Abstract
Aims: We performed a meta-analysis of randomised trials comparing percutaneous coronary intervention (PCI) with stent implantation to coronary artery bypass grafting (CABG) for the treatment of unprotected left main coronary artery stenosis (ULMCA).
Methods and results: Pubmed and other databases were searched. Data were expressed as odds ratios (OR) with 95% confidence interval (CI). Four randomised trials enrolling 1,611 patients were selected. At 12-month follow-up PCI, as compared to CABG, was associated with a significant risk reduction of stroke (0.12% vs. 1.90%, OR 0.14, 95% CI [0.04 to 0.55], p=0.004), with an increased risk of repeat revascularisation (11.03% vs. 5.45%, OR 2.17, 95% CI [1.48 to 3.17], p <0.001), a similar risk of mortality (OR 0.72, 95% CI [0.42 to 1.24], p=0.23) or myocardial infarction (OR 0.97, 95% CI [0.54 to 1.74], p=0.91), leading to an increased risk of major adverse cardiovascular events (14.37% vs. 10.14%, OR 1.50, 95% CI [1.10 to 2.04], p=0.01) and similar hazard of major adverse cardiac or cerebrovascular events (14.49% vs. 12.04%, OR 1.24, 95% CI [0.93 to 1.67], p=0.15).
Conclusions: PCI is comparable to CABG for the treatment of ULMCA with respect to the composite of major adverse cardiovascular or cerebrovascular events at 12-month follow-up.
Introduction
Recent guidelines consider coronary artery bypass graft surgery (CABG) as the treatment of choice for unprotected left main coronary disease, although they recognise percutaneous coronary intervention (PCI) with stent implantation as a feasible therapeutic option.1,2 These recommendations have been implemented on the basis of registry studies3-9 and a few randomised controlled trials (RCT),10,11 the latter being either not powered in detecting the presence of a significant difference in individual clinical endpoints between PCI and CABG,10 or limited by their design, such as the subgroup analysis of the Synergy Between PCI With Taxus and Cardiac Surgery (SYNTAX) trial.11,12
In a recent large RCT, PCI with sirolimus-eluting stents was shown to be noninferior to CABG with respect to major adverse cardiac or cerebrovascular events.13 However, due to statistical reasons, this trial also could not provide clinically directive findings. Therefore, whether PCI offers clinical outcomes that are comparable to those after CABG remains controversial. A pooled analysis of RCT with greater power than that in the original trials, thus reducing sample size limitations of individual RCT, may provide clinically informative findings in this setting.
We therefore performed a meta-analysis of RCT to assess whether PCI is comparable to CABG with respect to clinical outcome for the treatment of unprotected left main coronary artery disease.
Methods
Data sources and search strategy
Two unblinded cardiologists (G.F., M.V.) independently searched Pubmed, EMBASE, the Cochrane Central Register of Controlled Trials, for all RCT that compared PCI vs. CABG for the treatment of left main coronary artery disease. The following keywords were entered “left main AND (angioplasty OR stent) AND coronary artery bypass graft AND (trial OR randomised OR randomised)”. Ongoing clinical trials and unpublished studies were also searched on the following Internet sites: http://www.controlled-trials.com, http://www.clinicaltrials.gov, http://www.centerwatch.com. Hand search of textbooks and references of papers selected was also performed. Disagreement was resolved by consensus.
Study selection
Studies were included if they met the following inclusion criteria: 1) randomisation between PCI with stent implantation and CABG; 2) unprotected left main coronary artery disease; 3) minimum length of follow-up of 12 months. Exclusion criteria were: a) lack of randomised design,; b) ongoing/unpublished studies; c) publication only as an abstract; d) a follow-up duration of less than 12 months.
