Abstract
Aims: Guidewire (GW) tracking in a collateral channel (CC) is an important step during retrograde chronic total occlusion (CTO) percutaneous coronary intervention (PCI). The aim of this study was to create a prediction score model for CC GW crossing success.
Methods and results: We analysed data on 886 CCs included in the Japanese CTO PCI Expert Registry during 2016. CCs were categorised as septal (n=610) and non-septal (n=276). CCs were randomly assigned to derivation and validation sets in a 2:1 ratio. The score was developed by multivariate analysis with angiographic findings. Small vessel, reverse bend, and continuous bends were independent predictors in the septal CC subset. Small vessel, reverse bend, and corkscrew were independent predictors in the non-septal CC subset. The extent of intervention was easy, intermediate, and difficult in 92.9%, 57.4%, and 16.7% in the septal CC subset and 91.7%, 54.3%, and 19.0% in the non-septal CC subset, respectively, in the validation set. The area under the receiver operating characteristic curve was >0.7 in the derivation and validation sets of both CC subsets.
Conclusions: The prediction score model can suggest grading of the difficulty of CC GW crossing based on angiographic findings for each type of CC.
Introduction
Recent algorithms of coronary chronic total occlusion (CTO) percutaneous coronary intervention (PCI) have involved retrograde CTO-PCI1,2,3. Technical success of retrograde CTO-PCI is associated with the success of collateral channel (CC) guidewire (GW) crossing4. The anatomical morphology of CC affecting CC GW crossing success is an important issue for the success of retrograde PCI5.
Previous studies have reported the predictors of technical retrograde CTO-PCI success6,7. However, only a few studies have examined possible predictors of CC GW crossing success8,9. Therefore, in this study, we investigated potential angiographic predictors and established a scoring model for CC GW crossing success based on analyses of the Japanese CTO PCI Expert Registry10.
Methods
PATIENT POPULATION
This study was conducted using data from the Japanese CTO PCI Expert Registry. This was a multicentre, prospective, and non-randomised registry. The design of this Registry has been described elsewhere10. We used data from about 2,706 CTO-PCI procedures that were included from January 2016 to December 2016. On the basis of the uniformity of device availability, 1,621 CTO-PCI performed in Japan were selected. Of these cases, 685 cases underwent retrograde CTO-PCI. Of these, 1, 2 and 10 cases were excluded because of the presence of two CTO lesions treated in one procedure, inadequate anatomical indication, and inappropriate patient data and lesion background, respectively. After exclusion, 672 cases, including 948 CCs, were investigated. Of these 948 CCs, 19 with CCs attempted via a bypass graft were excluded. Another 43 CCs without tip injection were also excluded, because tip injection was recommended to recognise the anatomical morphology of the CCs11. Thus, in total, 886 CCs in 630 cases were assessed.
DEFINITIONS
PROCEDURES
For estimating lesion difficulty, the J-CTO (Multicenter CTO Registry in Japan) score was used12. Technical CTO-PCI success was defined as successful GW crossing and <50% residual stenosis with Thrombolysis In Myocardial Infarction flow grade 3. Major complications were hospital death, myocardial infarction, emergency PCI or coronary artery bypass grafting, cardiac tamponade requiring intensive treatment, and puncture-site bleeding requiring blood transfusion or surgical treatment. CC GW crossing success was defined as GW crossing through the CC from the retrograde side and reaching the CTO distal vessel segment. CC microcatheter (MC) crossing success was defined as MC crossing through the CC from the retrograde side and reaching the CTO distal vessel segment after GW crossing. CC perforation requiring treatment was defined as a CC treated with coiling or balloon haemostasis after CC perforation.
