Abstract
Aims: Septal surfing and distal tip injections are two techniques used for septal crossing in retrograde chronic total occlusion (CTO) percutaneous coronary interventions (PCI). The aim of this study was to examine for the first time the safety and feasibility of the septal surfing technique.
Methods and results: Among 470 consecutive CTO PCIs performed in the Quebec hybrid CTO PCI program between January 2010 and December 2015, 240 (51%) involved a retrograde attempt. In the septal crossing subgroup, we evaluated whether the Werner collateral channel (CC) classification, CTO location, tortuosity, and number of large septal CCs influenced retrograde crossing success, time, and perforation. Septal channels were used in the majority (n=152, 63%) of cases. Patients in the septal subgroup were younger, had less bypass surgery, were more likely to have RCA CTO and had previous failure. Septal channels were successfully crossed with the wire using the surfing technique in 81%, irrespective of the CC size. Septal crossing success and time were not influenced by Werner CC class but by septal CC tortuosity. One quarter of cases had septal perforations; all were minor and asymptomatic.
Conclusions: Septal surfing is a safe and highly successful technique for crossing septal CCs when a retrograde approach is mandated for CTO PCI. The Werner class does not affect retrograde CC crossing success or time.
Abbreviations
CABG: coronary artery bypass grafting
CC: collateral channel
CTO: chronic total occlusion
DTI: distal tip injections
J-CTO score: Japanese-Chronic Total Occlusion score
PCI: percutaneous coronary intervention
SST: septal surfing technique
WW: workhorse wire
Introduction
Based on the hybrid chronic total occlusion (CTO) percutaneous coronary intervention (PCI) algorithm1, the retrograde approach is preferred in the presence of an ambiguous proximal CTO cap, distal vessel disease or a major bifurcation at the distal cap. However, this is conditional on the identification of potential pathways to reach the distal CTO cap2.
When selecting a retrograde route to the distal CTO cap, a preference is usually given to septal collateral channels (CCs)3,4, which are considered safer than epicardial CCs. A recent systematic review and meta-analysis showed that the retrograde approach in selected patients can significantly enhance CTO PCI success with a low risk of serious procedural complications5. The advent of the Corsair microcatheter (ASAHI Intecc, Aichi, Japan) has also revolutionised CC crossing in retrograde CTO PCI6. Currently, there are two schools of septal crossing, the Japanese and the Western. The original Japanese method involves selecting a CC that has a higher likelihood to connect, and relies on sequential distal microcatheter tip injections in order to visualise and isolate a connecting CC, with subsequent attempts to cross the identified CC with a dedicated wire. Another method, first described by Sianos7, is termed the “septal surfing technique” (SST) whereby the wire probes septal CCs by “trial and error” without distal tip injections (DTI), in search of a path of low resistance. While the ability to visualise a connecting CC was described as being a key factor with the Japanese technique8, its impact on CC crossing with the SST is unknown. We therefore present our six-year experience with retrograde techniques. We compared cases where a septal channel was used vs. other retrograde pathways (epicardial CC or grafts)9. We hypothesised that the visualisation of a continuous connection between the donor and recipient vessel is not associated with improved septal CC crossing or a shorter time when using SST.
Methods
STUDY POPULATION, VARIABLES AND OUTCOMES DEFINITION
Between January 2010 and December 2015, 470 consecutive cases were performed in the Quebec hybrid CTO PCI program. A case was considered retrograde when a wire was used to attempt crossing a CC or a vein graft9, successfully or not. We collected features of the CTO that mandated a retrograde approach as per the published hybrid algorithm1. We also assessed the Werner class of the dominant collateral and the class of the CC that was finally crossed through prospective (by S. Rinfret) and detailed retrospective angiographic review (by R. Dautov). The Werner classification identifies collaterals as either without visible connection with the recipient vessel (CC0), as thread-like tiny vessels (CC1) or as small vessel-like channels (CC2) (Figure 1). To assess the CC class of crossed septal CC, we compared the course of the wire with the most likely collateral crossed on the baseline angiography at the time of PCI. If no connection was visible in the trajectory of the wire prior to crossing, we considered that a CC0 was traversed. In the case of failed connection, we considered for analysis the largest attempted collateral. We also assessed the Japanese-Chronic Total Occlusion (J-CTO) score10,11. For the purpose of identifying factors associated with higher retrograde CC crossing success using the SST, we analysed angiographies for the presence of the following factors: location of the CTO (left anterior descending artery [LAD] vs. non-LAD), tortuosity of the attempted channel in its visible portion and the number of CC2 connections. A CC was crossed successfully when the wire was placed at the distal CTO cap. We also assessed the proportion of those cases where the microcatheter followed to the distal cap with success.
