Abstract
Aims: Little is known about the prognostic role of pre-existing atrial fibrillation (AF) and new-onset AF (NOAF) in transcatheter aortic valve implantation (TAVI). Therefore, the aim of this meta-analysis was to compare the short- and long-term clinical outcomes of patients undergoing TAVI with and without pre-existing and new-onset AF.
Methods and results: Twenty-six studies, enrolling 14,078 patients undergoing TAVI, of whom 33.4% had pre-existing AF and 17.5% had NOAF, were analysed for early and long-term all-cause mortality, cardiovascular mortality and cerebrovascular events (CVE). In patients with pre-existing AF, 30-day all-cause mortality was similar to patients in sinus rhythm (SR). Conversely, long-term all-cause and cardiovascular mortality were significantly greater in pre-existing AF patients than in patients with SR (20 studies; 8,743 patients; HR: 1.68; p<0.00001, and three studies; 1,138 patients; HR: 2.07; p=0.01, respectively). Pre-existing AF was not a predictor of CVE at long-term follow-up. NOAF patients showed similar short- and long-term all-cause mortality when compared to patients in SR, whereas they experienced a significantly higher incidence of CVE at short-term follow-up (six studies; 2,025 patients; HR: 2.86; p<0.00001). A non-significant increase in the incidence of CVE was observed at long-term follow-up.
Conclusions: Pre-existing AF is a predictor of all-cause mortality in patients undergoing TAVI. NOAF is related to the occurrence of CVE at short-term follow-up. Similarly to surgical aortic valve replacement (SAVR), the optimal management and risk stratification of these patients should be further investigated.
Abbreviations
AF: atrial fibrillation
AS: aortic stenosis
CI: confidence interval
CVE: cerebrovascular events
HR: hazard ratio
NOAF: new-onset atrial fibrillation
SAVR: surgical aortic valve replacement
SR: sinus rhythm
TAVI: transcatheter aortic valve implantation
Introduction
Atrial fibrillation (AF) is the most common arrhythmia in the general population, with a higher prevalence in the elderly as well as in patients with severe aortic stenosis (AS)1. AF and AS coexist in almost 30% of patients, with a prevalence that varies from 16% to 40%2. New-onset AF (NOAF) post transcatheter aortic valve implantation (TAVI), however, occurs in approximately 13% of patients, ranging from 0.7% to 31.9%3.
Pre-existing AF and NOAF significantly affect cardiovascular physiology, due to loss of atrioventricular synchrony and irregularity of ventricular contraction resulting in reduced cardiac output and increased filling pressures, which may be further accentuated by the presence of severe AS and myocardial hypertrophy4. Additionally, the left ventricular outflow obstruction provoked by AS results in left ventricular hypertrophy and diastolic dysfunction, which may itself precipitate AF due to increased left atrial pressures4.
AF has an important impact on cardiovascular morbidity and mortality5. Population-based studies have indicated an increased risk of stroke and systemic embolism as well as impaired long-term survival of individuals with AF compared to those with normal sinus rhythm (SR)6. In the general population, AF is estimated to increase the risk of death 1.5-fold among men and 1.9-fold among women5. Moreover, it has been shown previously that, after surgical aortic valve replacement (SAVR), AF represents an independent predictor of late adverse cardiac and cerebrovascular events (CVE), including congestive heart failure, stroke, and mortality7,8. Similarly, NOAF is associated with overall and late mortality after coronary artery bypass graft surgery and perioperative complications, and 30-day mortality and CVE in post-myocardial infarction patients9.
In the last decade, TAVI has become the treatment of choice for inoperable or high-risk patients with severe, symptomatic AS, but the indication might be expanded in the near future. In the subset of patients with indications for TAVI, sparse and partly contrasting evidence exists regarding the impact of AF on morbidity and mortality. Some studies have indicated the absence of any significant impact of AF on prognosis10-18, whilst others have shown increased mortality among patients with AF undergoing TAVI19-30. Moreover, a recent meta-analysis did not mention AF among predictors of all-cause mortality in patients undergoing TAVI31.
Therefore, the aim of this meta-analysis was to compare the short- and long-term clinical outcomes of patients undergoing TAVI with and without pre-existing and new-onset AF.
Methods
The study was designed according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) requirements32,33. MEDLINE, Cochrane, ISI Web of Science and SCOPUS databases were searched for articles published from April 200234 (first-in-human TAVI date) until January 2015. Studies were identified using the major medical subject heading “transcatheter aortic valve implantation OR transcatheter aortic valve replacement OR TAVI OR TAVR” combined with “clinical outcome or mortality” and “atrial fibrillation”. Citations were screened at the title and abstract level by two independent reviewers and retrieved as a full report if they reported data on outcomes after TAVI, based on the presence/absence of AF and/or if AF was considered as a predictor of mortality in their regression models. No language limitations were applied. The full texts and bibliographies of all potential articles were also retrieved in detail to seek additional relevant studies.
Studies were included if: 1)TAVI was performed in high surgical risk or inoperable patients (as defined by a logistic EuroSCORE >20 or by the presence of contraindications to surgery such as porcelain aorta, severe respiratory failure, unfavourable anatomy for sternotomy) with symptomatic, severe AS (defined as an aortic valve area <1 cm2, or an indexed aortic valve area <0.6 cm2/m2); 2)they reported data of mortality outcomes according to the presence of pre-existing AF or NOAF.
