Abstract
Background: Calcified nodules (CN) have been reported as being associated with stent failure including in-stent restenosis (ISR). However, there is no systematic study of this condition.
Aims: We aimed to clarify the prevalence, predictors, and midterm results of ISR lesions with CN.
Methods: We examined the clinical characteristics of 651 ISR lesions in patients who underwent percutaneous coronary intervention (PCI) with optical coherence tomography (OCT) between October 2008 and July 2016, and their 6- to 8-month follow-up angiography results. CN was defined as a high backscattering mass with small nodular calcium depositions which protruded into the vessel lumen.
Results: Thirty-two ISR lesions (4.9%) had CN. Multivariable analysis showed that calcified lesion (odds ratio [OR] 12.441, p<0.001), incomplete stent apposition (OR 3.228, p=0.005), haemodialysis (OR 3.633, p=0.024), and female gender (OR 3.212, p=0.036) were independently associated with ISR lesions with CN. Midterm follow-up was performed on 612 ISR lesions. Both ISR and target lesion revascularisation (TLR) rates were significantly higher in lesions with CN compared with those without CN (43.8% vs 25.0%, p=0.023; 37.5% vs 18.8%, p=0.020, respectively). However, multivariate analysis did not show the presence of CN as an independent predictor of re-TLR (OR 1.690, p=0.286).
Conclusions: The prevalence of ISR lesions with CN was 4.9%. Calcified lesions, incomplete stent apposition, haemodialysis, and female gender are probably associated with CN formation. ISR lesions with CN may have poor midterm outcomes compared with ISR lesions without CN.
Introduction
Calcified nodules (CN) have been shown to be one of the causes of acute coronary syndrome (ACS)12. CN can be detected with optical coherence tomography (OCT) or optical frequency domain imaging (OFDI) in patients with ACS and in those with stable angina pectoris345678. Based on OCT investigations, Lee et al reported that 4.2% of de novo culprit lesions had CN3. Histopathological data have suggested that CN consist of nodular calcification and fibrin deposition78. Additionally, CN have been reported to be associated with stent failure, including in-stent restenosis (ISR) and stent thrombosis910111213. Alfonso et al reported that a CN was observed in an ISR lesion two years after drug-eluting stent (DES) implantation10. Mori et al reported two cases of CN which caused in-stent failure11. In their study, histological data showed that CN consisted of nodular calcification and fibrin deposition. As mentioned above, there are some case reports of ISR lesions with CN. However, there is no systematic study of this condition.
The aim of this study was to clarify the prevalence and predictors of ISR lesions with CN using OCT and examine the results of their 6- to 8-month (midterm) follow-up coronary angiography (CAG) after repeat percutaneous coronary intervention (PCI).
Methods
Study design and patient population
This was a single-centre, retrospective observational study conducted at Kurashiki Central Hospital, Kurashiki, Japan. The study was approved by the Institutional Ethics Committee of the Kurashiki Central Hospital. The risks of PCI and follow-up CAG were explained to each patient, and written informed consent was obtained from all patients. Between May 2008 and July 2016, we tried to perform pre-PCI OCT/OFDI imaging in 720 ISR lesions with 482 patients. The OCT/OFDI catheter could not pass through the lesions before PCI in 41 lesions out of 720 ISR lesions; these lesions were excluded from the study. Furthermore, adequate imaging could not be acquired in 28 lesions owing to insufficient elimination of red blood cells. Thus, 651 lesions in 432 patients were included in the study. After assessment of lesion morphology with OCT, PCI was performed with the use of plain old balloon angioplasty (POBA) alone (86 lesions), POBA+paclitaxel-coated balloon (PCB) (381 lesions), POBA+DES (180 lesions), or POBA+bare metal stent (BMS) (4 lesions). Morphological assessment of neointimal tissue with OCT or OFDI, including the presence or absence of CN, was also performed. Follow-up angiography at 6 to 8 months after PCI was performed in 612 ISR lesions in 404 patients (follow-up rate 94.0%) with a breakdown of POBA alone (81 lesions), POBA+PCB (355 lesions), POBA+DES (172 lesions), and POBA+BMS (4 lesions). We examined the association between the presence of CN and midterm (6- to 8-month) results, including the ISR and target lesion revascularisation (TLR) rates. The study flow diagram is provided in Figure 1.
