It is becoming increasingly clear that posterior pericardiotomy (PP) (Figure 1) may have a central role in reducing postoperative atrial fibrillation (POAF), the most frequent complication in patients undergoing cardiac surgical procedures1. A growing body of clinical and experimental data suggest that − excluding genetic predisposition, pre-existing and surgical-related factors − POAF can be triggered by small amounts of pericardial effusion causing localised inflammation2. By draining the posterior pericardium34, PP redirects pericardial fluids and blood clots to the left pleural space, minimising the potential development of a highly pro-oxidant and proinflammatory microenvironment within the pericardial sac in the early postoperative phase5.
In this issue of EuroIntervention, Abdelaziz and colleagues reaffirm the safety and efficacy of such a simple intervention in a new meta-analysis summarising the available randomised evidence on the role of PP in cardiac surgery6. In their study including 4,467 patients from 25 randomised trials (RCTs), the authors found that PP significantly reduced the incidence of POAF compared to no intervention (odds ratio [OR] 0.49, 95% confidence interval [CI]: 0.38-0.61) but at the cost of an increased rate of pleural effusion in the intervention group (OR 1.34, 95% CI: 1.12-1.61). No difference in pulmonary complications was observed between the groups (OR 1.14, 95% CI: 0.85-1.52). Early (OR 0.32, 95% CI: 0.22-0.46) and late pericardial effusion (OR 0.15, 95% CI: 0.09-0.46) were also found to be significantly reduced in the PP group, testifying to the presence of a direct association between pericardial effusion and POAF. The beneficial effect of PP on POAF remained even after removing studies with preoperative use of β-blockers, those with less than 100 patients, or stratifying for type of surgery.
However, when pooling estimates by geographical areas, the reduced incidence of POAF in patients receiving PP remained evident only in RCTs originating from Turkey and Egypt; those conducted in Asia or Europe/North America did not reach statistical significance, though a trend favouring PP was clearly visible. These contradicting results can be explained by either the lack of RCTs (Europe/North America) or the prevalence of underpowered and/or poorly designed RCTs. Given the relevance of the topic, the fact that most of the randomised data included in this as well as other analyses originate from Turkey, Egypt, and different countries in Asia has been at the centre of the debate for many years, even more so considering that only a few RCTs were adequately powered to detect any treatment effect. However, this is a very well-known methodological issue that does not seem to belittle the strength of the generated evidence, which undoubtedly points to an early clinical advantage for patients receiving PP. Overall, the authors must be congratulated on having produced results which are consistent with previously published study-level meta-analyses and of great clinical value, despite using a different search strategy78. As mentioned above, the small sample sizes appeared to be the main limitation of the studies included in the analysis. In addition, most RCTs adopted a single-centre design, and many investigated the impact of PP on individuals undergoing elective isolated coronary artery bypass grafting. Of note, none of them reported mid- or long-term follow-up. That being said, a closer look needs to be taken at the study by Gaudino and colleagues, the first PP-related RCT conducted in the USA and one of the most recently published RCTs included in the meta-analysis9.
The PALACS trial (The Effect of Posterior Pericardiotomy on the Incidence of Atrial Fibrillation After Cardiac Surgery) is an adequately powered RCT which compared PP to no intervention in 420 patients undergoing elective interventions in the coronary arteries, aortic valve, or ascending aorta (or a combination of such interventions). Of these, 212 were randomly assigned to the PP group and 208 to the no intervention group. The authors found that the incidence of pericardial effusion (12% vs 21%; relative risk 0.58, 95% CI: 0.37-0.91) and POAF (17% vs 32%; adjusted OR 0.44, 95% CI: 0.27-0.70) was significantly lower in the PP group than in the no intervention group. In addition, the time added to surgery was minimal, and no complications were seen. Interestingly, a recent post hoc analysis of the PALACS trial has shown that PP reduces POAF especially after postoperative day 2, suggesting that earlier POAF episodes are mostly due to a pre-existing arrhythmogenic substrate10. Overall, the results of this RCT seem to suggest that PP should be considered during most cardiac surgery operations. However, the authors excluded patients at relatively high risk of developing POAF, such as those undergoing mitral or tricuspid valve surgery or with a previous history of atrial arrhythmias. Other important limitations were the single-centre design, as well as the fact that the study was not powered to detect differences in clinical outcomes between the groups9.