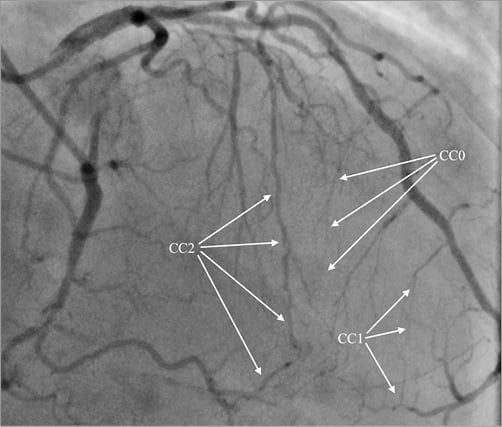
Figure 1. Werner’s classification of collateral channels. Collateral channel (CC) grades by Werner: CC0 - no continuous connection; CC1 – thread-like continuous connection; CC2 - side branch-like connection.
Baseline, procedural and hospitalisation data were prospectively collected and entered into a dedicated database. Data collection was approved by our institutional review committee as part of the Recherche Évaluative en Cardiologie InTerventionnelle (RÉCIT) registry and subjects provided signed informed consent. The feasibility endpoints were defined as successful CC crossing as well as the time to perform CC crossing. The safety endpoints were defined as events related solely to septal channel crossing and comprised intraprocedural complications (septal channel perforations, septal haematomas requiring specific treatment, pericardial effusion or tamponade) and donor-artery dissection or thrombosis. We also assessed the ability to place a microcatheter at the distal CTO cap, final technical success of the procedure, defined as the ability to open the CTO, and other performance variables, such as contrast use and radiation dose.
RETROGRADE COLLATERAL CHANNEL CROSSING TECHNIQUE
Once the retrograde approach is justified either as a primary strategy or after a failed antegrade attempt, we usually rely on 6 Fr guide catheters from the retrograde side, most of the time delivered transradially. Epicardial collaterals are invariably crossed with a soft wire, currently with the SION™ (ASAHI Intecc) guidewire, tracking the channel slowly and precisely based on the known anatomy, with the microcatheter following closer to the tip of the wire. DTI are frequently employed.
Septal CC surfing is, however, different. The microcatheter is advanced on a workhorse wire (WW) into the proximal part of one of the septal branches from the LAD for a right coronary artery (RCA) or dominant left circumflex (LCx) CTO, or in the posterior descending artery (PDA) for a LAD CTO. Following WW removal, we introduced up to March 2012 a Fielder FC wire (ASAHI Intecc) and after March 2012 a SION with a single 30-45° bend at 1 mm from its distal tip. The wire is quickly advanced and pulled back when a resistance is felt, and redirected into a different channel. Once some buckling is felt, drilling of the wire can lead to passage into the recipient vessel. This technique offers the advantage of testing several options of crossing from one proximal septal trunk from the LAD, or to engage small distal septals when surfing from the PDA. When surfing from the LAD, if the operator fails to connect from a given septal, the microcatheter is pulled, and a different septal is then engaged with the WW shaped appropriately for the proximal septal angulation. After the microcatheter advancement, the new septal branch with its CCs is “surfed” again with the SION wire. A good septal track to the recipient vessel can be identified when a repetitive course of the wire is noticed while pulling and pushing: if the wire keeps on making similar turns, it probably tracks a vessel structure that may finally connect, even if originally invisible on angiography. It is then advanced to the point of resistance and drilled at this level, seeking a release into the recipient vessel. The feeling is often of a free wire that tracks the PDA or LAD nicely, and engages branches before reaching the distal CTO cap. The difficulty in navigating the wire is usually located close to the PDA; therefore, when surfing from the LAD to the PDA, challenges will be encountered most of the time at the end of the course of the wire within the septum, where septal channels become very small. The opposite is true when surfing from the PDA: challenges come early in the course. When the wire crosses a small septal close to the PDA and feels free in a vessel structure afterwards, it is usually easy to advance the wire as the septals get larger close to the LAD. The wire can easily track into one of the two ventricles; this is benign as long as the microcatheter does not follow. With heart beats, a to-and-fro movement of the wire can be seen in the recipient vessel when successfully placed. DTI was not performed as a primary strategy; however, in case of failed SST, DTI was performed to help track potentially larger branches or understand the mode of failure, such as hidden tortuosity. A retrograde angiography is performed before advancing the Corsair (or other microcatheter such as the Turnpike® or Turnpike® LP; Vascular Solutions, Minneapolis, MN, USA) through the CC, which can sometimes need extra support from a mother-and-child catheter (5.5 Fr GuideLiner®; Vascular Solutions). We tend to avoid crossing dominant septal CCs: in case of damage, the CTO territory can become ischaemic (Figure 2, Moving image 1-Moving image 3).