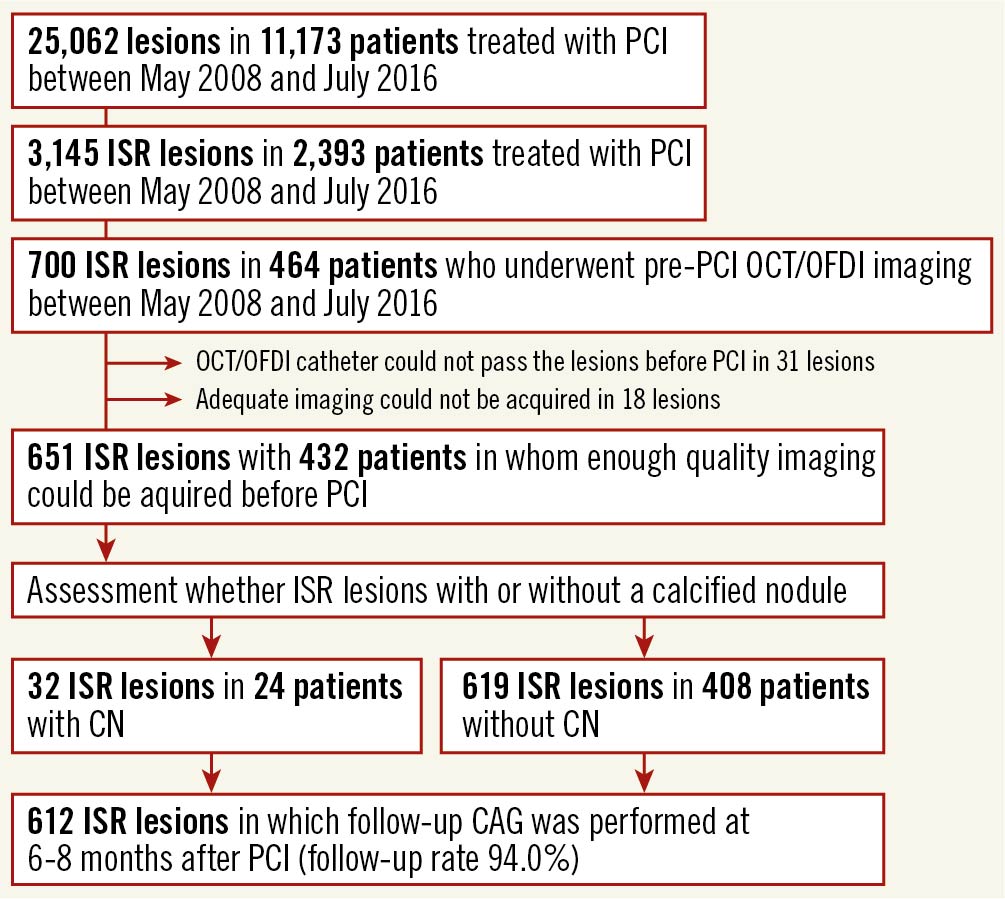
Figure 1. Study flow diagram. CAG: coronary angiography; CN: calcified nodule; ISR: in-stent restenosis; OCT: optical coherence tomography; OFDI: optical frequency domain imaging; PCI: percutaneous coronary intervention
PCI and OCT procedures
Cardiac catheterisation was performed with the use of 6 Fr or 7 Fr sheaths and a guiding catheter via the transradial or brachial approach. Intravenous heparin (about 100 U/kg, adjusted depending on age) and intracoronary nitrates were administered at the beginning of the procedure. After the initial angiography of the target vessel, OCT was performed to obtain information on the entire target vessel. Predilatation using a coronary balloon with a small diameter (1.5 to 2.25 mm) was performed before OCT imaging in 17 lesions because the target lesions were too tight to allow the OCT catheter to pass through. Between July 2008 and September 2011, time domain OCT was performed with the use of a 0.016-inch OCT catheter (ImageWire; LightLab Imaging). The OCT catheter was advanced to the distal end of the stent through a 3 Fr occlusion balloon catheter. To remove blood from the field of view, an occlusion balloon was inflated up to 0.6 atm at a site proximal to the lesion, and warm lactated Ringer's solution was infused into the coronary artery from the distal tip of the occlusion balloon catheter at a rate of 0.7 ml/s. Between October 2011 and July 2016, frequency domain OCT was performed with the use of a monorail-type OCT imaging catheter (Dragonfly [St. Jude Medical], or FastView [Terumo Corp.]). The OCT imaging catheter was advanced to the distal end of the stent along a 0.014-inch coronary guidewire. To remove blood from the field of view, a contrast agent was infused. The entire lesion length was imaged with an auto-pullback, and the OCT image clearly visualised the target vessel. After all the recordings, PCI was performed for all lesions. First, all lesions were dilated with a high-pressure balloon, a scoring balloon, or both. In the POBA group, the procedure was completed at that point. In the PCB group, further balloon dilatation with the use of a PCB (SeQuent Please balloon catheter; B. Braun Medical) was performed. The recommended inflation time for the PCB was 60 seconds, and the inflation pressure was a rated burst pressure (14 atm). In the DES or BMS groups, additional DES or BMS implantation and postdilatation with a high-pressure balloon were performed. The types of DES used in this study were as follows: sirolimus-eluting stent, 24 lesions; paclitaxel-eluting stent, 22 lesions; zotarolimus-eluting stent, 14 lesions; cobalt-chromium everolimus-eluting stent, 77 lesions; platinum-chromium everolimus-eluting stent, 20 lesions; biolimus-eluting stent, 21 lesions; and Ultimaster sirolimus-eluting stent (Terumo Corp.), 2 lesions. Because this was a retrospective study, there was no clear criterion for choosing a treatment strategy (POBA, PCB, DES, or BMS); it depended on the operator’s choice. Generally, we added stent implantation when we could not obtain a good angiographic result after predilatation with a high-pressure balloon.
Image analysis of CAG and OCT
Quantitative coronary angiography analysis (QCA) was performed with an automatic edge-detection system (QCA-CMS version 6; Medis Medical Imaging Systems BV). The analysis was performed through the in-stent segment and the adjacent proximal and distal 5 mm vessel segments. Quantitative measurements included reference vessel diameter, minimal luminal diameter, percentage diameter stenosis, and lesion length. Derived variables were as follows: acute gain = postprocedural minimum lumen diameter – preprocedural minimum lumen diameter and late loss = postprocedural minimum lumen diameter − follow-up minimum lumen diameter. Lesion morphologies before previous stenting, including angulated lesions, bifurcation lesions, calcified lesions, and chronic total occlusion, were defined angiographically according to the modified American College of Cardiology/American Heart Association (ACC/AHA) lesion morphology criteria14. Calcification was identified as readily apparent radiopacities within the vascular wall at the site of the stenosis and was classified as none/mild, moderate (radiopacities noted only during the cardiac cycle before contrast injection), and severe (radiopacities noted without cardiac motion before contrast injection, generally compromising both sides of the arterial lumen)15. Lesions with moderate/severe calcifications were defined as calcified lesions.