Studies were excluded if any of the following criteria applied: 1)duplicate publication; 2)lack of data on pre-existing AF before TAVI or NOAF after the procedure; 3)the outcome of interest was not clearly reported or was impossible to extract or calculate from the published results.
Two reviewers independently screened articles for fulfilment of inclusion criteria. Reviewers compared selected trials and discrepancies were resolved by consensus. Baseline characteristics, AF at baseline and outcomes, including mortality outcomes, were abstracted.
The primary endpoint evaluated was the incidence of early and long-term all-cause mortality in patients with baseline or new-onset AF undergoing TAVI. Secondary endpoints of interest were the cardiovascular mortality and the incidence of CVE in the same population. Long-term follow-up included a time frame ranging from six months to five years from the procedure. Short-term follow-up corresponded to 30-day follow-up.
Of 1,424 articles identified by the initial search, 45 were retrieved for more detailed evaluation and 26 trials were included in the study (Appendix Figure 1).
The number of events, participants, hazard ratios (HR) and confidence intervals (CI) were abstracted. Pooled measures were calculated assuming a random effects model using inverse variance weighting, and used the adjusted HR. The results were also confirmed with a fixed effects model; however, the random effects model was prioritised in case of significant heterogeneity. Statistical significance was set at p≤0.05 (two-tailed). Heterogeneity was assessed by a Q-statistic and I2 test. Significant heterogeneity was considered present for p-values <0.10 or an I2 >50%.
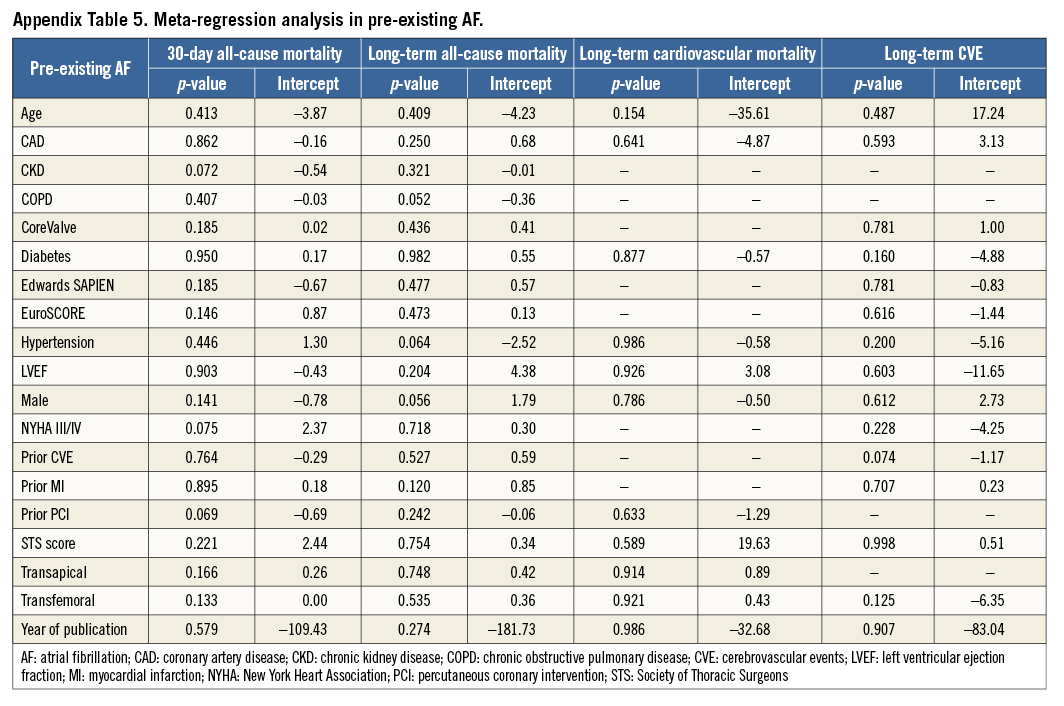
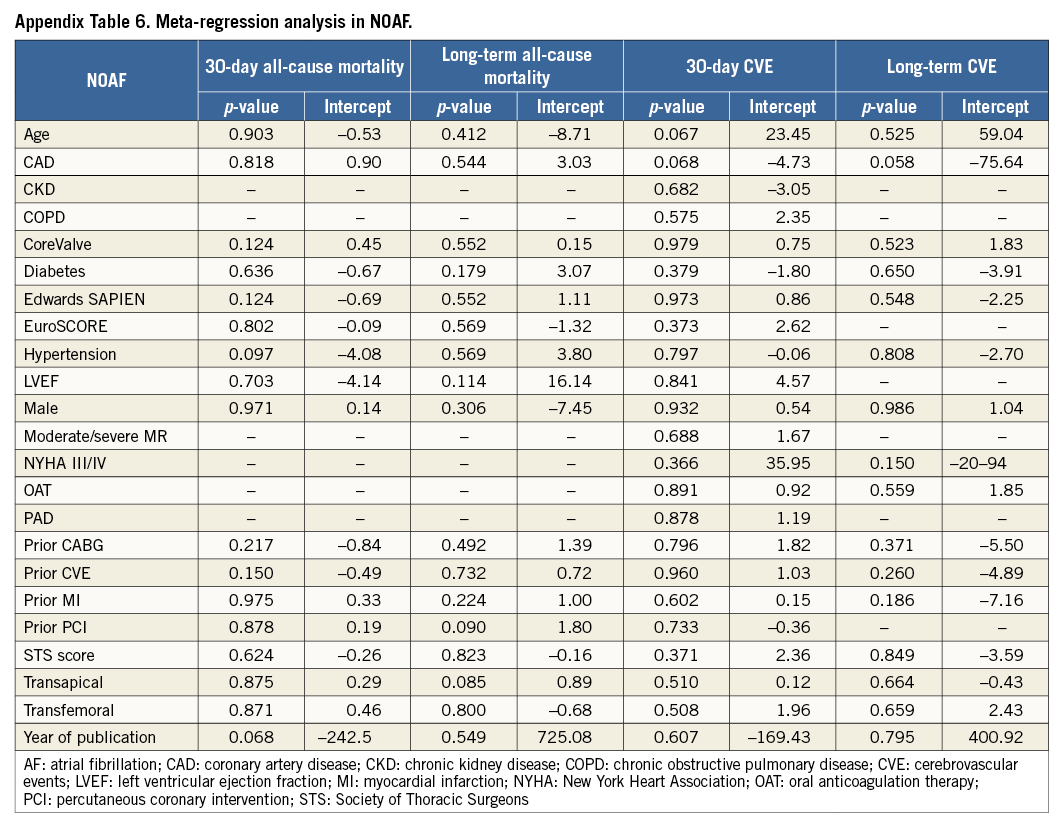
Meta-regressions were performed to test the influence of baseline characteristics included in Table 1 as potential effect modifiers (significance at p≤0.05).
Publication bias was assessed using funnel plots and Egger’s test, consisting of a linear regression of the intervention effect estimates on their standard errors, weighting by 1/(variance of the intervention effect estimate)35. If there was some evidence of publication bias, the trim and fill method, which estimates the number and results of potential missing studies resulting from publication bias, was applied36.
All data analyses were performed using Prometa Software, Version 2 (Internovi, Cesena, Italy), and Review Manager (RevMan), Version 5.2 (The Cochrane Collaboration, London, United Kingdom)37-41.
Results
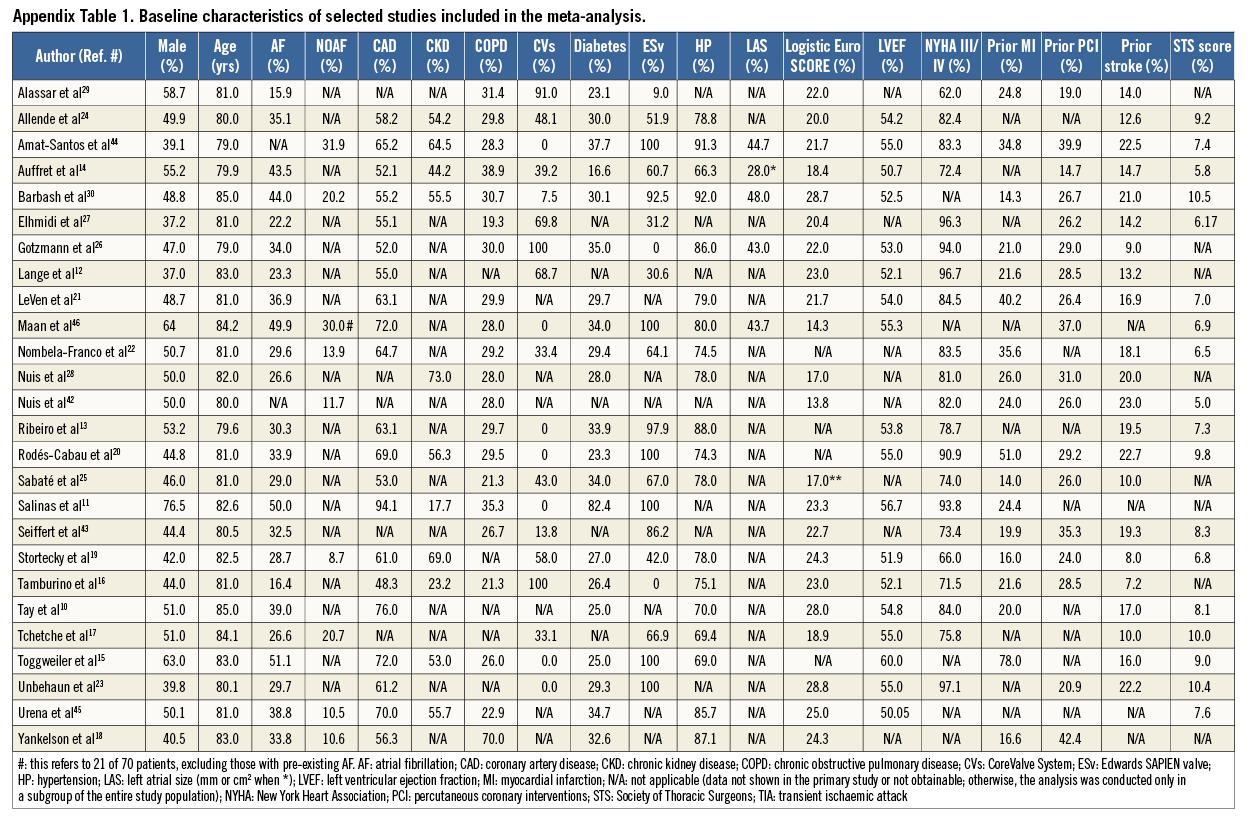
Of the 1,424 articles identified in the initial search, 45 were retrieved for more detailed evaluation. Nineteen studies were subsequently excluded. Therefore, 26 studies, enrolling 14,078 patients, were finally included in the analyses (Table 1, Appendix Table 1, Appendix Figure 1)10-30,42-46.
