technique (see Table 4), true bifurcations were treated in 28.2% of the cases with 2-stent approach and in 18.2% with 1 stent. A significantly higher rate of in-segment restenosis involving the MV (28.9% vs. 5.3%, p<0.04) and also a significantly higher rate of target lesion revascularisation (30.4% vs. 4.5%, p<0.01) was observed with 2 stent technique.
In-hospital and long-term MACE
In-hospital and long-term MACE are shown in Table 5.
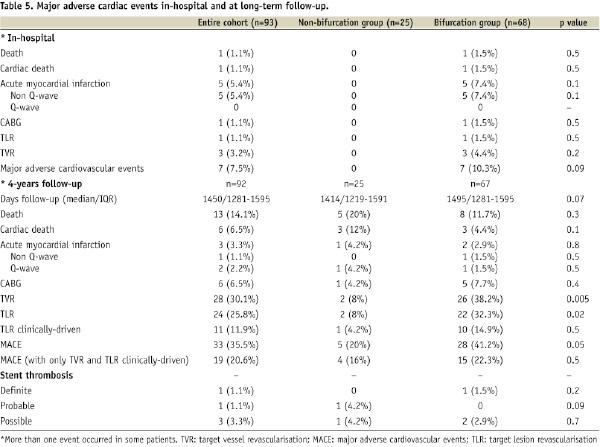
In-hospital complications occurred in six patients (6.4%): there was one death (1.1%) due to slow-flow as a result of a proximal dissection during crush stenting with subsequent cardiogenic shock that required emergency CABG; the death occurred from low cardiac output and multi-organ failure. Five patients (5.4%) had non Q-wave myocardial infarction.
Long-term clinical follow-up (median 1,450 days, IQR 1281-1595) was performed in all eligible 92 patients. During the follow-up period, 13 patients (14.1%) died (clinical and procedural characteristics of these patients are illustrated in Table 6).
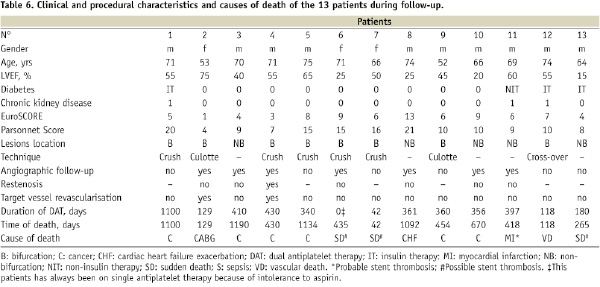
Six patients (6.5%) died of cardiac cause: three within six months after the procedure, of these two were sudden deaths (one patient on single antiplatelet therapy) and one after CABG performed for recurrence of effort angina. The other three patients died >2 years after the procedure, one was a sudden death, one a very late probable ST and the last was a death for heart failure. Seven deaths (63.6%) were non-cardiac due to cancer. The estimated cardiac survival rate was 96.7% at one year and 93.3% at four years (Figure 2A). The estimated overall survival rate and cardiac survival rate at four years were equal between the bifurcation and non-bifurcation groups (83.8% and 88%; p=NS and 91% and 96%; p=NS, respectively). Myocardial infarction occurred in three patients (3.3%): one was caused by a definite ST, one was a non-Q wave myocardial infarction with subsequent death without angiographic confirmation of ST (probable ST) and the last case was a non-target vessel acute myocardial infarction. Target lesion revascularisation was performed in 24 patients (25.8%), was clinically-driven in 11.9% of cases and CABG was performed in 6/24 patients (25%). In total, the rate of MACE was 35.5% and was significantly higher in the bifurcation group (41.2% vs. 20%, p < 0.05). Figure 2 shows the Kaplan-Meier curves for freedom from MACE and target lesion revascularisation (Figure 2B and Figure 2C, respectively). The percentage of patients free from target lesion revascularisation was significantly lower in the bifurcation group (consisting of both pseudo-bifurcations and true-bifurcations) compared to the non-bifurcation group (Figure 2C).
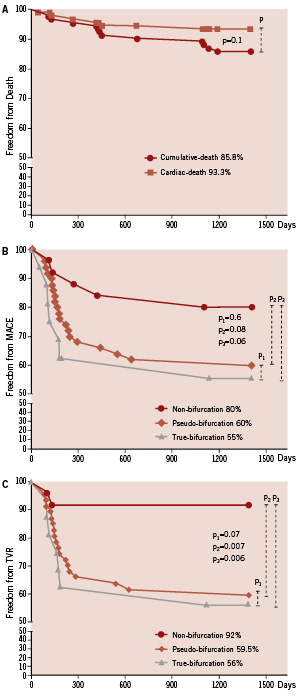
Figure 2. (A) Kaplan-Meier analysis and log-rank test of survival free of death over follow-up. (B) Kaplan-Meier analysis and log-rank test of survival free of MACE in three sub-groups (non-bifurcation, pseudo-bifurcation and true-bifurcation lesions). (C) Kaplan-Meier analysis and log-rank test of survival free of TVR over follow-up in the three sub-groups.