Data extraction
Two unblinded reviewers (G.F., M.V.) independently extracted the data regarding the endpoints. Disagreement was resolved by consensus. The primary outcome was the composite of death, myocardial infarction (MI), repeat revascularisation, and stroke (i.e., major adverse cardiovascular or cerebrovascular events [MACCE]) at 12-month follow-up. Secondary endpoints were individual components of MACCE, and the composite of major adverse cardiovascular events (MACE) (i.e., death, MI, repeat revascularisation). The incidence of stent thrombosis and graft failure was reported when available. The number of events in each study were calculated from percentages when not directly reported. Specifically in the study by Boudriot et al,14 the number of strokes at 12 month follow-up was derived as: ([reported combined rate of death, MI, stroke – reported combined rate of death, MI]* number of patients)/100. The following data were also abstracted: follow-up duration; median SYNTAX Score value; rate of crossover from one treatment arm to the other.
The presence of selection, performance, attrition, detection and reporting bias was systematically addressed for each study, and classified as low, unclear, high, analysing the following domains according to the Cochrane Collaboration recommendations: adequate randomisation sequence generation; presence of allocation concealment and blinding; presence of incomplete outcome data; selective outcome reporting.15 Other sources of bias were eventually searched and reported. A risk of bias graph with judgements about each risk of bias item, presented as percentages across all included studies and a risk of bias summary reporting each risk of bias item for each included study were reported.15 The validity of the studies was evaluated according to the CONSORT statement and the meta-analysis was performed in agreement with the PRISMA statement.16,17
Data synthesis and data analysis
Data are expressed as odds ratio (OR) and 95% confidence interval (CI). Binary outcomes were combined with Mantel Haenszel method according to a fixed effect model or with DerSimonian and Laird method according to a random effect model if heterogeneity between studies was found.18 The number of patients needed to treat to benefit (NNTB) and the number needed to treat to harm (NNTH) were calculated from meta-analytical estimates of OR, using the macro “metannt”, as 1/(projected control group event rate –projected treatment group event rate). The corresponding 95% CI was calculated using 95% CI of the effect size applied to the control group event rate. The presence of heterogeneity among studies was evaluated with Cochran Q chi2 test, and I2 test was used to evaluate inconsistency. I2 describes the percentage of total variation across studies that is due to heterogeneity: values of 25%, 50% and 75% correspond to low, moderate, high I2.19 The presence of publication bias was investigated using the Peters’ test as this test has been shown to be associated with lower type I error rates and to be more appropriate than the Egger’s test and by visual estimation, with the use of a funnel plot of sample size against the treatment effect, displayed as OR.20,21 Sensitivity analyses calculating the individual and pooled estimates using a random effect model, and expressing treatment effect measures as risk ratios (RR), were performed. NNTB and NNTH were calculated from meta-analytical estimates of RR also. An additional analysis including MACCE available at the longest follow-up in each study was performed. The statistical level of significance for the summary treatment effect estimate was two tailed p <0.05. STATA 11.1 statistical software (StataCorp LP, College Station, TX USA) and Revman 5.1. were used for statistical analyses.
Results
Search results
A total of 189 potentially relevant citations were retrieved after database search. The study selection process is shown in Figure 1. One hundred and sixty-two papers were excluded after reading the corresponding title or abstract due to lack of relevance to the topic addressed or clear absence of randomisation design of the study. Therefore, 27 relevant citations were selected. Of these, meta-analyses and studies lacking a randomised design were excluded, yielding to five papers to be considered for final inclusion.10,11,13,14,22 Among these, the study by Cohen et al22 was excluded as this was a substudy of the SYNTAX trial, focusing on the comparison of PCI versus CABG with respect to patient quality-of-life. Therefore, a total of four RCT were included in the final analysis.10,11,13,14
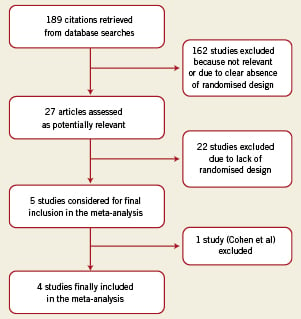
Figure 1. Algorithm for the selection of the studies included in the meta-analysis.