Pre-existing AF is common among patients with symptomatic severe aortic stenosis undergoing TAVI, with an average prevalence of 33.4±9.6% in our meta-population (23 studies; 13,241 patients; 3,824 pre-existing AF). NOAF incidence after TAVI was, on the other hand, 17.5±8.7% (nine studies; 4,749 patients; 831 NOAF).
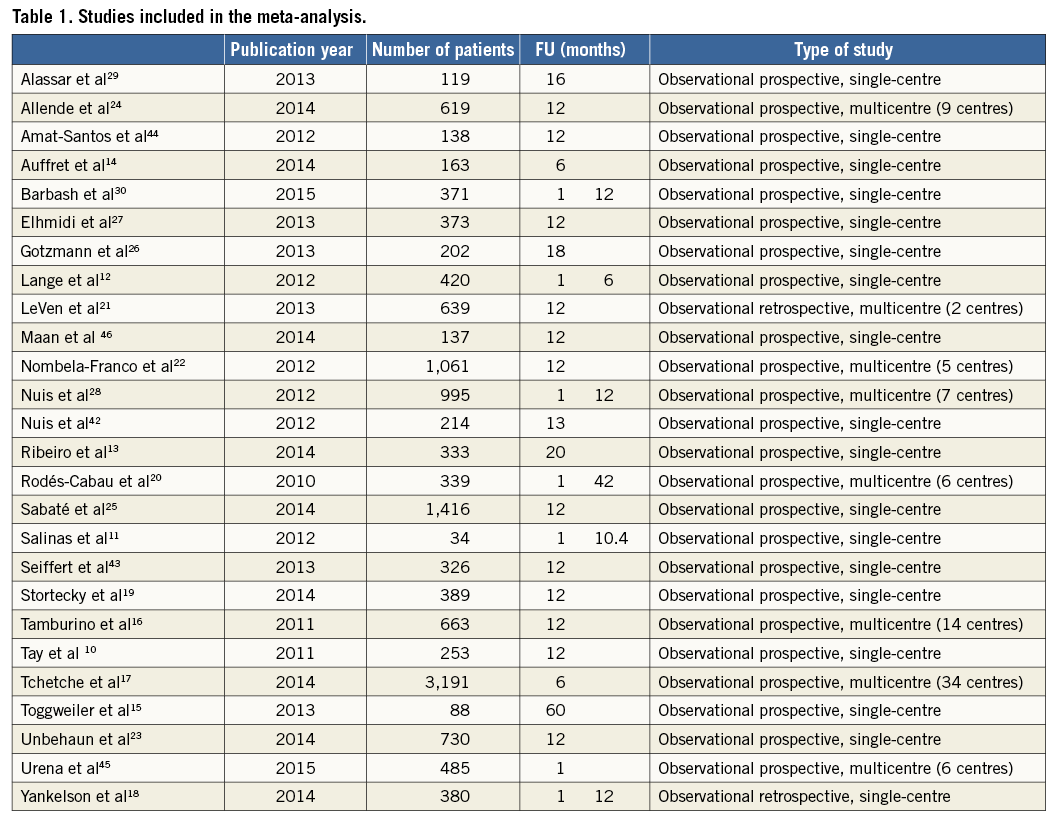
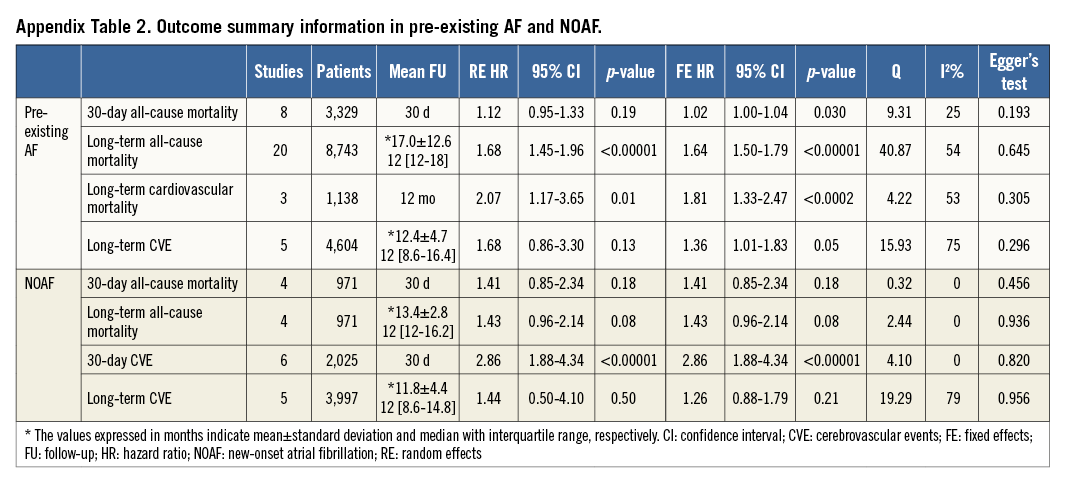
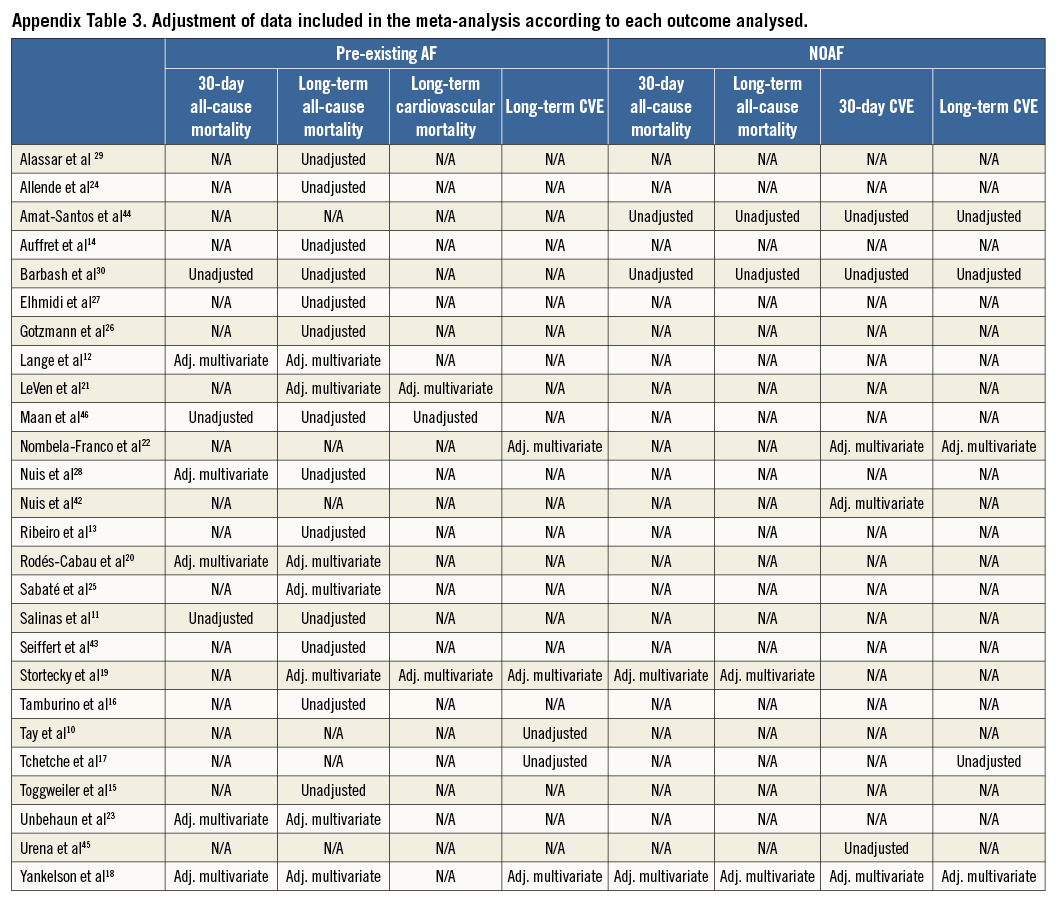