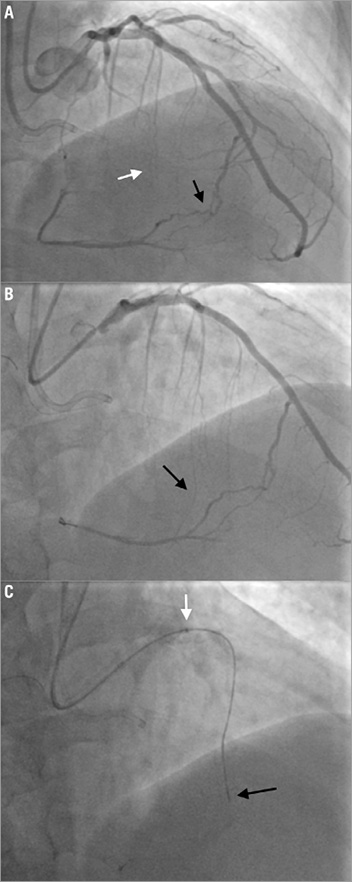
Figure 2. Septal surfing through invisible septal CC. A) Very large but tortuous CC2 septal visualised from the LAD to the PDA (black arrow). There are other septal branches that give CC0 collateral channels (white arrow). B) After five minutes of surfing of one of the most proximal septals (black arrow) with a SION through a Finecross® (Terumo Corp., Tokyo, Japan), a connection to the PDA was achieved. C) The Finecross is exchanged for a Corsair (black arrow), which is advanced through the septal CC with the support of a 5.5 Fr GuideLiner catheter (white arrow).
STATISTICAL ANALYSIS
Binary variables were expressed as percentages and continuous variables as mean values and standard deviation (SD) or standard error of the mean (SEM) when in figures. We first divided our sample into two groups: cases where a septal was crossed or attempted vs. those where an epicardial CC or a vein graft was used as a retrograde pathway. We compared several clinical and angiographic characteristics as well as procedure outcomes when using either approach. Pairwise comparisons were performed using the chi-square test for discrete data, and t-tests for continuous variables, after confirming a normal distribution. Pairwise comparisons are presented with p-values. We assessed the univariate predictors of retrograde wiring time, and compared times with t-tests or analysis of variance when there were more than two groups. Finally, we assessed, among the septal subgroup of cases, the association between the Werner CC class and successful retrograde CC crossing or successful CTO recanalisation, using the Mantel-Haenszel trend test, assuming an increasing probability from CC0 to CC2. Using successful retrograde CC crossing as the dependent variable, we performed multiple logistic regression analysis to assess the adjusted contribution of the Werner class and other factors, and linear regression modelling for retrograde wiring time as a dependent variable, with the same independent a priori selected factors. A p-value <0.05 was considered statistically significant. No adjustments were made for multiple comparisons. All analyses were conducted using SAS 9.3 (SAS Institute, Cary, NC, USA).