Consequently, to confirm the potential clinical benefits of PP, a large, multicentre RCT including the entire spectrum of cardiac surgery procedures (EPIC Trial: Effect of left posterior Pericardiotomy In Cardiac surgery) was designed by the same principal investigator and awaits formal clearance from authorities. The goal of this RCT is to assess the effectiveness and safety of PP in preventing POAF and improving early and long-term clinical outcomes, including quality of life. Pending the kick-off of this multicentre RCT whose results could inform our surgical practice, a 1-year and 5-year follow-up to assess differences in clinical outcomes including death, stroke, and cardiac-related readmission is currently being conducted in the two cohorts of patients enrolled in the PALACS trial. At present though, whether the systematic use of PP during cardiac surgery operations translates into better long-term outcomes remains unclear, as no data are available.
To conclude, this simple and safe technique holds the potential to radically change our daily surgical practice and positively impact the already challenging postoperative course of our patients. Yet, to obtain the answers we are all looking for, more time and solid evidence are needed.
Omnia cum tempore.
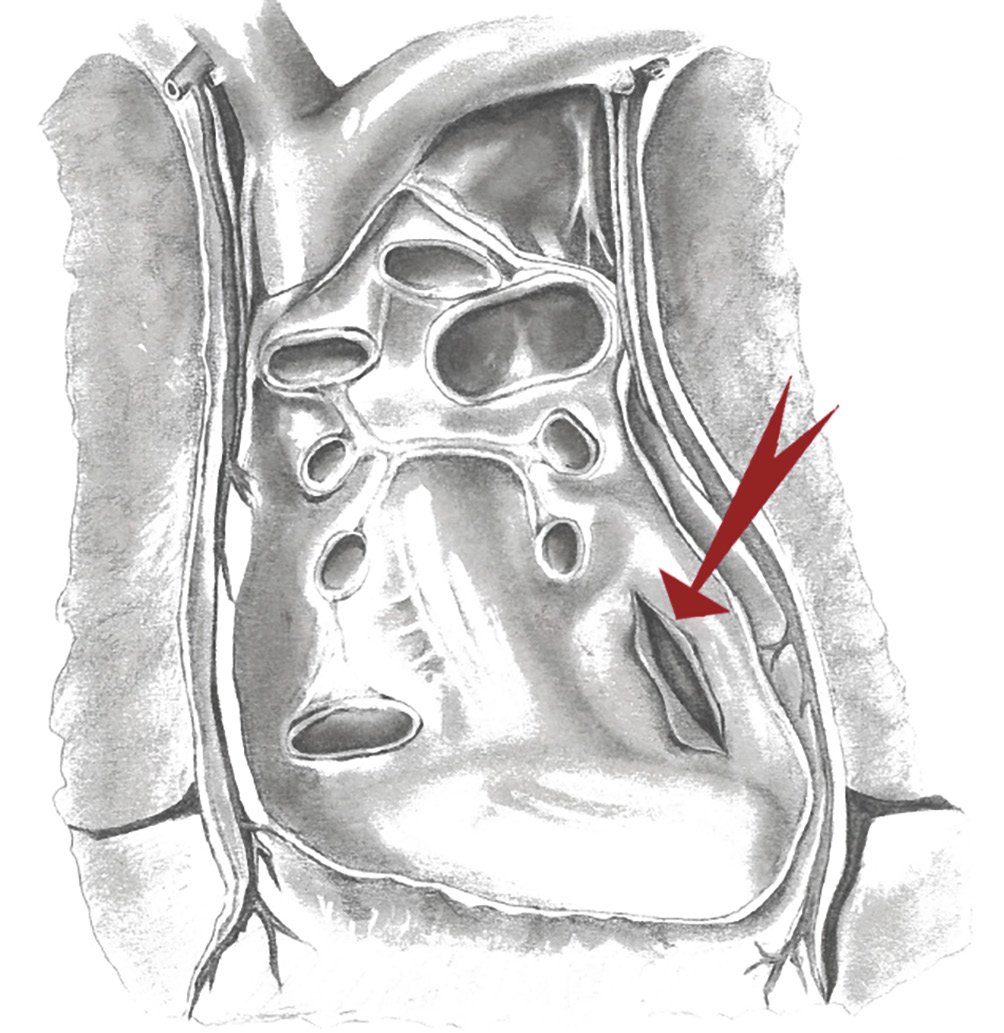
Figure 1. Artist’s representation of the posterior pericardiotomy (red arrow). Artist: Katherine Sokoloff. Reprinted with permission from9.
Conflict of interest statement
S.E. Fremes reports receiving grants as the principal investigator of the ROMA and STICH3C trials from the Canadian Institutes of Health Research; is a site coprincipal investigator of the ACURATE IDE trial from Boston Scientific; and is a site coprincipal investigator of the SURTAVI and Low-Risk trials from Medtronic. M. Gaudino reports research grants from the National Institutes of Health and Canadian Institutes of Health Research; and consulting fees from the Coronary Research Foundation.G. J. Soletti has no conflicts of interest to declare.