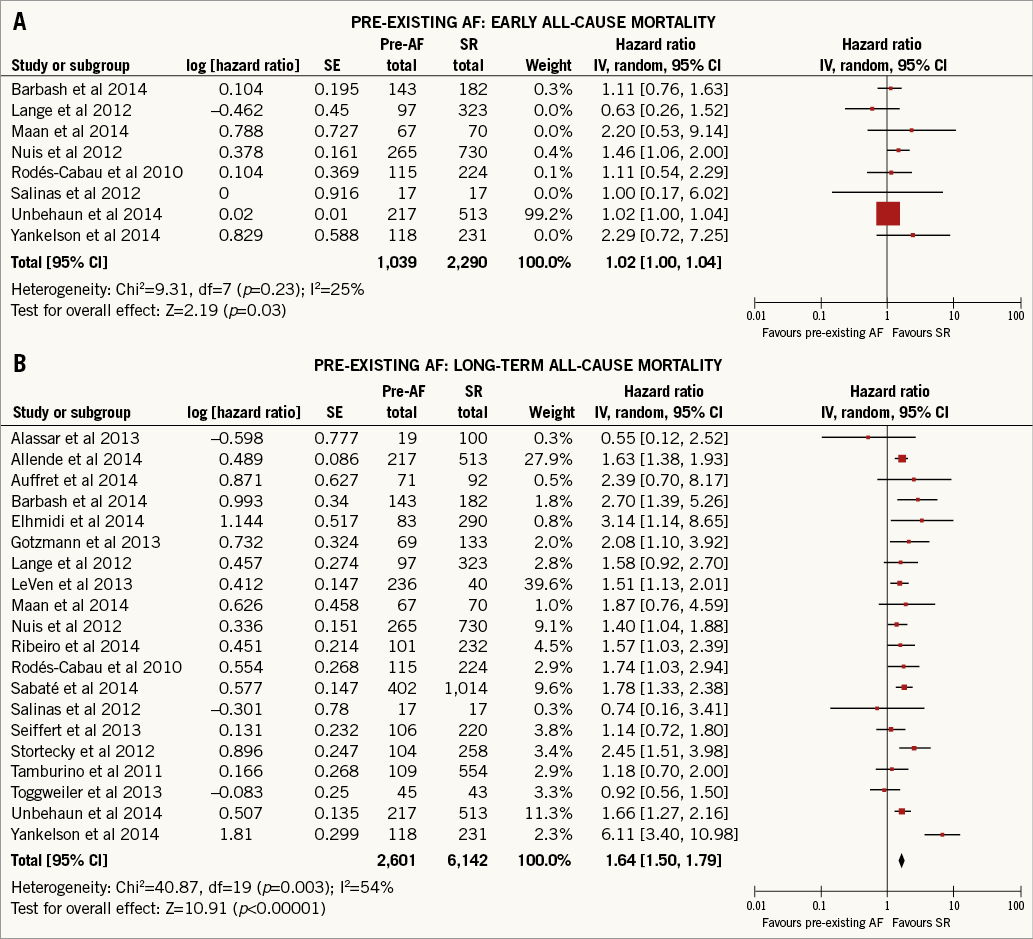
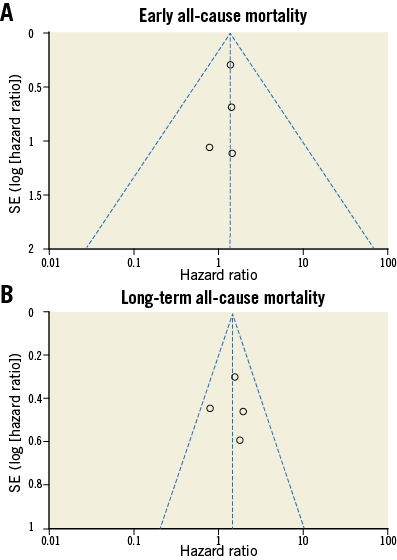
In patients with pre-existing AF, the overall mortality risk post TAVI was not significantly increased at 30-day follow-up (eight studies, 3,329 patients, HR: 1.12, 95% confidence interval [CI]: 0.95 to 1.33; p=0.19, I2=25%) (Figure 1A, Appendix Table 2, Appendix Table 3). Conversely, it was significantly increased at long-term follow-up (20 studies, 8,743 patients, HR: 1.68, 