Stent thrombosis
The ST events are reported in Table 5. There was one case (1.1%) of definite ST that occurred 114 days after the index procedure on dual antiplatelet therapy. The patient experienced an anterior-ST-elevation myocardial infarction with angiographic evidence of ST in the proximal part of LAD, successfully treated with intracoronary administration of thrombolytic and, the day after, with rescue PCI. There was one (1.1%) very late probable ST (418 days) presenting with myocardial infarction with ischaemia in the territory of the implanted stent in a patient on aspirin therapy. Possible ST was considered in three patients (3.3%) with unexplained sudden death, of which two patients also had severe left ventricular dysfunction (LVEF < 30%), one of that without the protection of an implantable cardiac defibrillator. The rate of any ARC defined ST was 5.5%.
Multivariate analysis
Multivariate predictors of adverse outcomes are listed in Table 7.
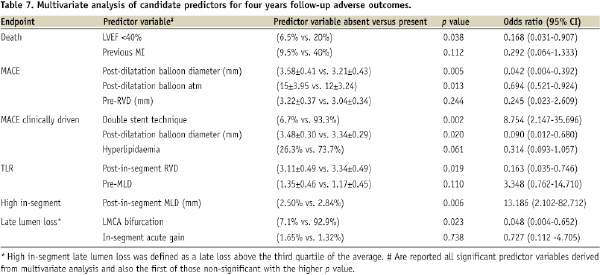
There were no significant predictors of cardiac death, parent vessel and LCx restenosis. Low ejection fraction (<40%) was associated with death and post in-segment MLD with more in-segment late lumen loss.
Discussion
The main findings of this report are: 1) at long-term clinical follow-up (median 1,450 days) following elective PES implantation in unprotected LMCA the incidence of cardiac death was 6.5% and definite and probable ST 1.1% (90% of patients were taking only aspirin at the last follow-up contact); 2) restenosis is more present when distal LMCA was treated especially with a widespread 2-stent approach; 3) when restenosis occurs on the distal bifurcation, the most common pattern was focal (72.4%), and frequently involved only the ostium of the side branch, i.e., LCx (58.6%).
Current ACC/AHA guidelines for PCI recommend surgical revascularisation in patients with unprotected LMCA disease18. The main reason for this recommendation is that long-term outcomes of surgical revascularisation, including the subpopulation with unprotected LMCA disease, are available and in consideration of recent results highlighted in the SYNTAX study19-21. To the best of our knowledge this is the longest follow-up reported in the literature for unprotected LMCA intervention. Three-year cumulative survival rate of elective patients with unprotected LMCA disease treated with CABG was 91% in the CASS study20 and 92% in the study reported by d’Allones et al19. Similarly, the 3-year cumulative survival rate of elective patients with unprotected LMCA disease treated with PCI was 93.4% in the study reported by Meliga et al6. In our study the cumulative survival and cardiac survival rates with a follow-up of four years were 85.8% and 93.3%, respectively (Figure 2A), without significantly differences between bifurcation and non-bifurcation groups.
Recently Chieffo et al7 reported a cumulative rate of ST of 1.49% (0.54% definite and 0.95% probable, respectively) in 731 patients at 29.5 months of follow-up. Similarly, in the present registry, the cumulative rate of definite and probable ST was 2.2% (1.1% and 1.1%, respectively) at 48.3 months of follow-up. It is worth mentioning that over 90% of our patients were taking only aspirin at the time of the report and from two to four years there was no event of ST according to any ARC definition.
Several observational registries have reported favourable midterm results following DES implantation in unprotected LMCA disease1-5 and recently encouraging results have been described also at long term clinical follow-up5,22-25. In particular, extremely positive results have been observed in non-bifurcation unprotected LMCA lesions with a 2-year incidence of MACE of 7.4%23. By contrast, a high incidence of MACE have been reported up to 44%, when there is involvement of the distal bifurcation8,26. Overall midterm follow-up of a meta-analysis for DES in >1200 unprotected LMCA, reported by Biondi-Zoccai et al27, showed MACE in 16.5% (11.7-21.3), death in 5.5% (3.4-7.7), and TVR in 6.5% (3.7-9.2).
In addition, previous studies reported restenosis rates ranging from 2% to 35%, but in these studies the proportion of patients who were treated with bifurcation stenting varied from 8% to 84%, respectively. Recently, Price et al8 performed LMCA intervention with SES in 50 patients (94% with distal left main disease) with 84% of patients having both LMCA branches stented. The binary restenosis in the main and side branch was 23% and 35%, respectively, and the TLR rate was 38%. This unfavourable outcome is in accordance with our data, and may be explained by the large proportion of patients treated for bifurcation lesion (73.1%), the predominant use of 2-stent techniques (67.6%) and by the length of long-term of clinical follow-up (median 1,450 days). Moreover, a less aggressive approach than currently employed (lack of IVUS usage in most patients, mean inflation pressure 14-16 atm, post-dilatation of only 1/3 of non-bifurcation stents), may account for the relatively small MLD post procedure and significant restenosis rate (side branch MLD 2.31 and restenosis rate 29.8%, for example). Given the recent data on the optimal treatment of bifurcation lesions, our study showed a relatively high incidence of the use of the two-stent technique. Despite only 28.2% of subjects have a true bifurcation lesion (which might have encouraged the operator to consider the more aggressive two-stent strategy), as many as 67.6% of lesions were tackled with two stents. Certainly, within our practice, we increasingly select a single stent provisional strategy where possible, even in the left main. Whether the current manuscript data therefore reflects optimal bifurcation strategy is a debatable point of interest.