ANGIOGRAPHIC DEFINITIONS
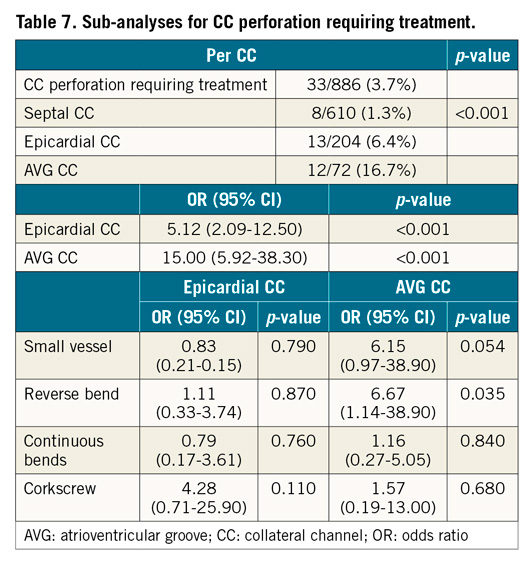
CCs were classified into three types8 – septal, epicardial, and atrioventricular groove (AVG). AVG CCs were on the AVG, with the CC connected between the left circumflex artery and the right coronary artery. Two CC subsets were defined – septal and non-septal (epicardial and AVG CC). Figure 1 shows the angiographic definitions. The small and large vessels were classified with reference to Werner’s CC grade13. Large vessel size was defined as CC2. Small vessel size was defined as CC0 or CC1 (Figure 1A). A significant CC vessel bend was described as an angle of bend of ≥45°. A reverse bend was described as part of the bend folded at an angle of >90° (Figure 1B). A continuous bend was specified when the height of the bend (a) exceeded the length between bends (b), that is, when a was >b (Figure 1C). At least three continuous bends (except corkscrew morphology) were considered variables of continuous bends. Corkscrew was defined as three or more continuous bends with a ratio of vessel amplitude/vessel diameter (AD ratio) ≤2 (Figure 1D). An acute angle with a distal recipient vessel was described as an acute angle of <45° between the CC and the recipient vessel5. If the CC did not have any bends, this morphology was defined as straight. These angiographic findings were observed by an experienced CTO examiner.
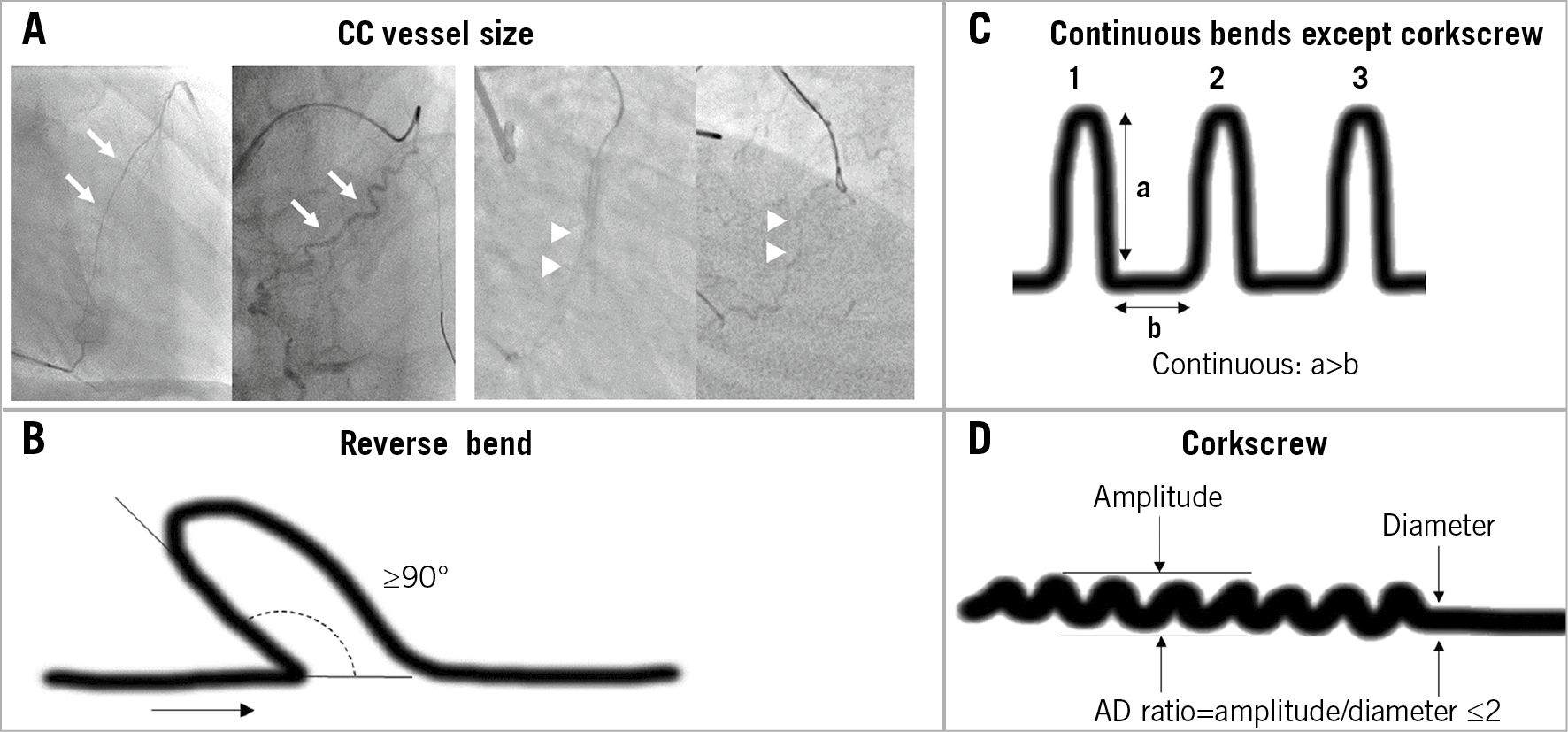
Figure 1. Definitions of angiographic findings. A) Arrows = large size CC such as CC2; arrowheads = small size CC such as CC1. Large vessel size was defined as CC2. Small vessel size was defined as CC0 or CC1. CC grade (CC0-2) was proposed by Werner13. B) The reverse bend was described as a part of a bend folded at an angle of >90°. C) Continuous bend was defined as the height of a bend (a) exceeding the length between bends (b), that is, when a is >b. At least three continuous bends, except corkscrew morphology, were termed as variables of continuous bends. D) Corkscrew was defined as three or more continuous bends with a ratio of vessel amplitude/vessel diameter (AD ratio) ≤2. CC: collateral channel