95% CI: 1.45 to 1.96; p<0.00001, I2=54%) (Figure 1B, Appendix Table 2, Appendix Table 3).
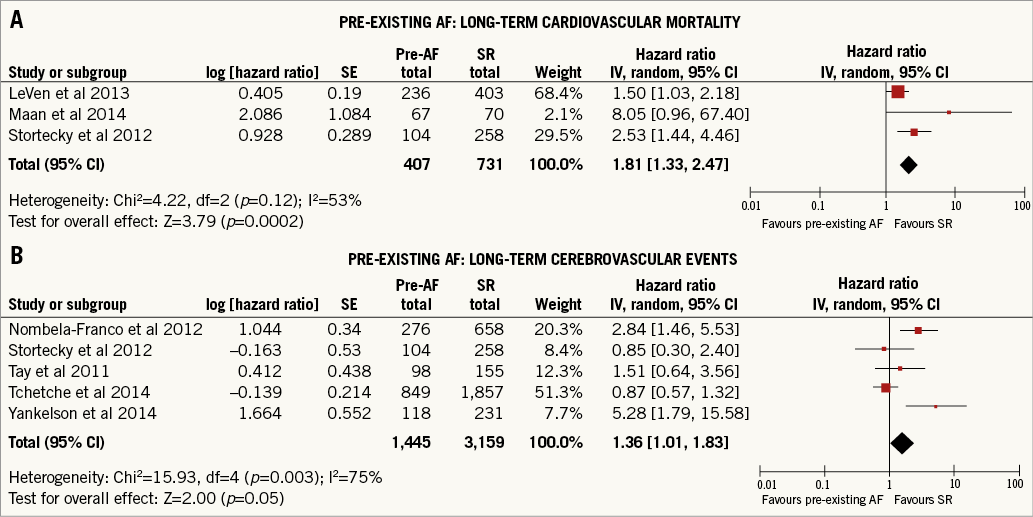
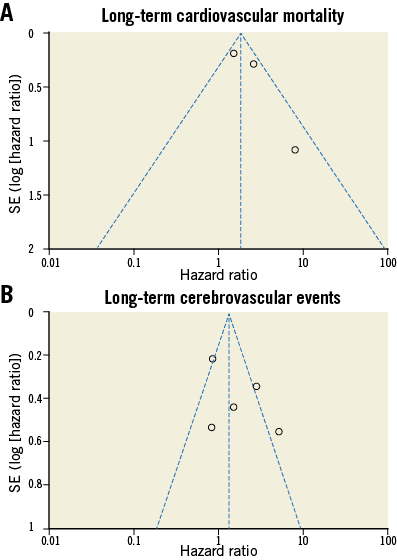
Cardiovascular mortality at long-term follow-up was significantly increased in patients with pre-existing AF when compared to patients with baseline SR (three studies, 1,138 patients, HR: 2.07, 95% CI: 1.17 to 3.65; p=0.01, I2=53%) (Figure 2A, Appendix Table 2, Appendix Table 3).