Study characteristics and bias assessment
The four trials selected in this meta-analysis included a total of 1,611 patients. Main clinical and angiographic characteristics of included studies are reported in Table 1. Follow-up was available until 12 months in all trials including a total of 1,596 patients, of whom 807 patients were randomised to PCI and 789 to CABG. The study by Park et al13 provided follow-up until 24 months, while in another study follow-up was 28 months.10 PCI was performed with drug eluting stent implantation in all studies, except in the study by Buszman et al10 where bare metal stents were employed in the majority of patients.
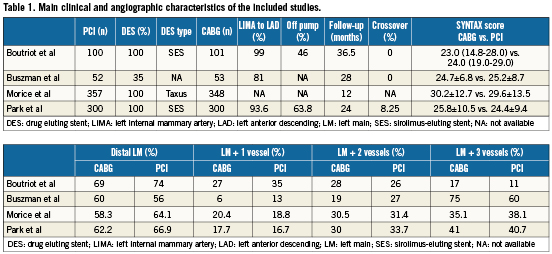
The assessment of bias according to Cochrane collaboration recommendations, both at outcome or study levels is reported in Figures 2 and 3. Overall, there was a high prevalence of low bias across most domains, except for blinding, across the studies. However the study by Buszman et al presented a higher prevalence of unclear bias.10
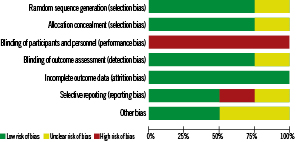
Figure 2. Risk of bias graph: judgements about each risk of bias item presented as percentages across all included studies.
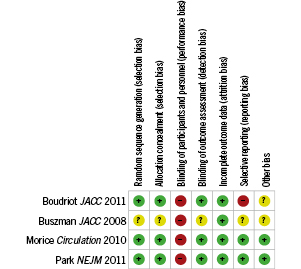
Figure 3. Risk of bias summary: judgements about each risk of bias item for each included study.
Outcome
Main analysis
No heterogeneity was detected for each endpoint assessed (chi-square test=2.00, p=0.57, I2=0 for mortality; chi-square test=1.05, p=0.79, I2=0, for MI; chi-square test= 1.55, p=0.67, I2=0 for repeat revascularisation; chi-square test= 0.22, p=0.97, I2=0 for stroke; chi-square test=0.09, p=0.99 , I2=0 for MACE; chi-square test=0.15, p=0.98, I2=0 for MACCE). Evidence of publication bias was present for the endpoint of mortality and of repeat revascularisation, but not for other endpoints (Supplementary appendix Table 2, Figures 4-9). At 12-month follow-up, no significant differences in mortality were found (2.97% mortality rate in the PCI group vs. 4.06% in the CABG group, OR 0.72, 95% CI [0.42 to 1.24], p=0.23), and the risk of MI was similar in the groups (MI rate 2.85% in the PCI group vs. 2.91% in the CABG group, OR 0.97, 95% CI [0.54 to 1.74], p=0.91) (Figures 10 and 11). PCI, as compared to CABG, was associated with an increased risk of repeat revascularisation (event rate 11.03% in the PCI group vs. 5.45% in the CABG group, OR 2.17, 95% CI [1.48 to 3.17], p <0.001; NNTH 18, 95% CI 10 to 41) and with a significant risk reduction of stroke (stroke rate 0.12% in the PCI group vs. 1.90% in the CABG group, OR 0.14, 95% CI [0.04 to 0.55], p=0.004, NNTB 62, 95% CI 55 to 118) (Figures 12 and 13). As a result, the risk of MACE was significantly higher in the PCI group (MACE rate 14.37% in the PCI group vs. 10.14% in the CABG group, OR 1.50, 95% CI [1.10 to 2.04], p=0.01; NNTH 23, 95% CI 12 to 106) (Figure 14), while the risk of MACCE was not significantly different between the groups (MACCE rate 14.49% in the PCI group vs. 12.04% in the CABG group, OR 1.24, 95% CI [0.93 to 1.67], p=0.15) (Figure 15).