Results
COMPARISON OF RETROGRADE CASES THROUGH SEPTAL CCs VS. OTHER RETROGRADE PATHWAYS (Table 1)
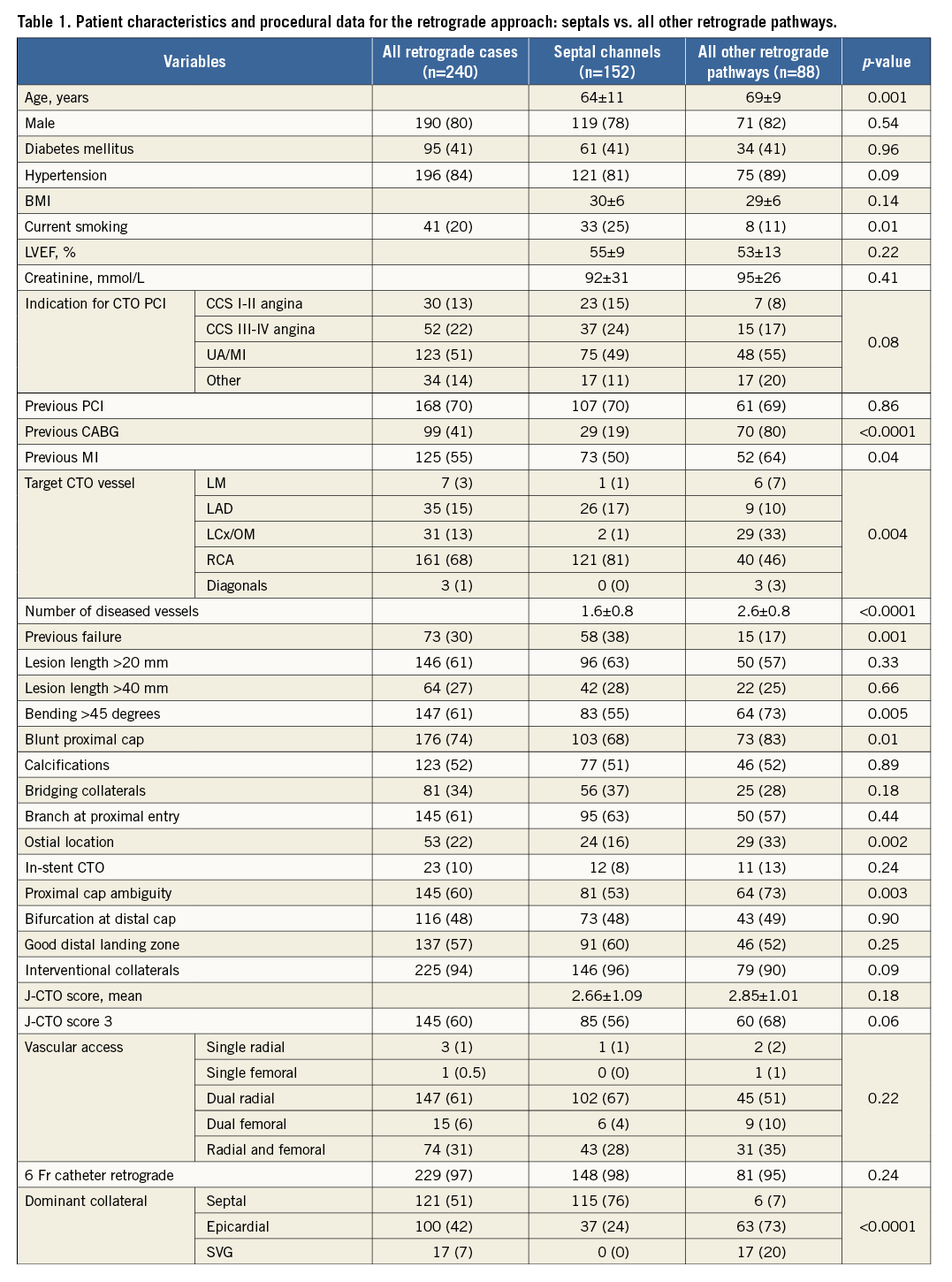
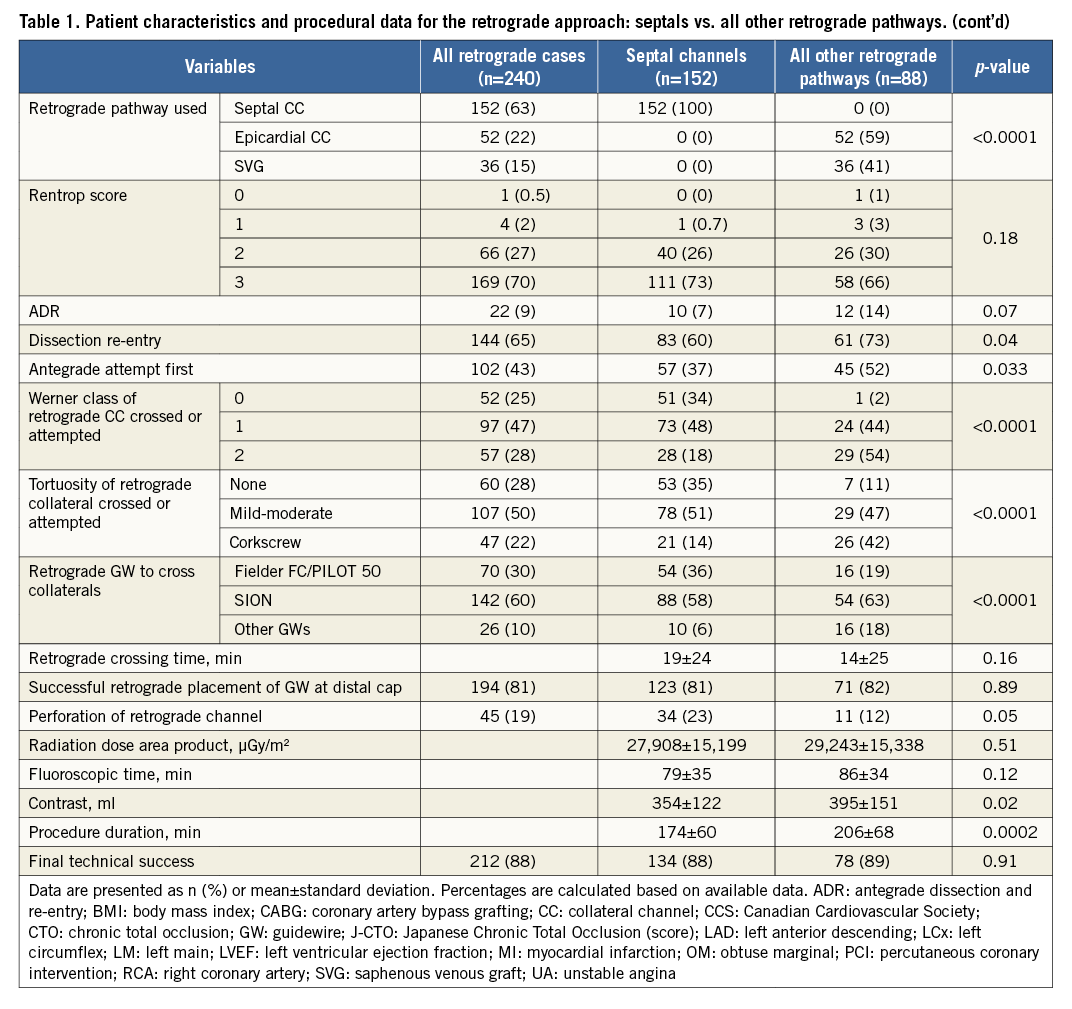
A total of 240 retrograde CTO cases were classified into two subgroups: the septal subgroup, where septal CCs were crossed or attempted (n=152; 63%), and the “all other retrograde” subgroup, including epicardial CCs and bypass grafts (n=88; 37%). Among the latter, epicardial CCs were utilised in 59% of cases and bypass grafts in 41%9.
Patients in the septal subgroup were younger (64 vs. 69 years; p=0.001), while the prevalence of previous coronary artery bypass grafting (CABG) was significantly lower than for the other retrograde subgroup (19% vs. 80%; p<0.0001). Meanwhile, the septal subgroup had more previous failed attempts (38% vs. 17%; p=0.001). Regarding lesion characteristics, those attempted via septal channels were less angulated (55% vs. 73%; p=0.005), less often had a blunt proximal cap (68% vs. 83%; p=0.01) or proximal cap ambiguity (53% vs. 73%; p=0.003), and had a lower proportion of very difficult lesions (J-CTO ≥3) (56% vs. 68%; p=0.06). An ostial location of the CTO was more common when other retrograde pathways were used (33% vs. 16%; p=0.002). Septals were more frequently used for RCA CTO, whilst other retrograde pathways were more frequently used for LCx CTO (p<0.004). Septal collaterals were dominant in the majority of septal cases, whilst epicardials were dominant in other retrograde cases (p<0.0001). The procedure was less likely to start antegradely in the septal subgroup (p=0.033). Septal cases had more perforations (23% vs. 12%; p=0.05), but the procedures were shorter in duration (174 vs. 206 min; p=0.0002) and required less contrast (354 vs. 395 ml; p=0.02). Final technical success was similar in both subgroups.