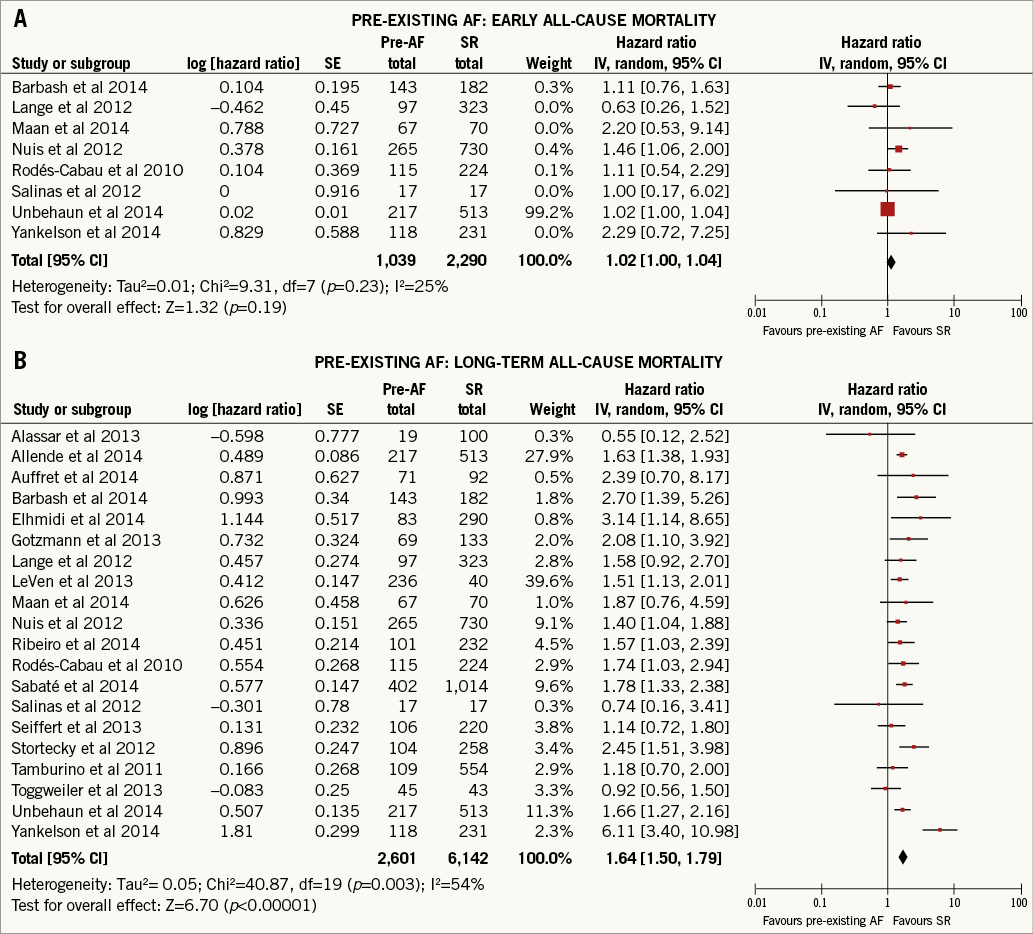
Figure 1. Impact of pre-existing AF on early and long-term all-cause mortality. Random effects hazard ratio and 95% confidence interval for early (A) and long-term (B) all-cause mortality.
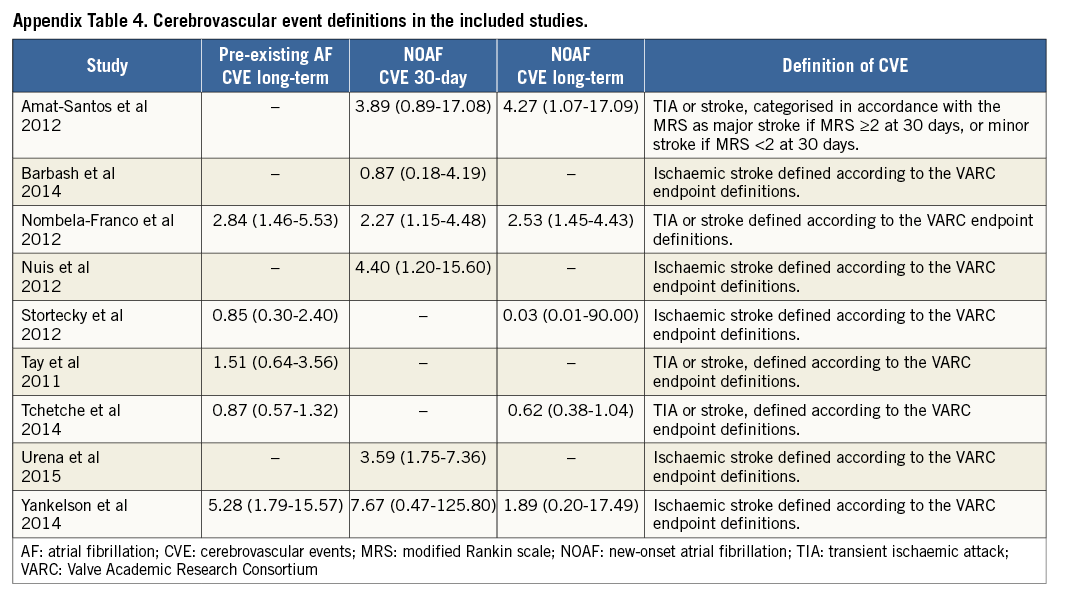
Additionally, the presence of pre-existing AF in patients undergoing TAVI did not predict CVE at long-term follow-up (five studies, 4,604 patients, HR: 1.68, 95% CI: 0.86 to 3.30; p=0.13, I2=75%) (Figure 2B, Appendix Table 2-Appendix Table 4). All these results were confirmed with fixed effect models (Appendix Figure 2 and Appendix Figure 3).
