Abstract
Aims: Many operators are discouraged from attempting percutaneous coronary intervention (PCI) of the left main coronary artery in the presence of a right coronary artery (RCA) stenosis, due to the perceived increased risk of periprocedural complications and poor clinical outcome at follow-up. The aim of this study was to asses if the impact of PCI on the clinical outcome of left main patients differed significantly relative to the presence of RCA disease.
Methods and results: A total of 255 consecutive patients undergoing PCI of the left main coronary artery were analysed. Patients were subdivided into “RCA disease” (n=113) and “no RCA disease” (n=142) groups. In the RCA disease group, 33 (29.2%) patients had a chronic total occlusion (CTO). The primary endpoint was the incidence of cardiac death at 3-year follow-up. Patients with RCA disease showed a higher rate of cardiac death (17.7%) compared with those without (6.7%, p=0.056). Patients with a CTO in the RCA had a significantly higher cardiac mortality (30.0%) compared with patients without RCA disease (6.7%, p=0.015) and patients without RCA disease or a >50-99% RCA stenosis combined (8.8%, p=0.021). The presence of residual RCA disease significantly predicted the occurrence of cardiac death (HR 4.41, 95% CI 1.55-12.51, p=0.005).
Conclusions: Patients with unprotected left main disease treated with PCI have worse outcome in terms of cardiac mortality when the RCA is diseased, especially when a CTO is present.
Introduction
The introduction of drug-eluting stents into clinical practice has prompted percutaneous coronary intervention (PCI) of unprotected left main1. Several reports have shown that this strategy represents a feasible, safe and, effective option of treatment for this high risk lesion subset2-8.
The SYNTAX (SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery) trial has recently suggested that PCI is associated with similar outcomes compared with coronary artery bypass grafting (CABG) in patients with a low burden of coronary artery disease (e.g., low or intermediate SYNTAX score)2. As the extent of coronary disease progresses, surgery is likely to be considered the best option of revascularisation2,9. However, many operators are still discouraged from attempting left main PCI in patients with a right coronary artery (RCA) stenosis, due to the perceived increased risk of periprocedural complications and poor clinical outcome at follow-up.
To address whether this concern is really justified in contemporary daily practice, we performed a clinical follow up investigation of all patients who underwent PCI of unprotected left main in our Institution. Specific aim was to test if the effects of PCI on in hospital and long-term clinical outcome of left main patients differed significantly relative to the presence of RCA disease.
Methods
Patient population
Consecutive patients undergoing PCI with either a sirolimus- (Cypher, Cordis, a Johnson and Johnson Company, Miami Lakes, FL, USA) or paclitaxel- (Taxus, Boston Scientific, Natick, MA, USA) eluting stent in an unprotected left main coronary artery from January 2003 to June 2008 were retrospectively evaluated in this single centre study. An unprotected left main coronary artery was defined as having no patent coronary artery bypass grafts to the left anterior descending artery or left circumflex artery. Patients were subdivided into “RCA disease” and “no RCA disease” subgroups according to the presence or absence of a ≥50% stenosis in the RCA by quantitative coronary angiography, respectively. All patients were fully informed about the possible procedure-related risks and the alternative treatment options, and written informed consent was obtained. Stent implantation was performed according to standard techniques and the final interventional strategy, as well as the use of intravascular ultrasound, was left entirely to the operator’s discretion. Lesions located at the ostium or shaft were treated with a single stent. Bifurcation lesions were treated by using one of the following strategies at the operator’s discretion: provisional T-stenting, T-stenting, V-stenting or mini-crush stenting.
Unfractionated heparin (75 IU/kg bolus) was administered before coronary intervention with the goal to achieve an activated clotting time >250 seconds. Glycoprotein IIb/IIIa inhibitors were administered at the operator’s discretion. All patients undergoing PCI were on aspirin, which was maintained indefinitely. Clopidogrel 75 mg/daily was recommended for 12 months.