SEPTAL SUBGROUP ANALYSES
In all but four cases, when a wire crossed the septal to the distal cap, the microcatheter successfully followed (119/123; 97%). By univariate analysis, using the Mantel-Haenszel trend test, the Werner CC class was not associated with increased retrograde CC crossing success, or with improved final technical success (Figure 3A). However, increasing septal tortuosity was significantly associated with a lower retrograde CC crossing success and with a lower technical success (Figure 3B). Crossing a septal from the LAD to the PDA vs. from the PDA to the LAD was associated with a trend towards improved success (83% vs. 71%, p=0.11). The Werner class or tortuosity of the attempted septal CC did not affect the risk of septal perforation (Figure 3A, Figure 3B). The number of CC2 septals did not predict successful retrograde wire placement, nor did it affect the final technical success or septal perforation rate (Figure 3C). When DTI was employed in addition to SST, the likelihood of septal crossing was lower (64% vs. 88% without; p=0.001), and the risk of perforation higher (54% vs. 20%; p=0.02). Successful CC crossing was associated with higher final technical success as compared to failed CC crossing (97% vs. 52%; p<0.0001).
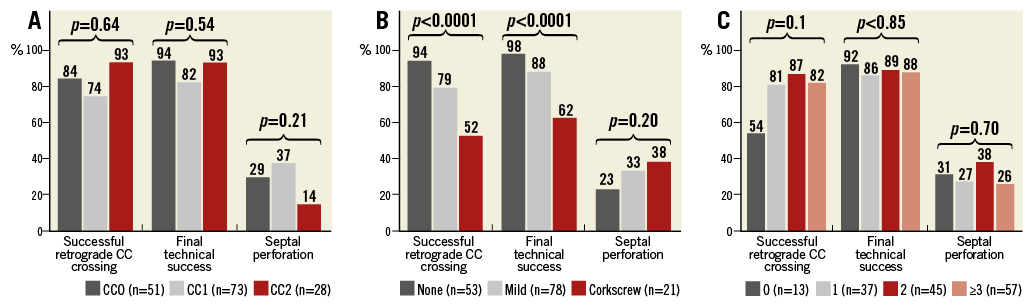
Figure 3. Univariate analysis of factors influencing successful retrograde CC crossing, final technical success, and septal perforations. Incidence of retrograde septal CC class (A), septal channel tortuosity (B), number of potential interventional CC2 septals (C).
When using collateral crossing time (in minutes, up to success or failure), we found that septals with an invisible connection (CC0) and large septals (CC2) were crossed faster than thread-like ones (CC1) (Figure 4). Septal tortuosity significantly affected septal crossing time (11 min if straight vs. 42 min when there was corkscrew-like tortuosity; p=0.0023). When DTI was performed in addition to SST, the septal crossing time was extended from 14 to 34 min (p=0.0019). Use of the SION wire (used in all patients after March 2012) was associated with a trend towards improved crossing success compared with polymer-jacket wires (85% with SION vs. 75% with HI-TORQUE PILOT® 50 [Abbott Vascular, Santa Clara, CA, USA] or Fielder FC; p=0.11). Moreover, use of the SION (also in a later period) was associated not only with a strong trend towards lower perforation (18% with SION vs. 31% with PILOT 50 or Fielder FC; p=0.07), but also with a significantly lower time to cross the septal (13±21 min vs. 28±27 min; p<0.001).