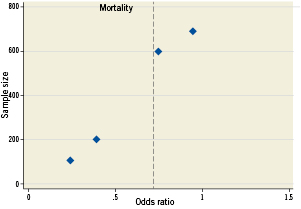
Figure 4. Funnel plot of sample size against odds ratio for the endpoint of mortality,
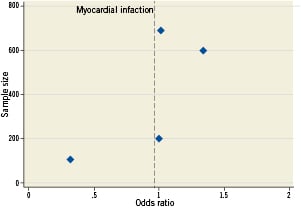
Figure 5. Funnel plot of sample size against odds ratio for the endpoint of myocardial infarction.
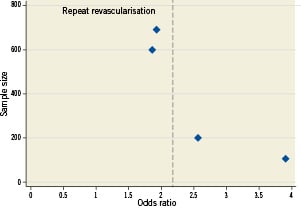
Figure 6. Funnel plot of sample size against odds ratio for the endpoint of repeat revascularisation.
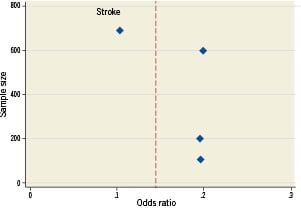
Figure 7. Funnel plot of sample size against odds ratio for the endpoint of stroke.
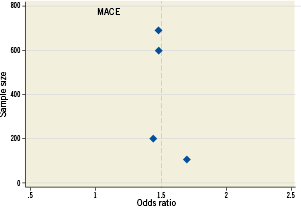
Figure 8. Funnel plot of sample size against odds ratio for the endpoint of major adverse cardiovascular events (MACE).
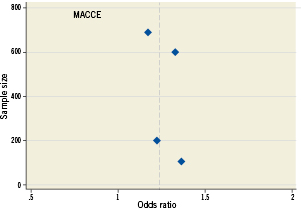
Figure 9. Funnel plot of sample size against odds ratio for the endpoint of major adverse cardiovascular or cerebrovascular events (MACCE).
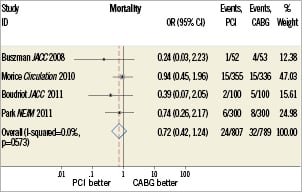
Figure 10. Forest plot shows summary treatment effect expressed as odds ratio (OR) with 95% confidence interval (CI) for the comparison of PCI versus CABG for the endpoint of mortality.
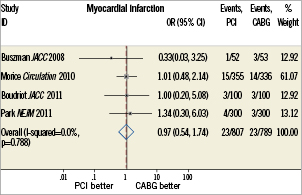
Figure 11. Forest plot shows summary treatment effect expressed as odds ratio (OR) with 95% confidence interval (CI) for the comparison of PCI versus CABG for the endpoint of myocardial infarction.
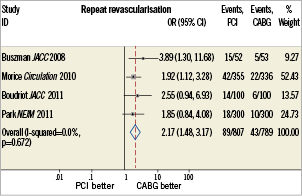
Figure 12. Forest plot shows summary treatment effect expressed as odds ratio (OR) with 95% confidence interval (CI) for the comparison of PCI versus CABG for the endpoint of repeat revascularisation.
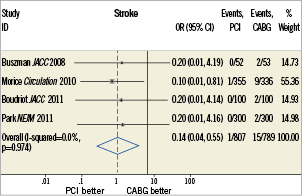
Figure 13. Forest plot shows summary treatment effect expressed as odds ratio (OR) with 95% confidence interval (CI) for the comparison of PCI versus CABG for the endpoint of stroke.
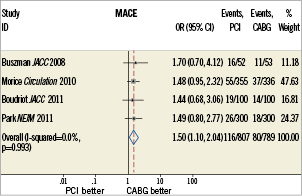
Figure 14. Forest plot shows summary treatment effect expressed as odds ratio (OR) with 95% confidence interval (CI) for the comparison of PCI versus CABG for the endpoint of major adverse cardiovascular events (MACE).