Information concerning in-hospital events was obtained from centralised databases of our institution for those patients who stayed in hospital and from the hospital records or by telephone contacts for those transferred to another hospital after the procedure. The clinical follow-up data related to medications and clinical status were prospectively completed through scheduled outpatient clinic evaluations. Referring cardiologists, general practitioners and patients were contacted whenever necessary for further information. All repeated coronary intervention (surgical and percutaneous) and re-hospitalisation data were prospectively collected during follow-up using the centralised system of our institution or contacting directly the hospitals were the patients were admitted or referred.
Objectives and definitions
The primary objective was the incidence of cardiac death considered as any death with a demonstrable cardiovascular cause or any death that was not clearly attributable to a non-cardiovascular cause. We report the incidence of the primary objective both in-hospital and at long term follow-up.
Secondary objective was the incidence of major adverse cardiac events (MACE) defined and ranked as cardiac death, non-fatal myocardial infarction (MI) or target lesion revascularisation (TLR). Patients with more than one event were assigned the highest rank event. Periprocedural MI was defined as a rise in troponin or creatine kinase-MB > 3 times the upper normal limit. Subsequent MI was diagnosed in the presence of any elevation of troponin or creatine kinase-MB above the upper normal limit. TLR was defined as any repeat intervention (by CABG or PCI) performed to treat a stenosis inside the implanted stent or within the 5 mm segments adjacent to the stent, including the ostium of left anterior descending and/or left circumflex coronary arteries.
Statistical analysis
Continuous variables are presented as mean±standard deviations and compared using Student’s unpaired t test. Categorical variables are presented as counts and percentages and compared with the chi-square test or Fisher exact test, as appropriate. Survival curves were generated by the Kaplan-Meier method and the log-rank test was used to evaluate differences between groups. Patients lost to follow-up were considered at risk until the date of last contact, at which point they were censored.
To account for potential confounders when studying the impact of residual RCA disease on cardiac death, a Cox multivariable proportional hazard regression analysis was used. The assumption of the proportional hazard was verified by a visual examination of the log (minus log) curves and the linearity assumption was assessed by plotting the Martingale residuals against continuous covariates. The variables considered as possible predictors included age, gender, smoke, diabetes, acute coronary syndrome, renal dysfunction, left ventricular ejection fraction (LVEF), EuroSCORE, reference vessel diameter, lesion length, lesion location, emergent setting, chronic total occlusion, number of diseased vessels, complete revascularisation and SYNTAX score (SXscore) as independent control variables and residual RCA disease as the independent study variable of interest. The total SXscore was derived from the summation of the individual scorings for each separate lesion (defined as ≥50% stenosis in vessel ≥1.5 mm). Full details on SXscore calculation are reported elsewhere10. The selection of the variables in the final model was based on a plausible association with the primary objective or a significant p value on univariate analysis. We report crude and adjusted hazard ratios (HRs) and corresponding 95% confidence intervals (CIs). For all analyses a two-sided p < 0.05 was considered statistically significant. All data were processed using the statistical Package for Social Sciences, version 15 (SPSS, Chicago, IL, USA).
Results
Two hundred fifty-five patients were analysed, 113 with RCA disease and 142 without. In the RCA disease group, 33 (29.2%) patients had a chronic total occlusion (CTO). CTO were ostial in eight cases, proximal in 18 cases and mid-segment in seven cases. No significant clinical baseline differences were seen between groups except that patient with RCA disease had a lower likelihood of chronic renal failure than those without (Table 1).
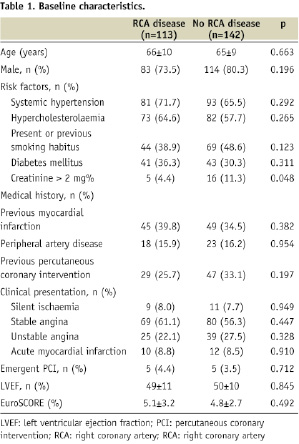
Based on procedural and angiographic characteristics, differences between patients with and those without RCA disease were more pronounced and noted in terms of a higher complexity in the former group (Table 2).
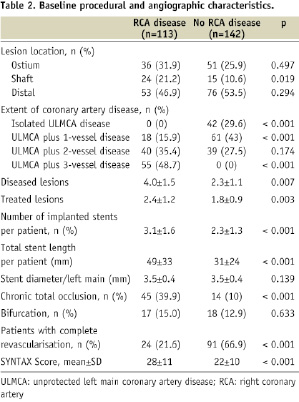
Patients without RCA disease had lower SXscore (22±10 vs. 28±11, p < 0.001) and a greater likelihood of complete revascularisation.