The OCT data were stored digitally and analysed by an OCT imaging system (LightLab Imaging), the ILUMIEN OCT imaging system (St. Jude Medical), or the LUNAWAVE imaging system (Terumo Corp.). Qualitative analyses of OCT images were performed at the minimum lumen area (MLA) site and every 1 mm of the preceding and following 5 frames (10 mm, 11 frames) before and after the procedure. The lumen area and stent area (SA) were traced manually, and the stent diameter (SD) and the intimal area (IA) were automatically calculated. Percent IA (%IA) was calculated as the IA divided by the SA. Differences in lumen area, SD, SA, and IA before and after the procedure were defined as the initial gain, ∆SD, ∆SA, and ∆IA, respectively. Based on the OCT image measurements, we determined the MLA site, minimum stent area (MSA) site, and CN site. We measured the distance between the MLA and CN sites, and calculated stent expansions at the three sites. The CN site was defined as a frame with the largest intimal area in which CN was observed. The percentage of stent expansion was defined as stent area divided by the mean of the largest proximal and distal reference lumen area. The largest proximal and distal reference lumen areas were identified within each reference segment adjacent (<5 mm) to each stent edge before the procedure16. ISA was defined as a distance between the adluminal surface of the strut and the vessel wall greater than the thickness of each stent strut17, and multiple interstrut hollows (MIH) were defined as (1) the existence of hollows between and outside the well-apposed stent struts, and (2) the maximum depths of the hollows >0.5 mm18.
Qualitative analyses of OCT images were performed by two experienced physicians (T. Tada and K. Miura) who were blinded to clinical and angiographic lesion characteristics. CN was defined as a high backscattering mass with small nodular calcium depositions which protruded in the vessel lumen and had an uneven surface and signal attenuation assessed with OCT or OFDI38. When the two physicians had different opinions, they reached a final decision after discussion. To assess inter-observer variability in the diagnosis of OCT findings of the presence of CN, OCT images were analysed independently by two experienced interventional cardiologists (T. Tada and K. Miura) who were blinded to the clinical data. Furthermore, one of the two observers (T. Tada) evaluated all OCT images again at four months after the initial evaluation to assess the intra-observer variability in the diagnosis of OCT findings for the presence of CN.
Clinical and angiographic follow-up after PCI
Clinical and angiographic follow-up was performed at 6 months after a successful procedure in the POBA and PCB groups and at 8 months in the DES group. A follow-up angiogram was obtained earlier if clinically indicated. Binary restenosis at follow-up was defined as stenosis occupying more than 50% of the diameter. TLR was defined as any repeat PCI or coronary bypass surgery owing to restenosis (percentage diameter stenosis ≥50%) associated with symptoms or objective signs of ischaemia.
Statistical analysis
Data are expressed as means±standard deviations, except for the data pertaining to time from PCI to ISR because these data did not follow a normal distribution. The data pertaining to time from PCI to ISR are expressed as medians (interquartile range). Intergroup comparisons were conducted by the χ2 independence test or Fisher’s exact probability test, and differences in mean values were tested by the Student’s t-test at a critical level of 5% or lower. The Mann-Whitney U test was used to compare time from PCI to ISR between the two groups. Multiple lesions within the same patient were assumed to be independent of each other. If a patient had two lesions with and without CN, he/she was regarded as a CN patient. To assess the independent predictors of the presence of CN in lesion-level data, multivariable analysis was performed with the use of generalised estimation equations. Rotablation was not adopted in the multivariate analysis because it exhibited a strong causal relationship with calcified lesion, and calcified lesion was adopted in the multivariate analysis. To assess the independent predictors of the occurrence of re-TLR in lesion-level data, multivariable analysis was also performed with the use of generalised estimation equations. Variables were adopted in multivariate analysis if the p-value in univariate analyses was less than 0.10. Inter- and intra-observer variabilities in the diagnosis of tissue morphology were evaluated by Cohen’s coefficient kappa. All data were analysed with SPSS software, Version 27.0.0.0 (IBM Corp.).
Results
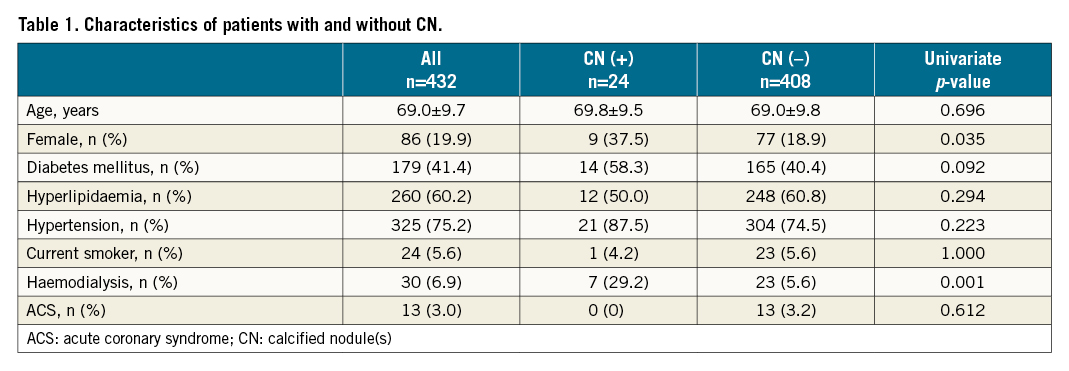
Patient and lesion characteristics with and without CN, and the prevalence of CN
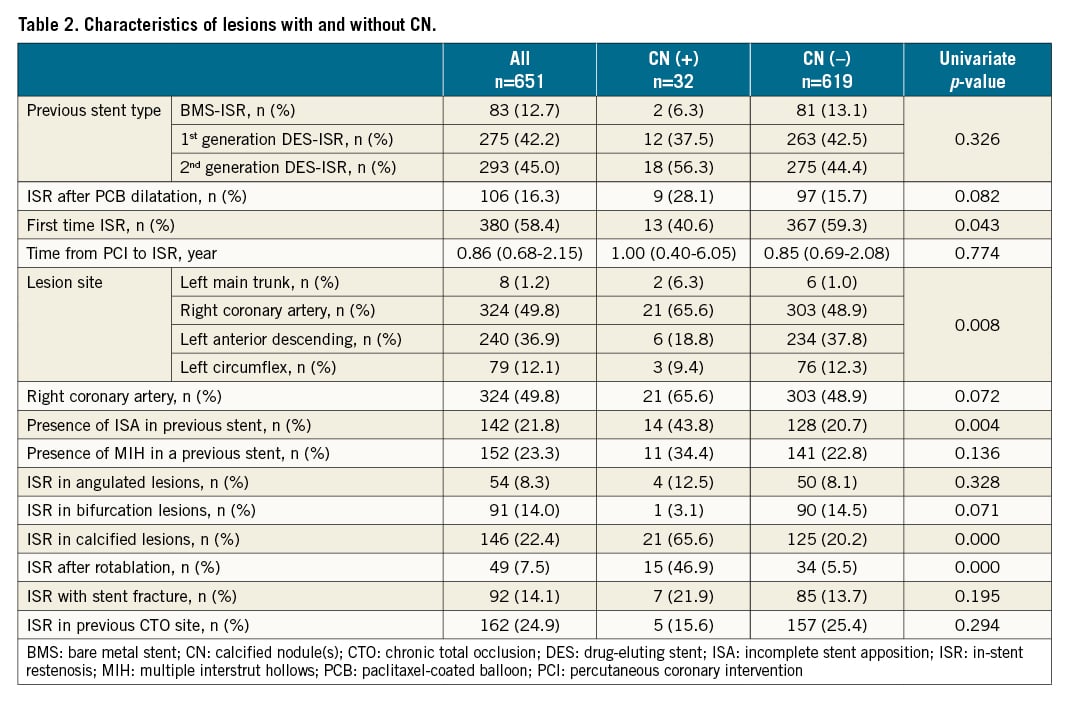
The patients were 346 men and 86 women with a mean age of 69.0±9.7 years. The median period from the initial PCI to ISR was 0.86 years (range 0.68-2.15). ISR lesions with CN were observed in 32 lesions (24 patients), the prevalence of CN was 4.9%. Two representative cases of an ISR lesion with CN are shown in the Central illustration. Patient and lesion characteristics with and without CN are listed in Table 1 and Table 2. In patients with CN, there were more women than men (37.5% vs 18.9%, p=0.035). The prevalence of haemodialysis (HD) was higher in patients with CN than in those without CN (29.2% vs 5.6%, p=0.001) (Table 1). Lesions with CN were more frequently observed than those without CN in calcified lesions (65.6% vs 20.2%, p<0.001) and lesions after rotablation (46.9% vs 5.5%, p<0.001). Lesions with CN were less frequently observed than those without CN in the first-time ISR lesions (40.6% vs 59.3%, p=0.043). Incomplete stent apposition (ISA) in previously implanted stents was more frequently observed in lesions with CN than in those without CN (43.8% vs 20.7%, p=0.004) (Table 2).
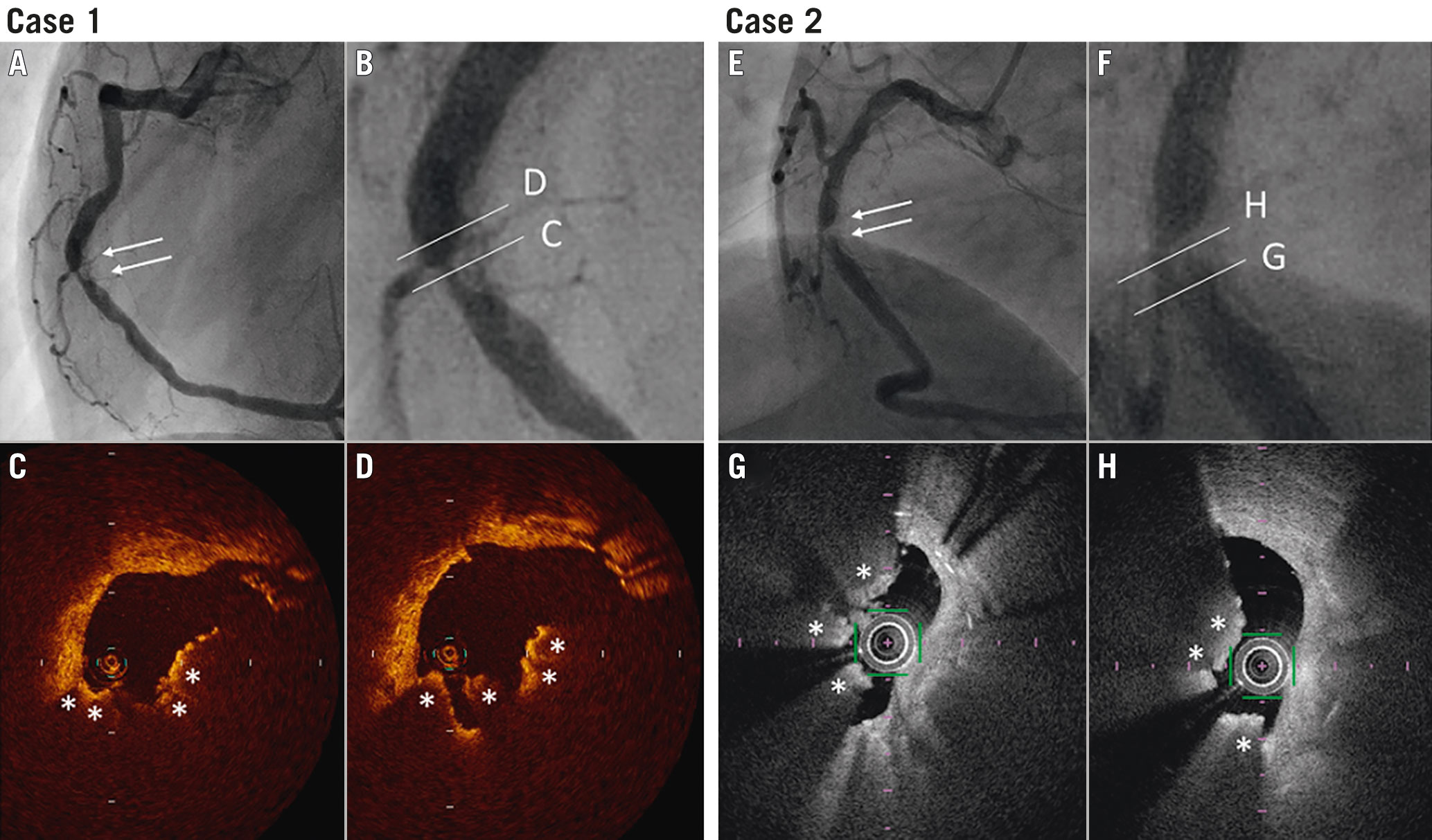
Central illustration. Two representative cases of ISR lesions with calcified nodules. Case 1: A) An ISR lesion was observed in the mid portion of the right coronary artery three years after paclitaxel-eluting stent implantation in a 55-year-old HD patient (white arrows). B) Magnified view of the lesion. C) & D) OCT images showed a protruding irregular mass with the deposition of small nodular calcification (asterisks). Case 2: E) An ISR lesion was observed in the mid portion of the right coronary artery one year after platinum-chromium everolimus-eluting stent implantation in an 81-year-old HD patient (white arrows). F) Magnified view of the lesion. G) & H) OCT images showed a protruding irregular mass with the deposition of small nodular calcification (asterisks).
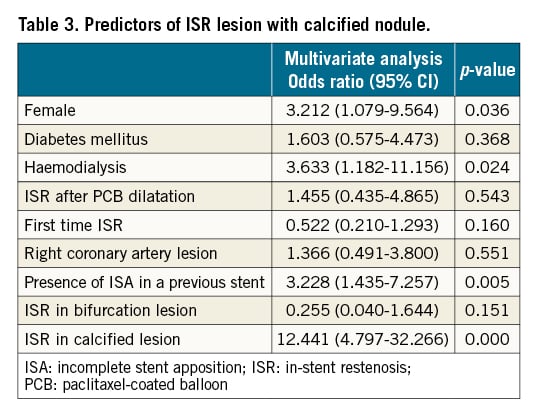
Predictors of ISR lesions with CN
A multivariate analysis was performed for predictors of ISR lesions with CN (Table 3). It showed that calcified lesions, the presence of ISA in previously implanted stents, HD, and female gender were independently associated with the prevalence of ISR lesions with CN.
QCA analysis of lesions with and without CN at PCI and follow-up CAG
QCA analysis outcomes for lesions with and without CN at PCI and follow-up CAG are listed in Table 4.
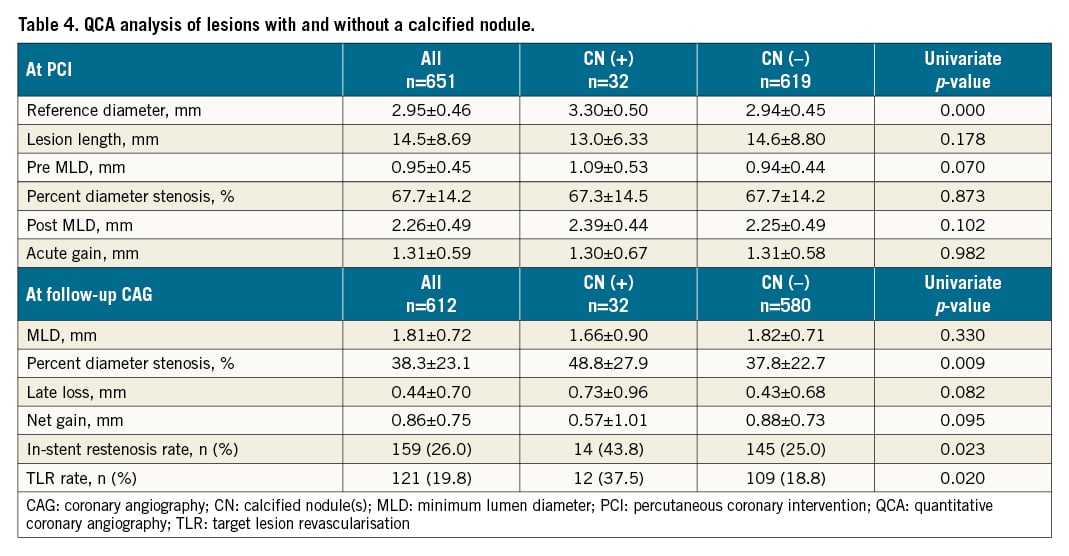
At PCI, the reference diameter of lesions with CN was significantly larger than that of those without CN (3.30±0.50 mm vs 2.94±0.45 mm, p<0.001). There were no significant differences in lesion length, preprocedural minimum lumen diameter, preprocedural percent diameter stenosis, postprocedural minimum lumen diameter, and acute gain between lesions with and without CN.
Follow-up CAG was performed in 612 lesions (32 lesions with CN and 580 lesions without CN; follow-up rate 94.0%) at 6 to 8 months after PCI. At follow-up CAG, the percent diameter stenosis of lesions with CN was significantly larger than that of the lesions without CN (48.8%±27.9% vs 37.8%±22.7%, p=0.009). Late lumen loss tended to be greater in lesions with CN than in those without CN and the net gain tended to be smaller in lesions with CN than in those without CN.
OCT findings in ISR lesions with and without CN
CN were identified at stent borders in 4 out of 32 CN cases that were adjacent (<5 mm) to a stent edge; the CN were identified within the body of the stent in the other 28 CN cases. The CN sites were the same cross-sections as the MLA sites in 18 out of 32 CN cases and mean distance between the two sites was 0.79±1.45 mm.
We compared OCT findings before and after the procedures between ISR lesions with and without CN (Table 5). Before the procedure, MLD, MLA, SD, and SA were significantly larger, %IA was smaller, and the stent underexpansion rate tended to be higher in lesions with CN than in those without CN. After the procedure, MLD, MLA, SD, and SA were significantly larger, and %IA was smaller in lesions with CN than in those without CN. There were no differences in IA, initial gain, ΔSD, ΔSA, and ΔIA between the two groups.
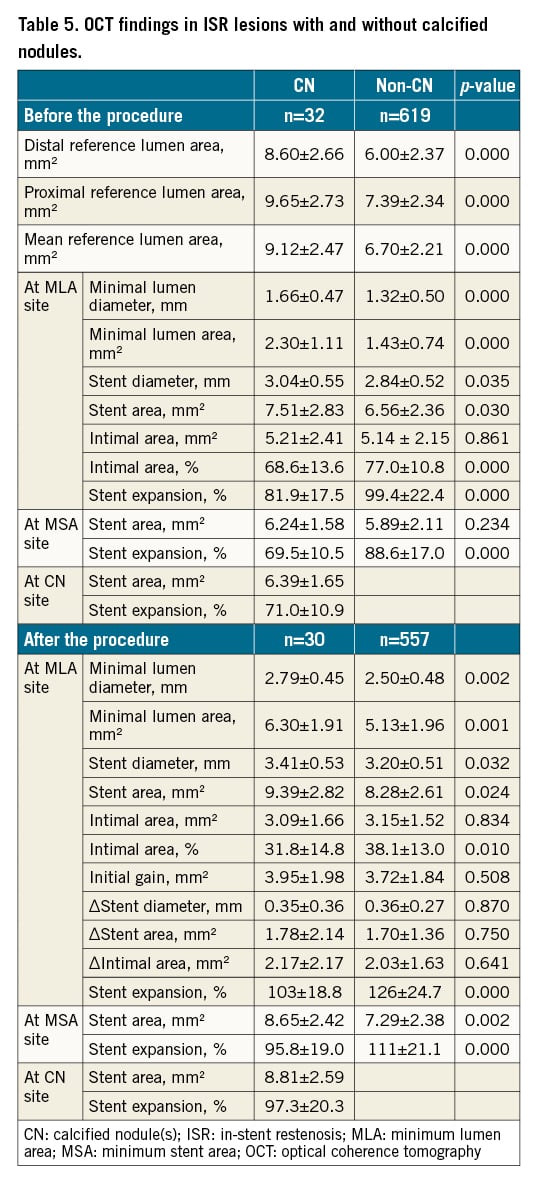
Furthermore, we examined the stent expansion at MLA and MSA sites in all cases, and at the CN site in CN cases before and after procedures (Table 5). The stent expansions were significantly smaller in lesions with CN than those in lesions without CN both before and after the procedure at the MLA and MSA sites. Mean stent expansions at the CN site in CN cases before and after procedures were 71.0±10.9 % and 97.3±20.3 %, respectively.
OCT findings of CN in patients with and without HD
In 32 lesions with CN, there were 9 CN lesions in patients with HD. We also compared OCT findings before and after the procedures between CN lesions in patients with and without HD (Supplementary Table 1). Proximal and mean reference lumen area were significantly larger in patients with HD than in those without HD. Before the procedure, there were no significant differences in MLD, MLA, SD, SA, IA, %IA, and stent expansion between the two groups. After the procedure, IA tended to be larger in CN lesions with HD than in those without HD (3.96±1.51 mm2 vs 2.71±1.60 mm2, p=0.056); however, there were no differences in MLD, MLA, SD, SA, %IA, initial gain, ∆SD, ∆SA, ∆IA, and stent expansion between the two groups.
Midterm results after PCI for ISR lesions with and without CN
As shown in Figure 2, both the re-ISR and the re-TLR rates at 6 to 8 months after PCI were significantly higher in lesions with CN than in in those without CN (43.8% vs 25.0%, p=0.023; 37.5% vs 18.8%, p=0.020; respectively).
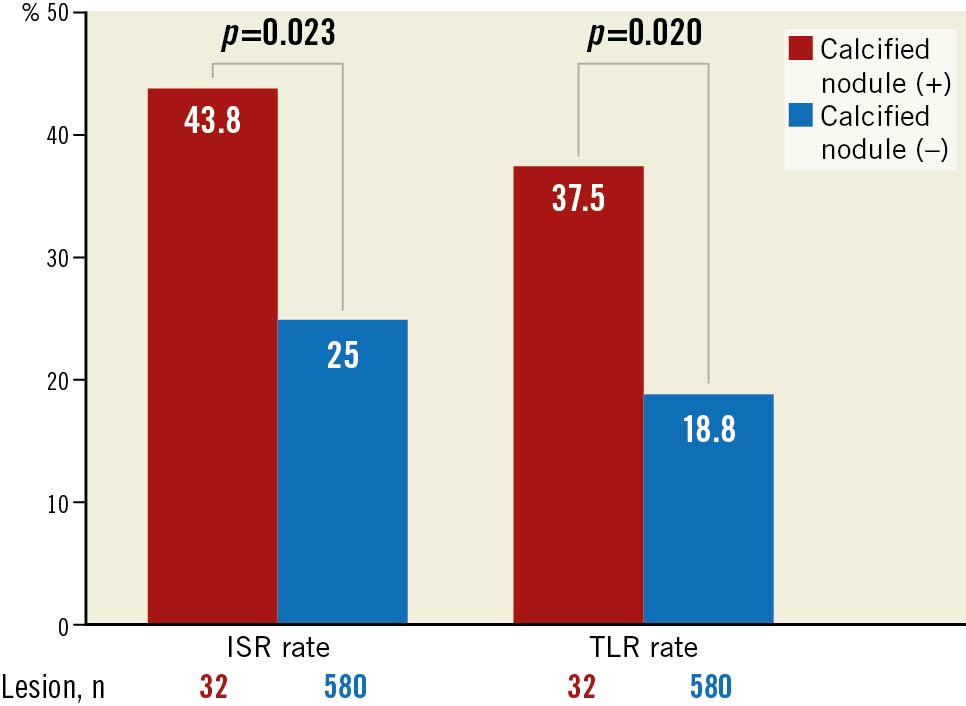
Figure 2. Midterm (6 to 8 months) results after PCI for ISR lesions with and without CN. The ISR and TLR rates in lesions with CN were significantly higher than those in lesions without CN. CN: calcified nodule; ISR: in-stent restenosis; PCI: percutaneous coronary intervention; TLR: target lesion revascularisation
To assess the independent predictors of the occurrence of re-TLR, multivariable analysis was performed. It showed that HD and ISR lesions in previous CTO sites (and not CN) were independent predictors of re-TLR (Table 6).

Association between midterm results and PCI devices in lesions with and without CN
The differences in the midterm results between lesions with and without CN with respect to each PCI device are shown in Figure 3. It was difficult to assess the effect of POBA on lesions with CN because the number of lesions with CN treated with POBA alone was too small. It was also difficult to assess the effects of BMS on lesions with CN. The data are not presented because the number of lesions with CN treated with BMS was also too small.
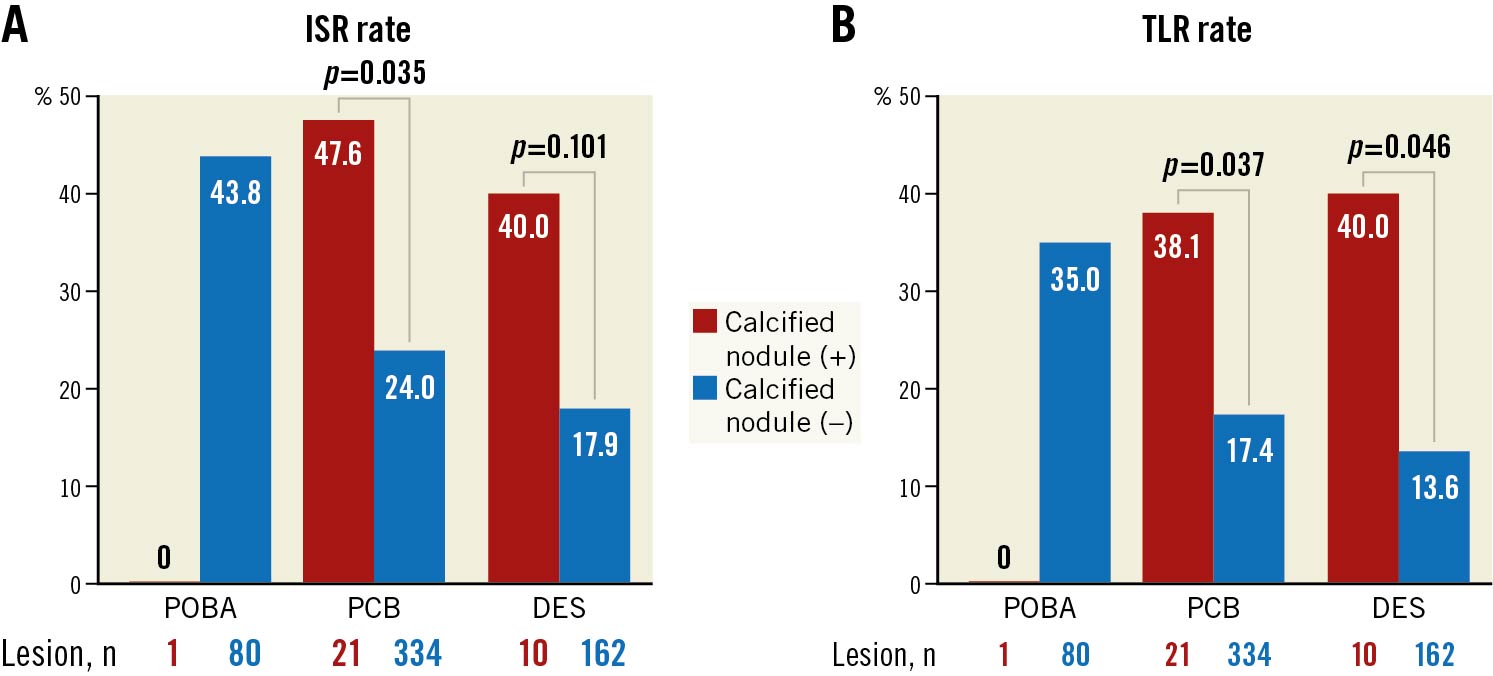
Figure 3. The association between midterm results and PCI devices in lesions with and without CN. In lesions treated with both PCB and DES, both ISR (panel A) and TLR (panel B) rates were significantly higher in lesions with CN than in those without CN. CN: calcified nodule; DES: drug-eluting stent; ISR: in-stent restenosis; PCI: percutaneous coronary intervention; PCB: paclitaxel-coated balloon; POBA: plain old balloon angioplasty; TLR: target lesion revascularisation
Reproducibility of analysed OCT results
Inter- and intra-observer variabilities (κ values) in qualitative OCT assessments were 0.84/0.84 for CN.
Discussion
This is the first study on the prevalence of ISR lesions with CN. The major findings are as follows: 1) the prevalence of ISR lesions with CN was 4.9%, it was especially high in calcified lesions, HD patients, female patients, and lesions with ISA in previously implanted stents, and 2) ISR lesions with CN treated with either PCB or DES may have poor midterm outcomes compared with ISR lesions without CN.
Using OCT, Lee et al reported that 4.2% of de novo culprit lesions contained CN3. In this study, the prevalence of ISR lesions with CN was 4.9%; this value was relatively close to the result described above. The same authors also reported that the proportion of females, diabetes mellitus, and HD were significantly higher in lesions with CN than in those without CN3. These results are consistent with our results.
In this study, HD was also one of the independent predictors of ISR lesions with CN (OR 5.284, 95% CI: 1.989 to 14.038, p= 0.001). It is well known that coronary plaques in HD patients are characterised by marked calcifications192021. Chin et al reported that the prevalence of CN in HD patients was 16% in culprit lesions and 13% in non-culprit lesions, these rates were relatively high21. It was reported that a) HD patients are exposed to metabolic abnormality in serum calcium and phosphorus, inflammatory cytokines, and oxidative stress, and that b) these factors promote apoptosis of vascular smooth muscle cells, thus leading to vascular calcification22. These mechanisms may also be involved in the formation of CN in HD patients. Furthermore, in this study, the IA after the procedure in CN lesion with HD tended to be larger than in those without HD. This may suggest that more severe calcification occurs in in-stent CN lesions with HD than in those without HD, and that it is more difficult to displace to the outer parts of the in-stent CN lesions with HD than those without HD.
Previous pathological studies have suggested that CN consists of nodular calcifications and fibrin deposition and that the mechanism of CN formation is associated with nodular calcification erupting from a fragmented calcified plate, fibrin, and thrombus surrounding the nodular calcification7112324. In this study, in-stent CN were frequently observed in calcified lesions. Vessel injury owing to PCI may cause the fracture of the coronary calcified plate on the outer parts of the stent and may thus lead to eruption of nodular calcification and in-stent CN formation. The presence of ISA in previously implanted stents was also a predictor of CN. ISA has been reported as being a cause of in-stent thrombus formation2526. However, the role of ISA in the process of in-stent CN formation was unclear. Calcified lesions were frequently observed in ISR lesions with CN, and ISA frequently occurs in calcified lesions. That may be why ISA was frequently observed in ISR lesions with CN.
In our OCT quantitative analyses, there were no significant differences in postprocedural and initial gain, ∆stent area, and ∆intimal area between lesions with and without in-stent CN, although it appeared to be difficult to achieve sufficient post-procedural acute gain in ISR lesions with CN. However, stent expansions before and after the procedure were significantly smaller in lesions with CN than those in lesions without CN. Furthermore, stent expansions at the CN site before and after the procedure were even smaller. Stent underexpansion is reported as being one of the risk factors for ISR2728, and lesions with severe calcification are at risk of stent underexpansion29. Stent underexpansion in CN cases might occur as a result of PCI for severely calcified lesions.
There are some case reports on ISR due to CN910111213. However, there are few data on the clinical outcomes after PCI for ISR lesions with CN. This study is the first systematic report concerning the midterm results after PCI for ISR lesions with CN. In this study, both ISR and TLR rates were significantly higher in lesions with CN than in those without CN. Additionally, ISR lesions with CN treated with either PCB or DES may have poor midterm outcomes compared with ISR lesions without CN. However, multivariate analyses showed that HD and ISR lesions in a previous CTO site, (and not CN) were independent predictors of re-TLR. The reasons for which CN was not an independent predictor of re-TLR were that (1) CN had strong confounding factors, such as HD and calcified lesions (specifically, HD served as an independent predictor of re-TLR), and (2) the prevalence of CN was 4.9% on ISR lesions and the impact on the whole re-TLR may be relatively small. The ISR rates in lesions with CN treated with PCB and DES were 47.6% and 40%, respectively. Neither PCB nor DES were effective for ISR lesions with CN, despite the fact that both constitute the main strategies for ISR lesions nowadays. There was no significant difference in acute gain between lesions with and without CN. This suggested that the acute results were unlikely to have a significant impact on the midterm results, although the reason for the poor midterm results after PCI for ISR lesions with CN was unclear. We sometimes find recurrent CN after PCI for ISR lesions with CN. Patient and lesion characteristics including HD, calcified lesions, and the presence of ISA, which promote CN formation, may also have an impact on recurrent ISR after PCI for ISR lesions with CN.
Limitations
There are several limitations associated with this study. First, this study was a single-centre, retrospective study, and selection lesion bias may have existed. The number of lesions with CN was small, which makes it difficult for the results of this study to be generalised to other cohorts. Second, qualitative definitions of CN are associated with some limitations. However, the inter- and intra-observer reproducibility of the OCT analysis results were generally good, and easiness of qualitative assessment may be important in terms of the clinical usefulness. Third, there were no pathological assessments of lesions with and without CN. CN was defined only with OCT images in this study and OCT images of CN may emulate acute red thrombus. Although there were no ACS patients among the patients with CN, we could not rule out misdiagnosis of CN instead of thrombus. Fourth, there was no morphological plaque assessment with the use of intracoronary imaging prior to previous stent implantation. Fifth, control angiograms may have had some impact on the high re-TLR rate not only in lesions with CN, but in lesions without CN (37.5% and 18.8%, respectively).
Conclusions
The prevalence of ISR lesions with CN was 4.9%, which was similar to that of native coronary arteries. Calcified lesions, HD, female gender, and ISA may be associated with CN formation. ISR lesions with CN treated with either PCB or DES may have poor midterm outcomes compared with ISR lesions without CN. Further studies are needed to explore the optimal strategy for ISR lesions with CN.
Impact on daily practice
This is the first systematic report on the prevalence and predictors of ISR lesions with CN, and on midterm results after repeat PCI for the ISR lesions with CN. The prevalence of ISR lesions with CN was 4.9%. Calcified lesions, ISA, HD, and the female gender are probably associated with CN formation. Because the formation of CN may suggest a poor outcome after repeat PCI, we should consider the indications for PCI and the procedures to avoid ISA when we think about PCI for lesions with a high risk of CN formation.
Acknowledgements
We wish to thank Miho Kobayashi, Makiko Kanaike, and Takako Yukiyoshi for their secretarial assistance. We also thank Hayato Shimizu and his colleagues for their technical assistance.
Conflict of interest statement
T. Tada has received lecture fees from Terumo Corporation and Abbott Vascular. K. Kadota has received lecture fees from Terumo Corporation and Abbott Vascular. S. Kubo has received lecture fees from Abbott Vascular. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.