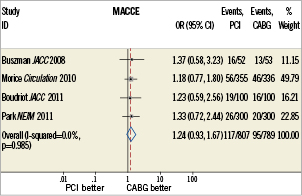
Figure 15. Forest plot shows summary treatment effect expressed as odds ratio (OR) with 95% confidence interval (CI) for the comparison of PCI versus CABG for the endpoint of major adverse cardiovascular or cerebrovascular events (MACCE).
The rate of graft occlusion was not reported in two studies,10,14 therefore the comparison between PCI and CABG with respect to stent thrombosis/graft occlusion was not performed. Of note, no stent thrombosis occurred in three studies,10,13,14 10 stent thrombi and 10 graft occlusions were reported in one study,11 three graft occlusions in the study by Park et al.13
Sensitivity analyses
The use of RR as a measure of treatment effect yielded similar results to those calculated as OR.
Summary RR and OR calculated with a random effect model were similar to those obtained using a fixed effect model. NNTB and NNTH calculated from meta-analytical estimates of RR were similar to those obtained from meta-analytical estimates of OR. (Supplementary Appendix, Tables 3-6).
Long-term follow-up
In a meta-analysis that included MACCE available at a follow-up longer >12 months from two studies (24 months in the study by Park et al,13 28 months in the study by Buszman et al10) the comparison of PCI with CABG with respect to MACCE yielded similar results to those reported in our main analysis at one year follow-up. No heterogeneity or publication bias were detected (Supplementary Appendix, Tables 7-9).
Discussion
The main findings of this meta-analysis of randomised trials are as follows: 1) PCI, as compared to CABG, is associated with a similar risk of the primary composite endpoint of MACCE at 12 month follow-up; 2) PCI is associated with a significant reduction of the risk of stroke; 3) PCI increases significantly the risk of repeat revascularisation, while it is associated with a similar risk of mortality or MI, resulting in a significant increase of the risk of the composite MACE.
The subgroup analysis of the randomised SYNTAX trial involving patients with left main coronary artery disease11 and the PRECOMBAT trial13 have reported the noninferiority of PCI in comparison to CABG with respect to MACCE at 12-month follow-up. Significant differences in MACCE rates were present between these two studies: 8.7% and 6.7% in the PCI and CABG arms, respectively, in the PRECOMBAT trial13, vs. 15.8% and 13.7% in the SYNTAX substudy.11 Large differences in patient and procedural trial characteristics, such as the presence of lower mean SYNTAX score and EuroSCORE values in the PRECOMBAT trial, the use of sirolimus-eluting stents vs. paclitaxel-eluting stents in the SYNTAX substudy,11 a higher usage of off-pump CABG in the PRECOMBAT trial,13 as well as ethnic differences in the study population may explain these findings.
The lack of significant MACCE differences was already observed in the LE MANS study,10 the first, albeit small, randomised trial comparing PCI vs. CABG for the treatment of unprotected left main coronary artery disease, that however reported even higher rates of MACCE at 12-month follow-up, in both the PCI (30.7%) and CABG (24.5%) arms. Such high event rates are likely to reflect the lower prevalence of drug-eluting stent use and of arterial conduits to the left anterior descending artery, despite the presence of high risk characteristics of the study population, that presented high mean SYNTAX score and EuroSCORE values, and high prevalence of triple vessel disease. In these randomised trials,10,11,13 patients undergoing PCI had similar or even numerically lower rates of mortality and of MI at 12-month follow-up compared to those undergoing CABG, while experiencing an increase of repeat revascularisation. No stroke occurred in the PCI arm in three RCTs,10,13,14 however, differences in stroke rate between the PCI and CABG groups were not statistically significant due to the small sample size and low event rates, whereas in the SYNTAX substudy,11 PCI as compared to CABG, yielded a significant reduction of stroke. In the recent study by Boudriot et al,14 PCI with sirolimus-eluting stents was inferior to CABG with respect to MACE at 12-month follow-up, mainly due to repeat revascularisation, while PCI resulted to be noninferior in terms of death or MI.
In our meta-analysis, the similar risk of MACCE in the PCI and CABG groups was the result of numerically lower rates of mortality and similar rates of MI, significant higher rates of repeat revascularisation and significant lower rates of stroke in the PCI arm as compared to the CABG arm.
Although the point estimate of the number needed to treat for repeat revascularisation or for the composite MACE was lower than that for stroke, the assessment of net clinical benefit of the most appropriate revascularisation strategy should balance the clinical impact and consequences of increasing or reducing repeat revascularisation versus stroke. Stroke has been reported to be associated with frequent disabling clinical sequelae.23 In our meta-analysis, the increased rate of repeat revascularisation observed in the PCI arm was not paralleled by a concomitant excess of mortality or MI, suggesting that the former does not carry a major negative impact on hard endpoints. Some studies have shown that the clinical cost of stent thrombosis may be more severe than that after graft occlusion.24-27 We could not assess whether the risk of stent thrombosis after PCI is higher than that for graft occlusion due to lack of data reporting on graft occlusion in two trials.10,14 However, no stent thrombosis was reported in three out of four studies,10,13,14 and in the remaining study, the same number of stent thrombi and graft occlusions occurred.11 Although our meta-analysis could not address the impact of repeat revascularisation on patient quality-of-life, a recent subgroup analysis of the SYNTAX trial assessing health-related quality of life has shown that both PCI and CABG led to significant improvements in disease-specific and general health status over the course of 12 months.22 PCI was associated with large benefits in general health-related quality-of-life as assessed by the Medical Outcomes Study 36-Item Short-Form Health Survey at 1 month, however, differences largely disappeared by six months.22 CABG instead was associated with a slightly greater improvement in the score on the Seattle Angina Questionnaire angina frequency subscale at six and 12 month follow-up, with no differences in the scores at these later time points. Therefore, the higher risk of stroke after CABG in our meta-analysis remains an important factor affecting the choice of the most appropriate revascularisation mode for unprotected left main coronary artery disease.
Study limitations
We acknowledge several limitations. The study by Morice et al11 is a subgroup analysis of the randomised SYNTAX trial, that although pre-specified and adequately powered for the detection of differences in the composite clinical endpoint, could provide only hypothesis-generating findings, due to the lack of demonstration of noninferiority between PCI and CABG with respect to the primary endpoint of the SYNTAX trial. Further, about one third of patients did not meet the criteria for significant left main disease by study definition.28 We could not calculate the summary treatment effect estimates for stent thrombosis/graft occlusion, due to the lack of information on graft occlusion in two studies.10,14 Although we did not detect the presence of statistically significant heterogeneity, intrinsic differences across trials are present, such as the sample size of study population, the number of recruiting sites (i.e., 85 sites in 17 countries in Europe and United States in the SYNTAX substudy,11 13 sites in Korea in the PRECOMBAT trial13), the use of different types of stent or techniques, the number of diseased vessels. We did not perform an individual patient data meta-analysis. Therefore, we could not assess the impact of the SYNTAX score or of other clinical, angiographic and procedural characteristics on the comparison between PCI and CABG. Our findings may not be generalisable to all patients with unprotected left main coronary artery disease, as in RCT, usually patients with unfavourable anatomy for PCI or excessive surgical risk are excluded, while these are encountered in real world situations. Further, these trials have been performed in highly specialised centres with experienced operators. Our main analysis reflects the first year of follow-up after revascularisation; longer follow-up is warranted to assess whether 1-year findings will be confirmed.
Conclusions
In this meta-analysis of RCT, PCI, as compared to CABG, was associated with a similar hazard of the composite MACCE at 12-month follow-up. This finding stems from a significant reduction of stroke that counterbalances the detrimental increase in repeat revascularisation after PCI.
Conflict of interest statement
All authors have no conflict of interest to declare in relation to this paper.