STATISTICAL ANALYSIS
In each CC subset, CC samples were randomly categorised to the derivation and validation sets in a 2:1 ratio. Both derivation and validation sets were compared using the chi-square or Fisher’s exact test, as appropriate. For each CC subset derivation set, univariate analysis was performed between variables and CC GW crossing success by the chi-square or Fisher’s exact test, as appropriate. After these univariate analyses, variables with statistical significance (p<0.10) were analysed with a multivariable model using logistic regression analysis. The prediction score model was defined by comparison with a beta coefficient for each CC subset. The summed score for each CC subset was graded into three categories – easy, intermediate, and difficult. To confirm the accuracy of the prediction score model, a receiver operating characteristic (ROC) curve analysis was performed using the derivation and validation sets14. Furthermore, an analysis of GW trends in each angiographic variable was conducted. All statistical analysis was performed using R software, version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria). Continuous variables were summarised as mean and SD; p<0.05 was considered statistically significant.
Results
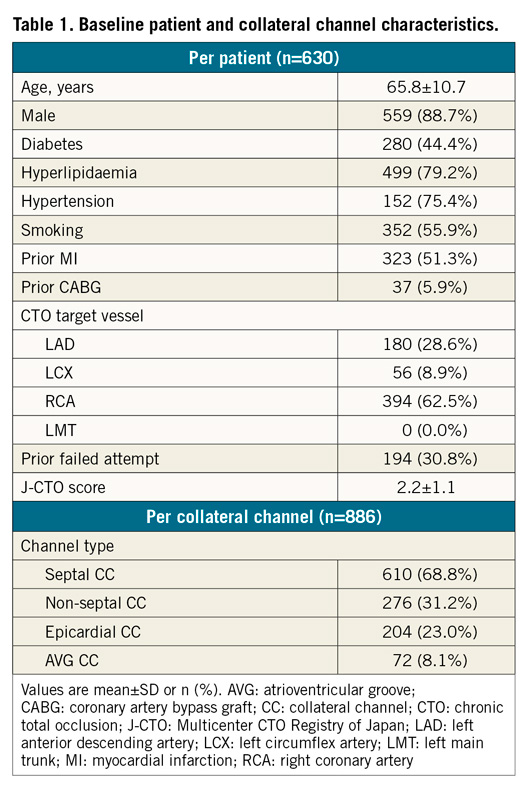
Baseline patient data and CC characteristics are summarised in Table 1. The number of septal and non-septal CCs was 610 (68.8%) and 276 (31.2%), respectively.
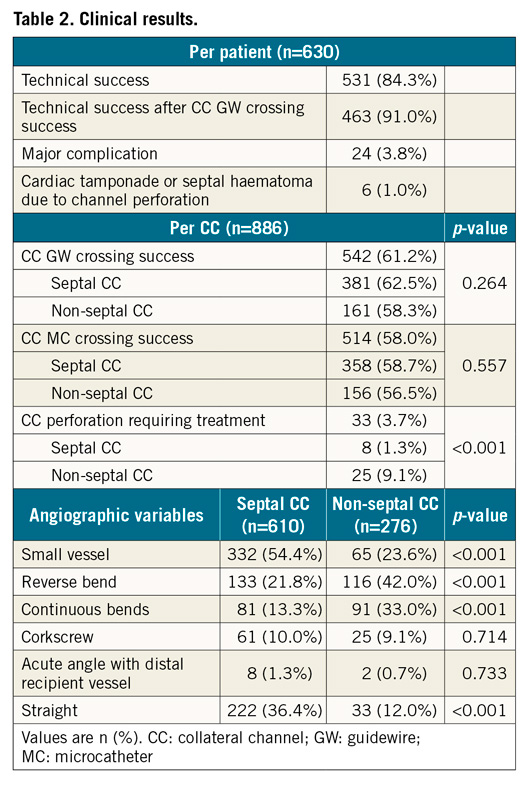
Clinical results are presented in Table 2. The technical CTO-PCI success rate was 84.3%. The CC GW crossing success rate was 61.2%. The CC GW crossing success rate among CC subsets was not significantly different. The rate of occurrence of CC perforation requiring treatment was 3.7% (33 CCs).