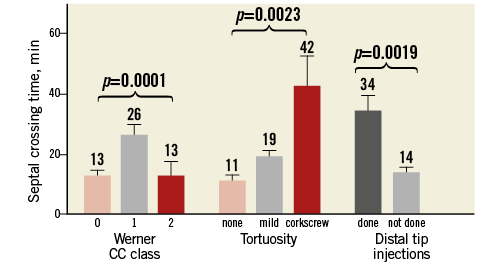
Figure 4. Angiographic and procedural factors affecting septal crossing time when primarily using a surfing technique first. CC: collateral channel
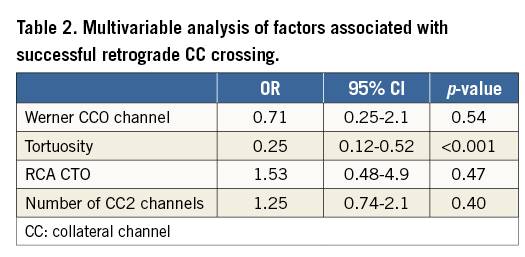
MULTIVARIATE ANALYSES
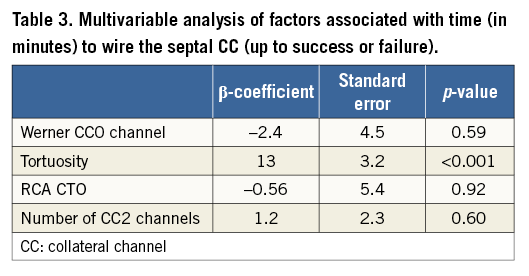
Given the non-linear effect of the Werner CC class on successful retrograde crossing, we dichotomised CCs into invisible connections (CC0) vs. visible ones (CC1 or CC2), for subsequent modelling. When adjusting for a priori selected factors believed to affect successful CC crossing, an invisible connection (CC0) was not significantly associated with reduced success to traverse the collateral channel successfully (OR 0.71, 95% CI: 0.25-2.1, p=0.54) (Table 2). However, tortuosity significantly reduced the chance to connect to the distal cap (OR 0.25, 95% CI: 0.12-0.52, p<0.001). When modelling time to wire the septal CC, again only septal tortuosity was significantly associated with increased time (Table 3).
SAFETY ENDPOINTS
Donor artery dissection or thrombosis occurred in 4.5% of all retrograde cases, and did not differ if the collateral crossed was a septal or another route. All cases were successfully treated with thromboaspiration, with or without stenting.
There was a total of 34 septal channel perforations (22%) in 152 retrograde septal CTO cases. All of these perforations were benign. Among these complications, septal staining <2 mm was noted in 25 cases. Six of them had sealed spontaneously by the end of the procedure. Contrast stains ≥2×2 mm (also called “septal contrast lakes”) were noted in five cases and remained unchanged throughout the case. There were four perforations into cardiac chambers during SST. One of them was not visualised anymore on final angiography. As a result of SST or microcatheter placement to the distal cap of a CTO, there were no cases of pericardial effusion, tamponade or septal haematoma requiring specific treatment. No patient presented life-threatening ventricular arrhythmia.
Discussion
The main finding of the present study is that the SST is safe and feasible when attempting retrograde CTO PCI and is associated with high collateral crossing success regardless of the angiographic appearance of collateral connections as per the Werner classification12. In our study, even Werner CC0 (invisible septals) were often attempted, and were crossed with as much success as larger CCs, and even faster. The Corsair was able to track and dilate channels in the vast majority of cases where the guidewire had crossed the septal channel. Although septal perforations were invariably benign, retrograde cases were associated with some donor artery trauma (often not specifically reported in retrograde series) which, fortunately, were all successfully treated with no further complication. Finally, our data suggest that the use of the SION guidewire is associated with better outcomes (less perforation, shorter crossing time) compared to polymer-jacket wires when performing the SST.
Only a few studies have evaluated predictors of retrograde CTO PCI success. In a smaller, single-centre Japanese study of 157 patients, including 106 septal CCs, Rathore et al8 identified the absence of any visible connection (CC0) as a predictor of failure. However, we could not replicate those findings, probably because of the fundamental difference between CC crossing techniques. Also, the advent of the microchannel dilator may have contributed to our higher retrograde success rate. Indeed, in a large recent CTO registry from Japan, Corsair microcatheter use was the only factor associated with successful retrograde CTO recanalisation3. Further improvement in microcatheter technology, with the advent of smaller profile microcatheters, is likely to translate into sustained or improved performance.