As previously described8, it is also reasonable to examine patients who underwent “clinically-driven” target lesion revascularisation within a trial such as this, as we know that routine angiographic follow-up can precipitate unnecessary interventions and excessively elevate the MACE rate. In our study, target lesion revascularisation triggered by symptoms or ischaemia testing was found in only 11 patients (11.9%), meaning an overall clinically-driven MACE rate of 20.6%, as opposed to the headline MACE rate of 35.5%.
Previous studies26,28-30 on bifurcation stenting showed a low restenosis rate in the main vessel. However, such studies did not show a benefit of side-branch DES over balloon angioplasty in terms of side-branch patency. However, in recently reported data from the RESEARCH and T-SEARCH registries, cumulative MACE rates were similar between single-vessel stenting and bifurcation stenting. In particular, a study by Hoye and co-authors31 showed that although the crush technique of bifurcation stenting with DES was associated with favourable outcomes for most lesions, efficacy appeared significantly reduced in LMCA bifurcation. In the present study, the side branch angiographic in-segment restenosis rate was not significantly higher in the 2-stent group compared to the 1-stent group (31.6% vs. 26.3%, p=NS). Moreover, we found a significantly and unexpected higher rate of in-segment restenosis and need of target lesion revascularisation in the MV of the 2-stent group compared to 1-stent group (28.9% vs. 5.3% for in-segment restenosis p<0.04; 30.4% vs. 4.5% for target lesion revascularisation, p<0.01; respectively). Finally, from our data, no conclusions can be drawn about the different stenting techniques as predictor of restenosis since the bifurcation stent approach was not randomised and the number of patients receiving double stenting was small. The SYNTAX study reported, at one year follow-up, an higher rate of target vessel revascularisation in the PCI group compared to CABG group (11.8% vs. 6.5%, p=0.02), but this result was offset by a significantly higher rate of stroke in the CABG sub-group of patients (2.7% vs. 0.3%, p=0.01).21 Although this study provided very important information about the current treatment of complex coronary artery disease, a 12 month follow-up period is not sufficient to fully delineate the differences in efficacy between either treatment. We need to see long-term follow-up data from this trial, ideally that gathered at the pre-specified completion date of five years. The long-term results of our smaller study are therefore complementary to our interpretation of the currently available Syntax data and contribute to the better understanding of the impact of using DES to treat patients previously considered as suitable only for surgery.
Study limitations
This registry did not evaluate a large study cohort of patients treated by stenting for unprotected LMCA disease. However, careful selection of patients according to the inclusion criteria (critical angiographic stenosis confirmed by QCA analysis), the complete long-term clinical and good rate of angiographic follow-up can be of value to better understand the outcome of PCI in this patient’s subset. Other limitations include the lack of IVUS usage in most patients, and the evidence of relative low final maximal inflation pressure. It is worth noting, that this registry encompasses early experience and a treatment modality which has changed with time in relation to the learning curve for LMCA treatment. Previous studies have demonstrated the utility of intravascular ultrasound in the placement of left main stents, and at least one restenosis in the ostial group may have been prevented using this technique32-34 . Nevertheless, the TRUE Registry reflects the current practice in a multicentre European real-world setting including “all-comers” undergoing implantation of PES within the unprotected LMCA, and therefore any selection bias should be minimised.
Conclusions
In conclusion, patients with unprotected LMCA disease treated with PES have favourable long-term outcomes. Cardiac survival rates after four years of follow-up is comparable with that reported for CABG. Moreover, the rate of ST in the long-term follow-up is not higher than that reported in the literature, even if more than 90% of the patients were on single antiplatelet therapy after four years from stent implantation. Finally, albeit the majority of restenosis were focal, the need for target lesion revascularisation in 32.3% of patients treated for LMCA distal bifurcation demands further improvements in implantation technique to reduce angiographic restenosis in such lesions subset.
Acknowledgements
We would like to acknowledge the Angiographic Core Laboratory: Maria Antonietta Bonardi, BSc, Monica Repetto, BSc, Mario Marzanati, BSc, Mediolanum Cardio Research, Milano.
Appendix
TRUE participating centres co-investigators and number of patients with unprotected LMCA treated.
1. San Raffaele Hospital, Milan, Italy: 26
2. Careggi Hospital, Florence, Italy: 21
3. Ferrarotto Hospital, Catania, Italy: 19
4. Columbus Hospital, Milan, Italy: 15
5. Heart Centre Siegburg, Siegburg, Germany: 8
6. Royal Brompton Hospital, London, United Kingdom: 4
7. Mirano, Hospital, Mirano, Italy: 0