In-hospital and long-term outcome
The rates of cardiac death during hospitalisation were 2.7% and 0.7% in patients with and without RCA disease, respectively (p=0.213). MACE occurred in 3.5% of patients with RCA disease and 2.8% of patients without (p=0.742). Twenty patients (7.8%) were lost to follow-up. The other patients were followed up for a mean duration of 18 months (ranging three to 57 months based on the date of enrolment). In the Kaplan Meier analysis, patients with RCA disease showed a higher estimated rate of cardiac death (17.7%) at three years compared with patients without RCA disease (6.7%) (Figure 1). The presence of RCA disease was associated with a trend towards a higher risk of cardiac death (HR 2.66, 95% CI 0.94-7.55, p=0.056).
Conversely, MACE did not significantly varied different according to the presence or absence of RCA disease (26.6% vs. 23.8%, respectively; HR 1.13, 95% CI 0.62-2.07, p=0.695; Figure 1).
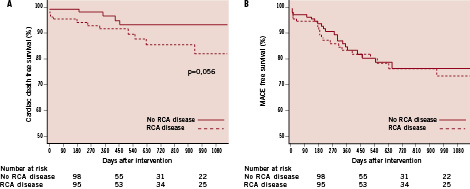
Figure 1. Survival free from cardiac death (A) and MACE (B) at three years among patients with no RCA disease or RCA disease at baseline. RCA: right coronary artery; MACE: major adverse cardiac events
Difference between early and late events
A landmark analysis separating early from intermediate and late clinical events is shown in Figure 2 for the primary objective.
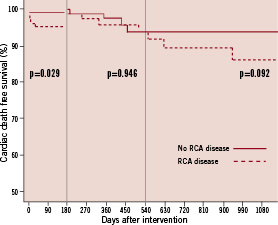
Figure 2. Three-year cumulative survival free from cardiac death subdivided into early, intermediate and late events. RCA: right coronary artery
Overall, there was an early significant better outcome in patients without RCA disease (p=0.029), which contrasted to no differences in the period beyond six months up to 18 months (p=0.946). After 18 months, the curves started to diverge due to a trend towards increased rates of late events in patients with RCA disease (p=0.092).
Impact of total RCA occlusion on clinical outcome
In-hospital cardiac mortality and MACE were almost equally distributed among patients with a totally occluded RCA (3.0% and 3.0%, respectively) and those with a >50-99% stenosis (2.5% and 3.8%, respectively).
At three years, patients with a RCA CTO had a significantly higher estimate of cardiac mortality (30.0%) compared with patients without RCA disease (6.7%, HR 4.35, 95% CI 1.32-14.26, p=0.015) and patients without RCA disease or a >50-99% RCA stenosis combined (8.8%, HR 3.24, 95% CI 1.20-8.77, p=0.021).
Impact of revascularisation on clinical outcome
To assess whether the effect of RCA disease on prognosis differed significantly after revascularisation, the entire cohort was stratified according to the presence (35.3%) or the absence (64.7%) of residual RCA disease. Among this latter group, 85.3% had no RCA disease at baseline and 14.7% achieved this result by means of a second angioplasty performed soon after the index procedure on the left main. No CTO revascularisation was attempted. Three-year clinical cardiac mortality distribution between groups is shown in Figure 3.
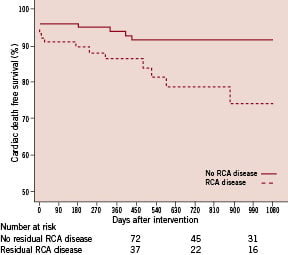
Figure 3. Cardiac death-free-survival at three years among patients with no residual RCA disease or residual RCA disease after left main angioplasty. RCA: right coronary artery
The presence of residual RCA disease significantly predicted the occurrence of cardiac death (HR 4.41, 95% CI 1.55-12.51, p=0.005).