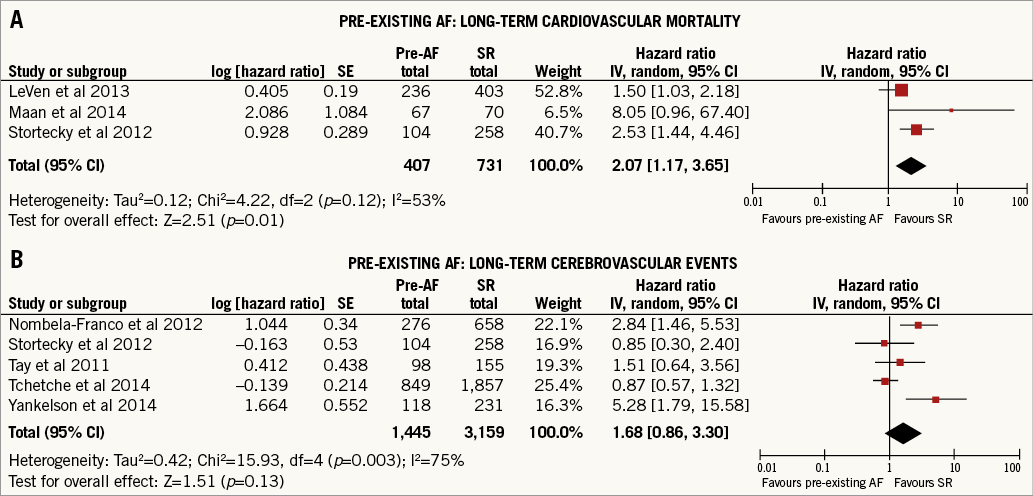
Figure 2. Impact of pre-existing AF on long-term cardiovascular mortality and cerebrovascular events. Random effects hazard ratio and 95% confidence interval for long-term cardiovascular mortality (A) and long-term cerebrovascular events (B).
Patients with and without NOAF did not show significant differences of 30-day (four studies, 971 patients, HR: 1.41, 95% CI: 0.85 to 2.34; p=0.18, I2=0%) (Figure 3A, Appendix Table 2, Appendix Table 3) or long-term all-cause mortality (four studies, 971 patients, HR: 1.43, 95% CI: 0.96 to 2.14; p=0.08, I2=0%) (Figure 3B, Appendix Table 2, Appendix Table 3).
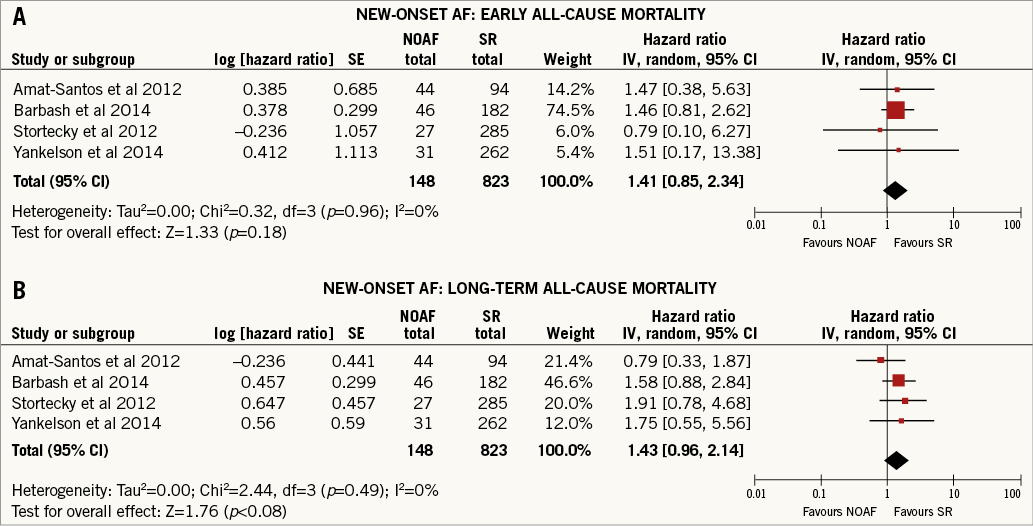
Figure 3. Impact of NOAF on early and long-term all-cause mortality. Figure showing random effects hazard ratio and 95% confidence interval for early (A) and long-term (B) all-cause mortality. