Abstract
Aims: Data regarding the impact on clinical outcomes of PCI with DES implantation vs. CABG to treat unprotected left main coronary artery (ULMCA) disease in diabetic patients are still insufficient. The present study evaluated the short-term and long-term results of percutaneous and surgical revascularisation in diabetic patients with ULMCA disease in a large population.
Methods and results: A total of 826 diabetic patients with ULMCA stenosis who received DES (n=520) or underwent CABG (n=306) were selected and analysed from the DELTA registry. In-hospital MACCE was significantly higher in the CABG group, mainly driven by a higher incidence of MI. At four-year follow-up, freedom from death and the composite endpoint of death, MI and cerebrovascular accident (CVA) was similar in the two treatment groups (CABG 87.4%, PCI 82.5%, p=0.124, and CABG 85.4%, PCI 78.9%, p=0.11, respectively). Conversely, freedom from TVR and MACCE was significantly higher in the CABG compared to the PCI group (CABG 95.4%, PCI 79.4%, p<0.001, and CABG 81.9%, PCI 64.7%, p<0.001).
Conclusions: In diabetic patients with ULMCA disease with/without concomitant multivessel disease, PCI and CABG led to similar results in terms of death, MI and CVA. However, CABG was associated with less MACCE at long-term follow-up, primarily due to the higher repeat revascularisation rate with DES.
Introduction
Diabetes increases the risk of developing a diffuse and rapidly progressive form of coronary artery disease (CAD)1,2 and has been shown to be an important predictor of death, myocardial infarction (MI), and in-stent restenosis3.Together with coronary artery bypass grafting (CABG), percutaneous coronary intervention (PCI) represents a valuable and effective therapeutic strategy for diabetic patients with significant CAD4,5. Nevertheless, there are limited data that address clinical outcomes associated with PCI with drug-eluting stents (DES) and CABG to treat unprotected left main coronary artery (ULMCA) disease in diabetic patients6-8, and studies reporting long-term data are lacking. We therefore evaluated the short-term and long-term clinical outcomes of PCI with DES or CABG in diabetic patients with ULMCA disease in a large population selected from the DELTA registry (D-DELTA).
Methods
The study population consisted of 826 “all-comer” diabetic patients with ULMCA stenosis treated with PCI and first-generation DES (sirolimus- and paclitaxel-eluting stents) implantation or CABG between April 2002 and April 2006 in 14 international centres, within the DELTA (Drug Eluting stent for LefT main Artery) registry9. Factors that determined the choice of a percutaneous approach over surgery included: 1) haemodynamic conditions; 2) lesion characteristics; 3) vessel size; 4) presence of comorbidities; 5) quality of arterial and/or venous conduits for grafting; and 6) patient and/or referring physician preferences. In all cases, the selected revascularisation approach seemed suitable to guarantee complete revascularisation. Information regarding clinical status was collected with the hospital recording network, at clinic visits and by telephone interview. Data collection was carried out using a dedicated electronic case report form (CRF). All the explored variables in the CRF were defined and number-coded before the CRF was sent to each participating centre.
Dual antiplatelet therapy (i.e., aspirin 100 mg daily and clopidogrel 75 mg daily or ticlopidine 250 mg twice daily) was administered for at least 12 months in patients treated with PCI. In the Korean centre, cilostazol was also prescribed. The choice of DES was at the discretion of the physician. Stent implantation techniques for patients with ULMCA disease have already been described10,11. Interventions for any other significant coronary artery disease were performed according to current practice guidelines. Surgical revascularisation was performed using standard bypass techniques12. Angiographic follow-up was scheduled according to hospital practice or if a non-invasive evaluation or clinical presentation suggested ischaemia. This protocol was approved by the hospital ethics committees and is in accordance with the Declaration of Helsinki. Written informed consent was obtained from every patient.
Definitions
In this report, the following events were analysed cumulatively at the latest clinical follow-up available: overall death, myocardial infarction (periprocedural MI, Q-wave MI, spontaneous MI), cerebrovascular accident (CVA), target lesion revascularisation (TLR), and target vessel revascularisation (TVR). The occurrence of stent thrombosis (ST) was defined on the basis of the Academic Research Consortium definitions13 in the PCI group. Periprocedural MI was defined as the elevation of the serum creatine kinase (CK) isoenzyme myocardial band that was 3x the upper limit of normal in the PCI group and 5x the upper limit of normal in the CABG group14. Q-wave MI was defined as the development of new pathological Q-waves in two or more contiguous leads with or without CK or CK-myocardial band levels elevated above normal. Spontaneous MI was defined as the occurrence after hospital discharge of any value of troponin and/or CK-myocardial band greater than the upper limit of normal if associated with clinical and/or electrocardiogram change. CVA was defined as stroke, transient ischaemic attacks, and reversible ischaemic neurological deficits adjudicated by a neurologist and confirmed by computed tomography scanning, when appropriate. TLR was defined as any repeat percutaneous intervention of the target lesion performed for restenosis or other complication of the target lesion. The target lesion was defined as the treated segment 5 mm proximal to the stent and 5 mm distal to the stent; TVR was defined as any repeat intervention of any segment of the target vessel, defined as the entire major coronary vessel proximal and distal to the target lesion, including upstream and downstream branches and the target lesion itself. Major adverse cardiac and cerebrovascular events (MACCE) were defined as the composite endpoint of death, MI, CVA and TVR. Diagnostic angiograms were scored according to the SYNTAX score algorithm at the site laboratory15.
Study endpoints
The primary study endpoint was the incidence of death, MI and CVA at long-term follow-up. The secondary study endpoints were the occurrence of death, TVR and MACCE.
Statistical analysis
Continuous variables are expressed as mean±SD and differences were compared using Student’s t-test. Categorical variables are expressed as counts and percentages. Differences between subgroups were assessed by Fisher’s exact test or chi-square test, as appropriate. Because of the non-randomised nature of the study, a propensity score analysis was performed to minimise any selection bias due to the differences in clinical characteristics between the two treatment groups. The propensity score was determined using a non-parsimonious multivariable logistic regression model from which the probability of receiving a DES rather than CABG was calculated for each patient. Variables included in the logistic regression model to calculate the propensity score were age, sex, diabetes type, smoking, family history of coronary artery disease, unstable angina, acute myocardial infarction, chronic kidney disease, left ventricular ejection fraction (LVEF), previous CABG, previous PCI, multivessel disease, and concomitant right coronary artery disease. The C-statistic was 73.9 and the Hosmer-Lemeshow test p-value was 0.11, confirming good discrimination and calibration of the propensity score model. Thereafter, a Cox regression analysis was performed using as covariate the propensity score and treatment strategy calculated as a simple linear term.
Survival curves were generated at mean of covariates, and differences between groups were evaluated and reported using log-rank test and p-values. Statistical analyses were performed using SPSS 14.0 (SPSS Inc., Chicago, IL, USA). P-values less than 0.05 were considered statistically significant.
Results
BASELINE CLINICAL, PROCEDURAL AND ANGIOGRAPHIC CHARACTERISTICS
Baseline characteristics are shown in Table 1 and Table 2. In both groups, the majority of patients were male, with hypertension, hypercholesterolaemia, and were active smokers in forty percent of cases. Non-insulin-dependent and insulin-dependent diabetes mellitus (NIDDM and IDDM) were present in 70% and 30% of patients, respectively. The most common clinical presentation was acute coronary syndrome/non-ST-elevation myocardial infarction (ACS/NSTEMI: 56.3% vs. 64.1%, p=0.02), followed by stable angina/silent ischaemia (35.4% vs. 29.4%, p=0.07) and ST-elevation myocardial infarction (STEMI: 8.3% vs. 6.5%, p=0.83). Mean EuroSCORE in the PCI and CABG groups was 5.4±3.6 and 5.4±2.7, respectively (p=0.91).
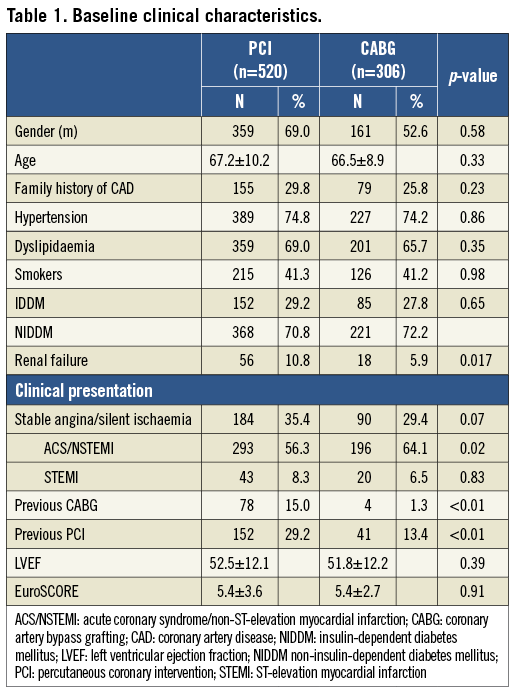
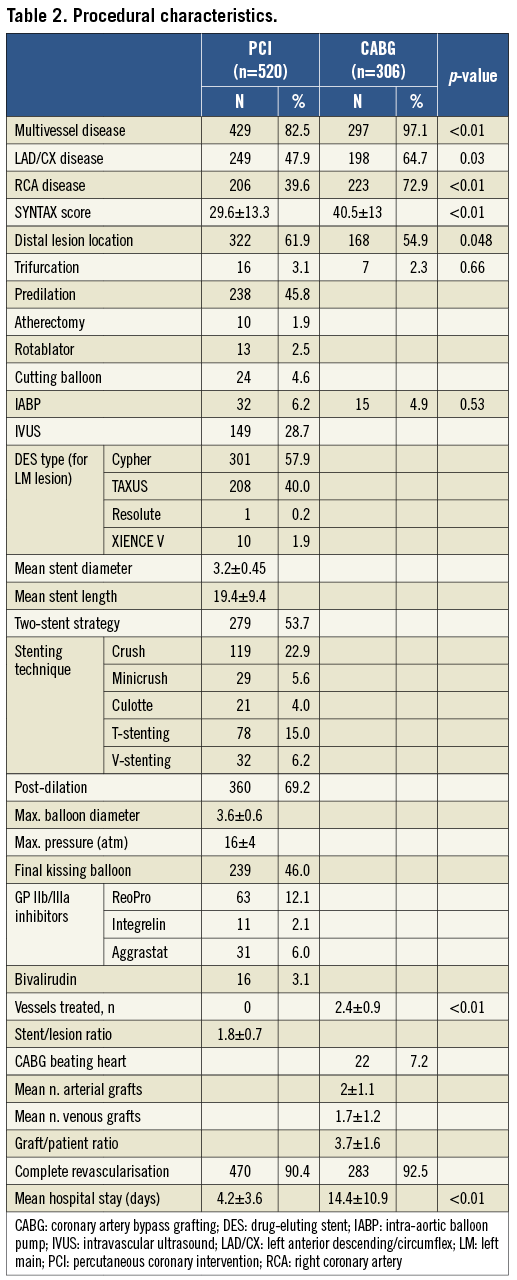
Compared with patients who underwent CABG, those who received DES had a significantly higher prevalence of renal failure, previous CABG and previous PCI. Conversely, patients who underwent CABG were significantly more likely to have multivessel disease, RCA disease and a higher SYNTAX score (29.6±13.3 vs. 40.5±13, respectively; p<0.01).
Distal lesion location was 61.9% in the PCI group and 54.9% in the CABG group (p=0.048). Approximately half of all LM lesions in the PCI group were treated with a two-stent strategy. The favoured stenting technique was crush stenting, followed by T and V-stenting. The number of treated vessels was significantly higher in the CABG group (1.6±0.9 vs. 2.4±0.9, respectively; p<0.01).
FOLLOW-UP CLINICAL OUTCOMES
Short-term and long-term clinical outcomes of patients receiving DES versus CABG are summarised in Table 3. The in-hospital incidence of death, TLR, TVR and CVA did not differ between the two groups. In-hospital MACCE was significantly higher in the CABG group (7.7% vs. 31.7%, p<0.01), mainly driven by the higher incidence of periprocedural MI. Mean±SD/median (IQR) follow-up was 1,088±644/1,191 (478-1,575) days. At long-term follow-up, the incidence of death, MI and CVA did not differ between the two groups, but the incidence of TLR, TVR and MACCE was significantly higher in the PCI group (31.9% vs. 21.6%, p<0.01). Adjusted curves derived from Cox survival analysis are displayed in Figure 1. Freedom from death and the composite endpoint of death, MI and CVA was similar in the two treatment groups. Conversely, the incidence of TVR and MACCE was significantly higher in the PCI compared to the CABG group (20.6% vs 4.6%; p<0.001 and 35.3% vs. 18.1%; p<0.001).
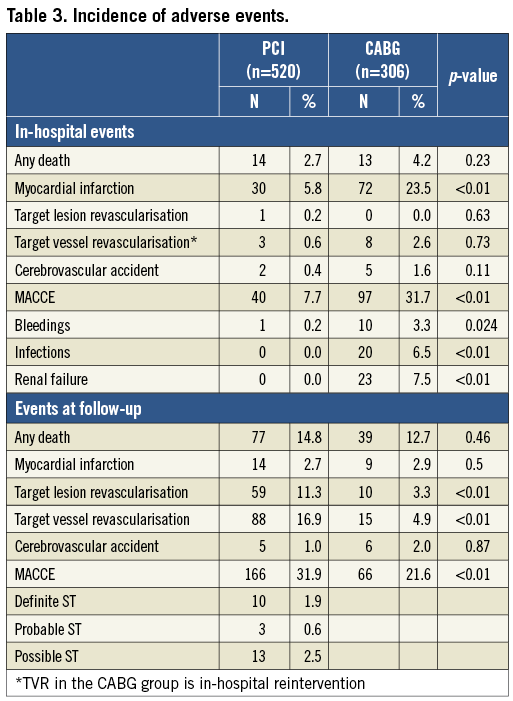
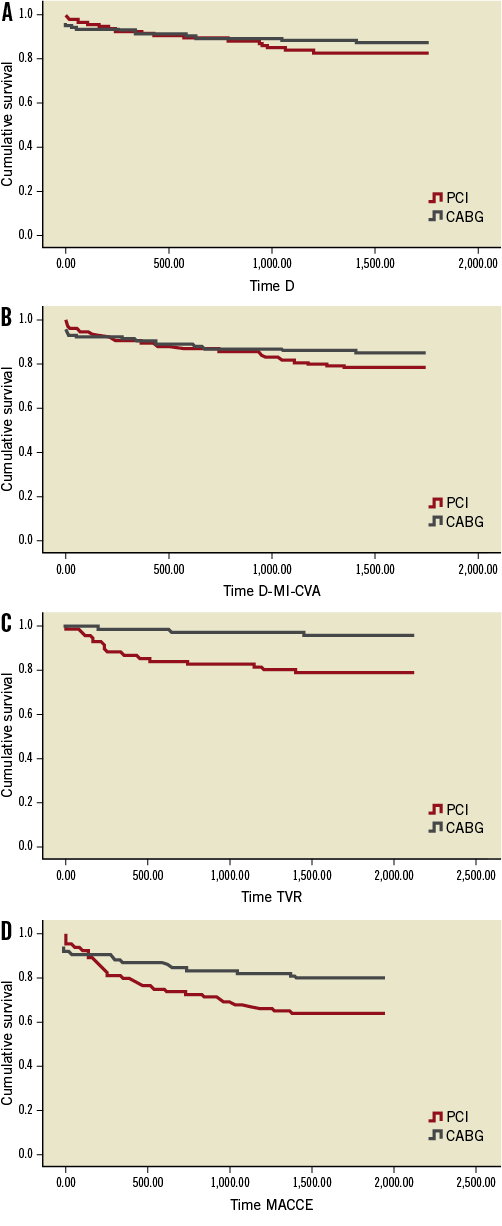
Figure 1. Freedom from death, D-MI-CVA, TVR and MACCE at mean of covariates. A) Freedom from death: CABG group 87.4%, PCI group 82.5%, p=0.124. B) Freedom from death, MI and CVA (D-MI-CVA): CABG group 85.4 %, PCI group 78.9%, p=0.11. C) Freedom from TVR: CABG group 95.4%, PCI group 79.4%, p<0.001. D) Freedom from MACCE: CABG group 81.9%, PCI group 64.7%, p<0.001.
Discussion
The main findings of the present study are the following: 1) no difference was found at four-year follow-up in the occurrence of death, MI, and CVA between PCI with DES implantation and CABG for ULMCA disease in diabetic patients; 2) there was an advantage of CABG over PCI in terms of MACCE, mainly driven by the lower incidence of TVR in the CABG group.
Diabetes mellitus plays a major role in the development and progression of coronary artery disease. The enhanced inflammatory response, endothelial dysfunction, increased plaque burden and altered coagulation processes have been found to be major determinants of the increased severity of CAD and poor clinical outcomes in patients with multivessel CAD16-18. The introduction of DES has dramatically broadened the indications for PCI and shifted the treatment of angiographic complex disease away from CABG. Results coming from recent large-scale randomised controlled studies and registries comparing DES with CABG in patients with diabetes are reassuring since they show similar outcomes for hard endpoints such as death, MI, or stroke, at short-term and midterm follow-up (FU) between the two strategies6,19,20. On the other hand, the results of DES use in this particular subset of patients at long-term FU are still inadequate and most of the studies currently available steadily report higher incidences of TVR and MACCE in patients treated with PCI, though with the use of first-generation DES4-9. In this context, the choice of revascularisation strategy is tricky and never unequivocal. Our results, derived from the observation of a large population with long and complete FU, seem to reinforce the concept that the two treatments differ primarily in the need for repeat revascularisation. This gap is partially explained by the fact that CABG is not associated with stent restenosis and stent thrombosis, and that arterial and venous grafts have been shown to have a “protective” effect on atherosclerotic progression21,22. Moreover, progressive atherosclerosis, which is responsible for repeat revascularisation in a significant number of diabetic patients23, occurs within the proximal 6 cm of epicardial arteries, the coronary artery segment that is usually bypassed by a graft24. Regarding technical aspects, the low use of IVUS (28.7%) and the consequent use of post-dilation (69.2%) may have had a negative effect on clinical outcomes. Recent reports have shown that IVUS-guided stent implantation is significantly related to a reduction of adverse events at follow-up25 and that it should be considered as mandatory when the left main is involved. Although the “aggressiveness” of CAD in diabetic patients is indisputable, the relatively high incidence of MACCE in the PCI population could also be a matter of definitions. In fact, it is worth noting that, in the context of LMCA disease, the TVR definition comprises the whole left coronary system, and therefore the likelihood of a reintervention due to a new lesion is much higher in this subset when compared to populations with multivessel disease. Also, the graft occlusion rate might be inaccurate due to the lack of routine angiographic FU in patients who underwent CABG.
Limitations
Despite the use of propensity scores to adjust for the differences in baseline clinical and lesion characteristics between the two study groups, the choice of treatment modality was an intrinsic limitation due to the observational nature of this study. Since our results are mainly derived from a subgroup analysis, they should be considered as exploratory in nature and hypothesis-generating. Adverse clinical events were adjudicated by investigators and not by an independent and centralised clinical events committee. Also, it was not possible to calculate the rate of symptomatic graft occlusion in the CABG group.
We acknowledge that in our registry the proportion of patients undergoing PCI is double that of those undergoing CABG. This phenomenon might reflect the practice of selected high-volume tertiary centres, such as the ones included in this study.
Conclusions
In this observational study, diabetic patients with ULMCA with/without concomitant multivessel disease treated with PCI had similar rates of death, MI and cerebrovascular accidents but a higher rate of MACCE compared to CABG, due to the significantly higher incidence of reinterventions. While a PCI strategy may be appropriate in selected patients, it should be performed in a setting where the risk/benefit ratio of both approaches has been carefully considered.
Conflict of interest statement
The authors have no conflicts of interest to declare.