After adjustment for potential confounders, the presence of residual RCA disease preserved a trend towards prediction of cardiac mortality (adjusted HR 5.19, 95% CI 0.83-32.5, p=0.078). The only significant predictor of outcome at multivariable analysis was SXscore (adjusted HR 1.11, 95% CI 0.20-1.68, p=0.001).
Discussion
Despite CABG being considered the gold standard for the treatment of left main coronary artery disease11, the introduction of DES has reopened the debate on the comparative efficacy between PCI and CABG for treating this subset of lesions8.
In patients with three-vessel and/or left main coronary artery disease who are eligible for both PCI or CABG either revascularisation strategy is associated with similar survival rates at 12 months, a greater need for repeat intervention in the PCI arm, and an excess of early morbidity (stroke) in the CABG arm2. While caution should be applied as the SYNTAX study was underpowered to identify differences surrounding the secondary endpoints, the results of the left main sub-analysis of the SYNTAX trial somewhat suggest that there are specific subgroups of patients (e.g., those with low or intermediate SYNTAX score) who can receive PCI as a reasonable alternative to conventional surgery12.
The occurrence of left main disease associated with an obstructed RCA is historically considered a life threatening finding13, which casts some concerns about the use of stent as the best choice for the treatment and urges many interventionalists to submit patients to surgery even when the angiographic characteristics of coronary artery disease are not particularly challenging and easily manageable by PCI. In this setting, CABG has been associated with a mortality rate comparable with that of patients with left main stenosis alone and a significantly better survival than that of similar patients treated medically14. The Coronary Artery Surgery Study (CASS) investigators provided evidence that although concomitant RCA disease may affect intermediate-term mortality, this issue abated over time15, with a median survival of 12.7 years in the surgical group and 5.6 years in the medical therapy group (p < 0.0001).
This is, at the best of our knowledge, the first study specifically set up to obtain some insights into the performance of PCI in this context. Our main findings suggest that 1) the presence of a concomitant RCA disease affects the prognosis of patients undergoing left main PCI. The magnitude of this side effect is bigger when RCA is chronically occluded; 2) revascularisation of RCA could be an aim to be purposely sought after left main angioplasty, when technically feasible and clinically appropriated. These statements are mainly based on the following observations.
First, technical concerns associated with left main angioplasty in the context of a concurrent RCA disease could seem justified by a slightly higher rate of in-hospital cardiac mortality compared to patients with no RCA disease (2.7% vs. 0.7%). However, both these rates are reasonably low and consistent with those reported in other contemporary studies14,16. Importantly, the presence of a CTO in the RCA is not associated with a noticeable increase of periprocedural mortality compared with the presence of a sub occlusive stenosis in the same vessel (3.0% vs. 2.5%).
Second, at follow up, the gap between patients with RCA disease and those without gets wider showing a trend towards lower survival rates in the former. Obviously, this study is underpowered to detect a difference in clinical endpoints, but it is very likely that a larger number of patients could enhance the statistical significance of this finding.
Third, a landmark analysis supports the understanding that patients with RCA disease experience worse outcome than those without especially early and late after left main angioplasty, while in the intermediate stage between 6 and 18 months this condition seems less influential. A possible explanation for this finding might be related to the different distribution of the adverse events in the different subgroups. In fact, in patients with a RCA CTO, cardiac mortality was uniformly distributed along the entire length of follow up, consistently with previous data15. Conversely, in patients without a CTO the cluster of deaths was particularly concentrated during the first 18 months in patients with a >50-99% stenosis and between six and 18 months in patients without RCA disease. These data in aggregate suggest that early mortality is affected by both types of RCA disease, whereas late mortality may be more specifically related to the presence of a CTO. This is also in agreement with the observation that the presence of a CTO in the RCA in this series was associated with a 4-fold increased risk of 3-year mortality compared to patients without RCA disease and a 3-fold increased risk in patients with no RCA disease or a >50-99% stenosis combined.