The fact that invisible septals were crossed with as much success as larger CCs, and even faster, merits some discussion. Our hypothesis is that CC0, even though invisible, are often straighter and have a more direct course. The crossing time of CC0 was equal to CC2, where visible and straighter connections guaranteed smooth crossing at the price of possible ischaemia related to the obstruction/perforation of a large collateral. CC1, on the other hand, we crossed with less success and more time. We think this might be attributable to the fact that the transition from larger parts of the connection to smaller parts may hide tortuous segments that are difficult to cross.
This series of consecutive patients had the highest proportion of retrograde approach (51% of total CTO cases) published to date. As a comparison, Werner et al13 used the retrograde approach in 27% of patients and Christopoulos et al14 in 44%. Cases treated from the retrograde approach appear to have had many factors justifying the way we selected to proceed. Given that more than 80% of cases were referred to the programme, either primarily or after a failure (in 30%), some referral bias towards more difficult cases may explain this particularity. We can also speculate that the SST and its success may have lowered our threshold to use the retrograde approach, even in cases without obvious interventional CCs.
Even though perforation of an epicardial CC can be successfully managed percutaneously or conservatively in most cases15, such a complication can potentially lead to emergency surgery or even death. While 1/4 of cases in our SST cohort had septal perforations, they were minor and asymptomatic. This finding confirms that septal CCs are safer to use than epicardial CCs, and should be used preferentially, even when barely visible. Indeed, we elected to cross septal CCs as a safer alternative even if 24% of our cases had dominant epicardial collaterals. Although additional DTI can be useful to guide navigation of tortuous septal CCs, as used in 27% of our cohort, we believe that the systematic use of upfront DTI confers no significant advantage over a simpler and safer SST first, and could be associated with a higher risk of hydraulic septal perforation. However, DTI were performed in cases with a difficult retrograde connection; therefore, DTI following SST is probably a marker of a more difficult CC crossing attempt, and our analysis is certainly not a direct comparison of the two techniques.
Limitations
Our study has limitations. First, it is a single-programme series, which may have been influenced by local operators’ skills and experience. Nevertheless, the SST has been adopted by many operators in the western world, and yet no data were available on the effectiveness of the method. Second, although this series constitutes the largest study to date on the subject of retrograde crossing per se, it is still limited by the sample size, with only a few factors allowed into the models. Third, no angiographic core lab was used. However, most observational CTO PCI studies do not report core lab assessments. Finally, our analyses suggest that the SION wire may be a better wire for the SST compared to first-generation polymer-jacket wires, such as the PILOT 50 or the Fielder FC. However, such a comparison may be biased, as the SION was used at a later stage in the experience.
Conclusions
In conclusion, the SST for retrograde CTO PCI appears to be simple and relatively safe when a retrograde route is considered to be the best approach. It is associated with a high success rate, regardless of the Werner CC class. Small septal channels (CC1) or even invisible septals (CC0) can often be crossed with the wire. Once the guidewire is at the distal CTO cap, the microcatheter is able to follow in the vast majority of cases. Surfing CC0/CC1 septals rather than CC2 in order to avoid ischaemia during crossing of collaterals or in case of perforation may be safer. Therefore, small or even invisible channels should not discourage an operator from attempting CTO PCI from a retrograde approach when the algorithm suggests it is the preferred direction for a given anatomy. However, operators should keep in mind that retrograde techniques, even when performed with smaller 6 Fr catheters and by experienced operators, remain associated with inherent complications such as donor artery dissection or thrombosis.
| Impact on daily practice This is the first study to demonstrate the safety and feasibility of septal surfing for crossing septal collateral channels in comparison with other retrograde options. Furthermore, we show that the technique is highly effective to cross invisible channels and should encourage CTO operators to attempt crossing septal channels when a retrograde approach is needed. The availability of new soft wires (e.g., SION black and SUOH [both ASAHI Intecc]) and lower profile microcatheters (e.g., Caravel from ASAHI Intecc, or TurnPike LP from Vascular Solutions) should further improve our findings. |
Conflict of interest statement
S. Rinfret has received speaker and proctorship honoraria from Boston Scientific, Abbott Vascular Canada, Medtronic Canada and Terumo USA. He has received research support from Medtronic and Abbott Vascular. The other authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Septal network.
Moving image 2. Septal surfing.
Moving image 3. Advancement of the Corsair through the septal channel.
Supplementary data
To read the full content of this article, please download the PDF.
Septal network.
Septal surfing.
Advancement of the Corsair through the septal channel.