SEPTAL CC SUBSET
A total of 610 septal CCs was randomly allocated to a derivation set (407 CCs) and a validation set (203 CCs) in a 2:1 ratio. No significant difference was noted between the derivation and validation sets for any variable (Table 3). In the derivation set, the CC GW crossing success rate was 61.9%. Univariate analysis revealed a significant difference in angiographic variables of small size, reverse bend, and continuous bends between the successful and unsuccessful groups for CC GW crossing (Table 4). Those three variables were analysed in the multivariable analysis. Small vessel size, reverse bend, and continuous bends were revealed as significant independent predictors. The value of the beta coefficient of small vessels, reverse bend, and continuous bends was 2.09, 1.51, and 0.81, respectively (Table 5).
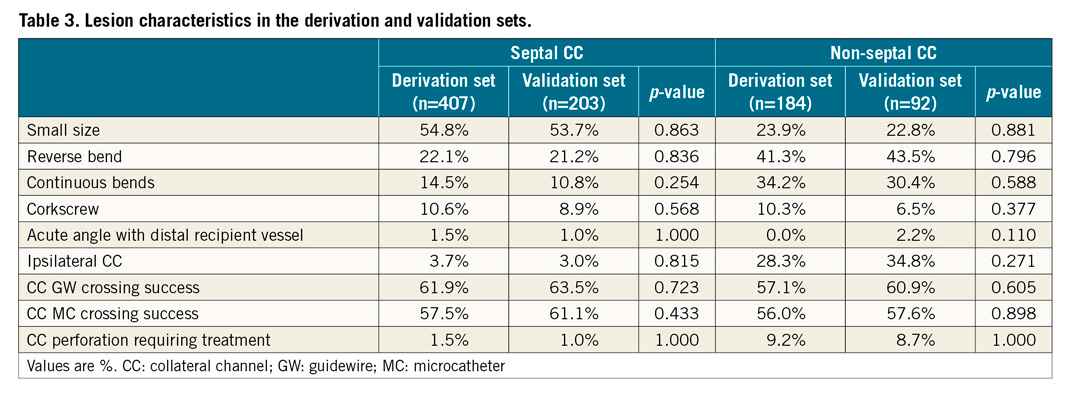

NON-SEPTAL CC SUBSET
A total of 276 non-septal CCs was randomly assigned to the derivation set (184 CCs) and validation set (92 CCs) in a 2:1 ratio. No significant difference was noted between the two sets for any variable (Table 3). In the derivation set, the CC GW crossing success rate was 57.1%. Univariate analysis revealed a significant difference in angiographic variables for small size, reverse bend, continuous bends, and corkscrew between the successful and unsuccessful groups for CC GW crossing (Table 4). Those four variables were analysed by multivariable analysis. Small vessel size, reverse bend, and corkscrew were found to be significant independent predictors. The value of the beta coefficient of small vessel size, reverse bend, and corkscrew was 2.43, 1.46, and 1.51, respectively (Table 5).
DEVELOPING A PREDICTION SCORE FOR ESTIMATING THE DIFFICULTY OF CC GW CROSSING SUCCESS: J-CHANNEL SCORE
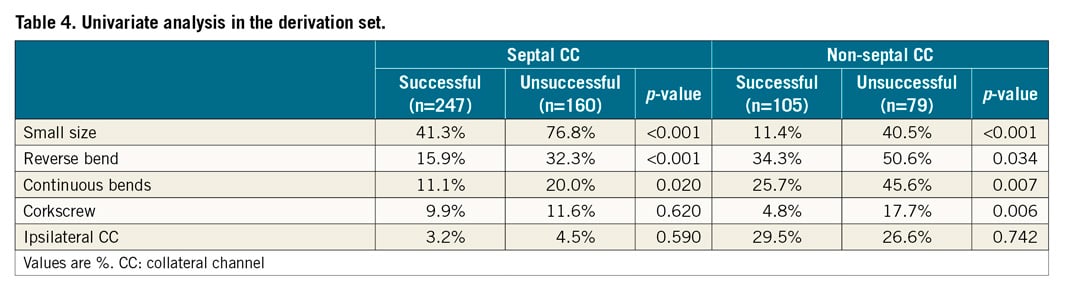
For scoring, the value of the beta coefficient 2.43 was considered a score of 3, 2.09 was a score of 2, and 0.81–1.51 was a score of 1. The variable factors of small vessel size, reverse bend, continuous bends, and corkscrew provided scores of 2, 1, 1, and 0, respectively, in the septal CC subset and scores of 3, 1, 0, and 1, respectively, in the non-septal CC subset. The area under the ROC curve of the derivation and validation sets was 0.744 and 0.743, respectively, in the septal CC subset and 0.757 and 0.826, respectively, in the non-septal CC subset (Figure 2).