Fourth, the prognosis of patients with RCA disease has the potential to change by pursuing the goal of RCA revascularisation. Although consistent with previous evidences showing that complete revascularisation with drug eluting stents of multivessel disease patients is associated with lower rates of long term adverse events17, this finding must be interpreted with caution, because only 14.7% of the patients in the group with no residual RCA disease underwent active revascularisation. This study demonstrates that patients with RCA disease have an almost 3-fold increased risk of cardiac mortality than those without. However, when patients undergone to RCA revascularisation by PCI are shifted in the group of patients with no RCA disease, the presence of a residual RCA disease indicates a 4-fold increased risk of cardiac mortality than the absence of RCA disease or the presence of any lesion treated with stents. Of note, the association of residual RCA disease with a poor prognosis remained strong, although not significant due to a lack of statistical power, even after adjustment for potential confounders, including baseline, angiographic and procedural characteristics. In this context, the SYNTAX score emerged as the only significant predictor of outcome, reflecting the learning that the extent of coronary artery narrowing is a primary determinant of survival in patients with coronary artery disease18,19. The notion of worse outcomes in patients with residual RCA disease must be viewed with the understanding that these patients had greater coronary disease burden. Therefore, the possibility that residual RCA disease might simply be a marker of a subgroup with more coronary disease overall should not be excluded.
Fifth, patients undergoing left main angioplasty seem to benefit from PCI of concurrent RCA disease, but the presence of a CTO deserves more caution. In our series, no attempt to recanalise a CTO in these patients was performed. One may hypothesise that even these patients could benefit from a RCA revascularisation. Actually, the absence of a “honeymoon” window free from cardiac events, in which left main revascularisation could be followed by CTO recanalisation, does not encourage the performance of a long and complex procedure. Conversely, at the best of our knowledge, there are no data supporting CABG for patients with totally occluded RCA in addition to left main disease. However, it was demonstrated that successful recanalisation of CTO confers a long-term survival benefit20. A further discussion and specifically designed studies are demanded in order to verify the true impact of CTO revascularisation in patients with a prior left main PCI.
Finally, although the study findings are generally consistent in suggesting that patients with RCA disease in addition to a left main stenosis experience worse outcomes at long term compared with those with left main stenosis alone, whether the purpose of RCA revascularisation should be pursued by PCI or CABG in patients undergoing LM PCI is currently undefined. Given the detrimental effect of RCA disease on prognosis, it seems intuitive that patients in whom RCA disease cannot be treated by PCI should be entirely managed with CABG even in case of a left main stenosis easily manageable by means of a percutaneous approach. When technically feasible, left main and RCA revascularisation by PCI could represent an option, when pursued by highly experienced interventional cardiologists. A multidisciplinary team approach involving both cardiologists and heart surgeons is key in selecting the ideal revascularisation strategy for each patient.
Limitations
This study carries the obvious limitations of each observational study on current clinical practice. Evaluating the impact of a specific treatment using a registry can lead to incorrect conclusions due to the influence of unassessed confounding variables. In this study, the choice of treating the RCA was assigned not randomly but by specific criteria in each case, generating an unavoidable risk of bias regarding treatment selection and the possible prognosis. In order to partly compensate for the baseline and angiographic imbalance between groups with or without residual RCA, we performed adjustments with multivariate analysis, making residual selection biases unlikely. However, it is impossible to know if these adjustments are appropriate or if the relevant characteristics have been correctly identified, since only randomisation can provide an unbiased estimation of the effects of a treatment. In addition, from a statistical standpoint, the potential for over fitting of the model may not be excluded, since the selection of the variables was based on clinical judgment and univariate analysis. Other caveats are the irregular and short follow up and the fact that the evidence regarding the benefit of RCA-revascularisation is quite indirect, tangential, and should be cautiously interpreted. We also recognise that numerous data are missing from this registry with regards to factors known to affect cardiovascular survival including usage of cardio active medications (i.e., beta-blockers, statins, ACE inhibitors).
Conclusion
Patients with unprotected left main coronary artery disease treated with stent-supported PCI might have long term worse outcome in terms of cardiac mortality when the RCA is diseased, especially in presence of a CTO. The difference in outcome becomes more prominent and statistically significant when comparing the presence of residual RCA disease versus no residual RCA disease, pointing out an eventual benefit of pursuing RCA revascularisation.
Acknowledgement
The authors would like to acknowledge in this paper the Associazione Cuore e Ricerca, Catania, Italy.