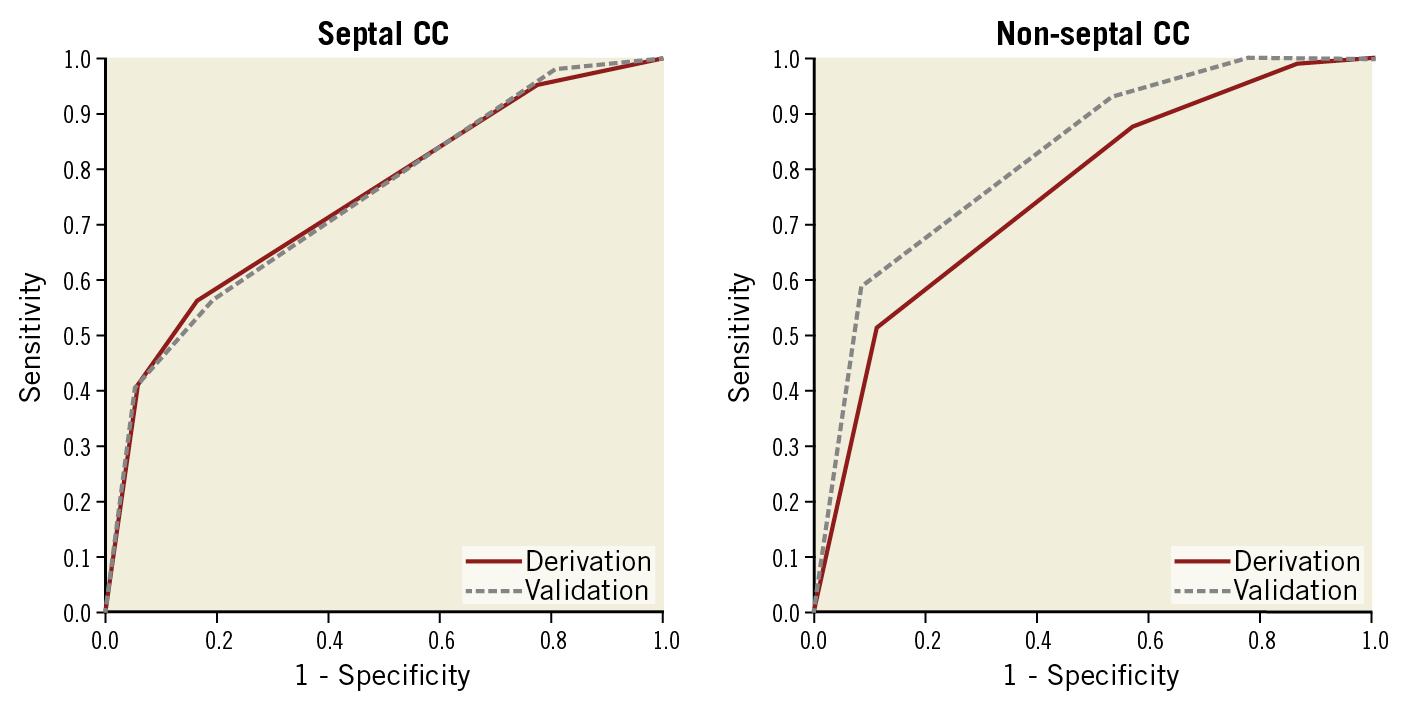
Figure 2. Receiver operating characteristic curves for evaluation of the new scoring model. The area under the curve of derivation and validation sets was 0.744 and 0.743, respectively, in the septal CC subset and 0.757 and 0.826, respectively, in the non-septal CC subset. CC: collateral channel
Figure 3 depicts the risk groups of the derivation and validation sets of each type of CC. The summed scoring numbers were assigned to three risk groups – easy, intermediate, and difficult defined as 0, 1–2, and ≥3, respectively. The rate of CC GW crossing success in the easy, intermediate, and difficult risk groups was 92.9%, 57.4%, and 16.7%, respectively, in the validation set of the septal CC subset and 91.7%, 54.3%, and 19.0%, respectively, in the validation set of the non-septal CC subset.
Figure 3. Relationships between the CC GW crossing success and the risk groups. Relationships between the CC GW crossing success and the risk groups were defined as easy, intermediate, and difficult due to total score in derivation and validation sets. CC: collateral channel; GW: guidewire
ANALYSIS OF GW TRENDS
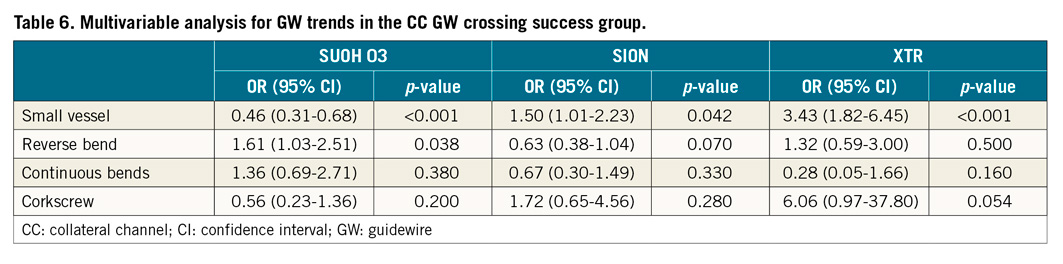
The prevalence of GWs used in the CC GW crossing success group is shown in Figure 4. Those GWs were final GWs for CC negotiation. The total ratio of different GWs (SUOH 03 [48.3%], SION [31.9%], and XTR [9.2%]; Asahi Intecc, Nagoya, Japan) was 89.4%. In these three types of GW, a multivariate analysis was performed for the angiographic variables (Table 6). XTR and SION GWs showed a statistically significant use for small vessel size. The SUOH 03 GW showed a statistically significant use for the reverse bend.
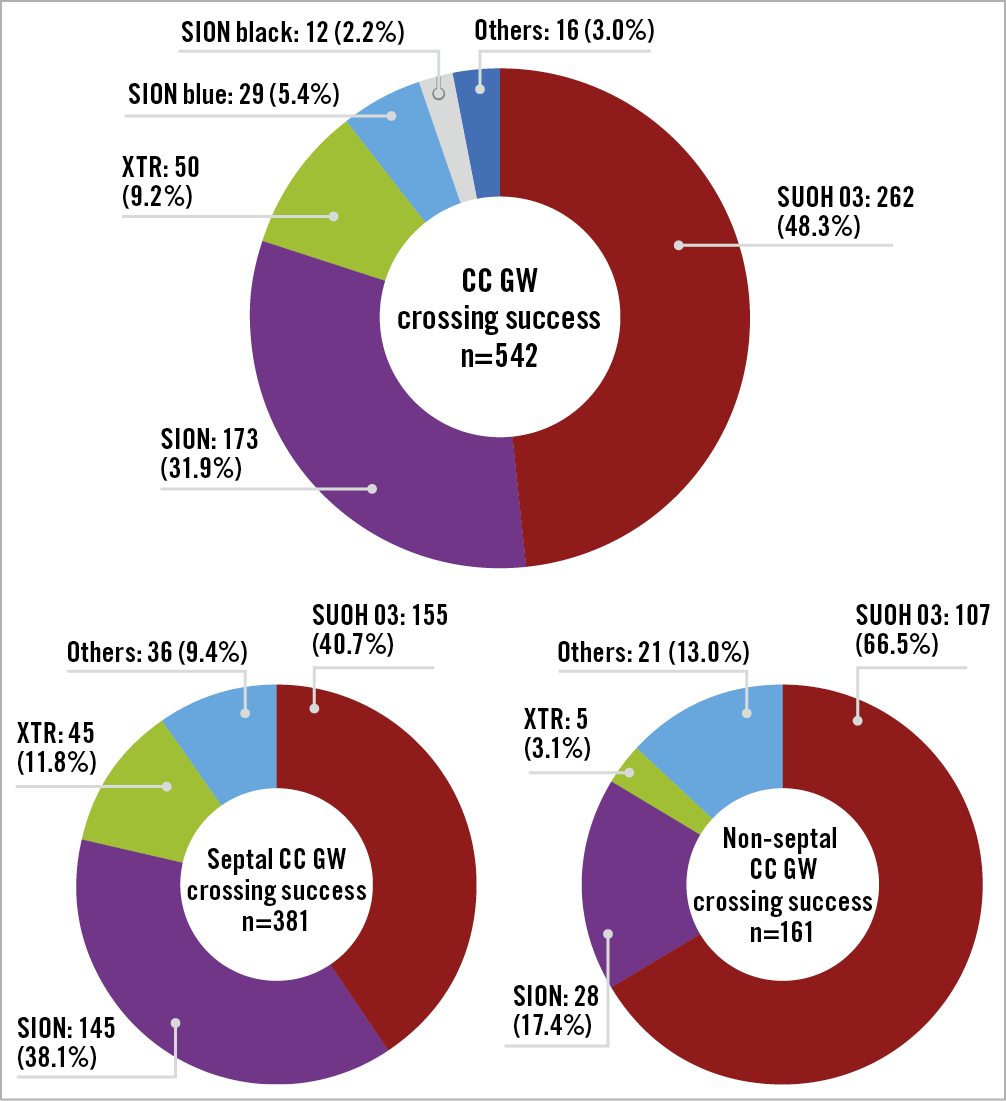
Figure 4. Prevalence of GW types in the CC GW crossing success group. The ratio of the numbers of GW types used (SUOH 03, SION, and XTR; Asahi Intecc, Nagoya, Japan) was 89.4%. A smaller number of XTR GWs was used in non-septal CCs. CC: collateral channel; GW: guidewire
SUB-ANALYSES FOR CC PERFORATION REQUIRING TREATMENT
Sub-analysis of the non-septal category was performed for estimating complications. The rate of occurrence of septal, epicardial, and AVG CC perforations was 1.3%, 6.4%, and 16.7%, respectively, with statistical significance. Epicardial and AVG CC variables were analysed by a multivariable analysis for CC perforation requiring treatment in all CCs. The value of the odds ratio of epicardial and AVG CC was 5.12 and 15.00, respectively, with statistical significance. Multivariate analyses were performed for the angiographic variables in the epicardial and AVG CC categories. This analysis revealed that the morphology of the reverse bend in AVG CC was an independent predictor of CC perforation requiring treatment (Table 7).
Discussion
CC GW crossing success is a key stage of retrograde CTO-PCI4. However, only a few studies have examined interventional CCs. Previous reports have suggested that predictors of CC GW crossing success were vessel size, tortuosity, side branch at CC tortuosity, and inadequate CC exit locations8,9, because, in the actual procedure, CC tortuosity and subset are important issues for GW passage. In this study, variables of the angiographic anatomical findings of the CC subset, especially details of tortuosity (Figure 1), were investigated.
Our study revealed new evidence that the angiographic findings that affected CC GW crossing had differences between septal CCs and non-septal CCs (Table 5). The values of the beta coefficient were developed to address the difficulty in estimating the score for CC GW crossing success. For convenience of clinical usage, the scoring model was adjusted (Figure 5). However, the examination of the area under the ROC curve in the derivation and validation sets for each type of CC showed positive results (Figure 2). Although each CC had a complex anatomy, this score simplified anatomical information.
Figure 5. Summary of the J-Channel score. The J-Channel score as a difficulty estimating tool for CC GW crossing success from the Japanese CTO PCI Expert Registry. CC grades (CC0-2) were proposed by Werner13. CC: collateral channel
The examiners in the Japanese CTO PCI Expert Registry had the required experience and options for devices. This score depicted the difficulty of CC GW crossing success and did not predict the success rate.
SEPTAL CC SUBSET
The variable of the small channel was a strong factor compared with other variables (Table 5). From the analysis of GW trends, the XTR GW showed a strong relationship with the small vessel size CC (Table 6). The ratio of XTR GWs used in septal CC was higher than in non-septal CC (Figure 4). The use of this type of GW posed a risk of vessel perforation, because of its tapered tip and polymer jacket, and even its low tip load. Conversely, the frequency of occurrence of CC perforation requiring treatment was significantly low in the septal CC subset compared with non-septal CC (Table 2). As reported by a previous study15, we found septal CC to be safe. On the basis of this result, if there was no difference in the difficulty for estimating the CC GW crossing success between septal and non-septal CC, the preference in terms of safety would be septal CC.
NON-SEPTAL CC SUBSET
Small vessel size, reverse bend, and corkscrew were factors affecting prediction. In the non-septal CC subset, the odds ratio of small vessel size was 11.40. Conversely, in the septal CC subset, the odds ratio of small vessel size was 8.09 (Table 5). We hypothesised that examiners tended to use an XTR GW with a small vessel (Table 6); however, cardiac tamponade easily occurred with perforation in the non-septal CC16. Therefore, examiners may have avoided the use of XTR for small vessels in non-septal CCs. For these reasons, the factor of small vessel size was a stronger predictor for non-septal CC than for septal CC. The factor of corkscrew shape was not significant in septal CCs. Generally, non-septal CCs were longer than septal CCs. Similarly, other characteristics of non-septal CCs may be involved in the factor of corkscrew shape. Further research is needed to confirm these points. Continuous bends were not a significant factor in non-septal CCs. One reason was that the bending part in non-septal CCs was easily straightened when GWs or MCs were inserted.
COMPLICATIONS AND AVG CCS
In the AVG CC category, the complication of CC perforation requiring treatment occurred with a significantly high ratio (16.7%), and the odds ratio was significantly higher than in the epicardial CC subset (15.00 vs 5.12). We expected vulnerability of AVG CCs. The reverse bend variable of AVG CCs was a significant factor for CC perforation requiring treatment (Table 7). AVG CCs with a reverse bend had a significant risk of perforation requiring treatment. There was a tendency to apply SUOH 03 GWs in reverse bends in the successful CC GW crossing group (Table 6). The low tip load (0.3 gf) of SUOH 03 GWs may function safely in a reverse bend.
Limitations
This study is based on a multicentre registry. Therefore, it involves bias in case selection, examiner skill, and institution. Moreover, this registry does not include any standardised CTO-PCI procedure. Therefore, each case involves selection bias with respect to the retrograde procedure, CCs, and devices. The primary endpoint is not CC MC crossing success or CTO-PCI technical success. However, in this study, the CTO-PCI technical success rate after CC GW crossing success was reasonable (91.0%). Regarding the evaluation of CC complications, the frequency of CC perforation requiring treatment was not equal to clinical cardiac tamponade or other clinical major complications. Even though an experienced CTO examiner observed angiographic findings, there was a possibility of variability in angiographic evaluation. The angiographic findings of CCs were based on tip injection findings. There was a possibility of wire passage through CCs without tip injection. In this study, native CCs were investigated. There is a limitation for estimating bypass graft CCs. In the GW evaluation, only final GWs were investigated. There is a possibility that initial or second GWs were not investigated. Because CC GW crossing success is closely related to GW technology, further validation is needed to confirm the effects of future GWs.
Conclusions
The J-Channel score as a prediction tool based on angiographic findings for each type of CC can be used for judging the difficulty of CC GW crossing success with retrograde CTO-PCI.
|
Impact on daily practice We created a prediction score model (J-Channel score) for measuring the difficulty of CC GW crossing success in retrograde CTO-PCI. The angiographic findings, which affected CC GW crossing, had differences between septal CC and non-septal CC. The proposed scoring model can evaluate the difficulty of CC GW crossing success by angiographic findings for each type of CC, and information about difficulty can be shared with examiners for appropriate selection of CCs. |
Acknowledgements
The authors dedicate this paper to the late Dr Kazuaki Mitsudo. The authors appreciate the clinical research coordinators and the doctors participating in the Japanese CTO PCI Expert Registry: Tomohiro Kawasaki, Yuji Hamasaki, Atsunori Okamura, Koichi Kishi, Toshiya Muramatsu, Yoshito Yamamoto, Satoru Otsuji, Tsutomu Fujita, Yoshihisa Kinoshita, Yoshiki Uehara, Takeshi Serikawa, Shinya Okazaki, Fumitaka Hosaka, Kenya Nasu, Shigeru Nakamura, Akitsugu Oida, Yoshihiro Takeda, Makoto Sekiguchi, Yuichi Kobori, Toru Takahashi, Takenori Shibata, Masahisa Yamane, Kenichiro Shimoji, Masaki Tanebe, Yosiaki Ito, Yuichi Noguchi, Kazuhiro Ashida, Kaname Takizawa, Eisho Kyo, Kenji Kawajiri, Kinzo Ueda, Yasushi Asakura, Masakazu Nagaoka, Hiroyuki Tanaka, and Jiro Ando.
Funding
This study was funded by the Japan Chronic Total Obstruction Intervention Specialist Council that is funded by Asahi Intecc, Abbott Vascular Japan, Biosensors Japan, Boston Scientific, Daiichi Sankyo, Kaneka, Medtronic Japan, Nipro, and Terumo.
Conflict of interest statement
W. Nagamatsu is a consultant for Asahi Intecc, Abbott Vascular Japan, Terumo, Medtronic Japan, Boston Scientific Japan, Kaneka Medics, and Nipro. E. Tsuchikane is a consultant for Boston Scientific Japan, Asahi Intecc, Nipro, and Kaneka Medics. S. Sumitsuji is a consultant for Terumo, Kaneka Medics, Nipro, Asahi Intecc, Abbott Vascular Japan, Boston Scientific Japan, Medtronic Japan, Biosensors, and OrbusNeich, has received grants from Terumo, Kaneka Medics, Nipro, and Asahi Intecc, has received personal fees from Abbott Vascular Japan, Boston Scientific, Medtronic Japan, Biosensors, OrbusNeich, Amgen Astellas BioPharma, Daiichi Sankyo, Shionogi, Takeda Pharmaceutical, Heart Organization, Sumitomo Dainippon Pharma, Hokushin Medical, Canon Medical, Fujifilm Medical, Shimadzu, Bristol-Myers Squibb, Boehringer Ingelheim, Sanyo Chemical Industries, and Siemens Healthcare. O. Kato is a consultant for Asahi Intecc and Nipro. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.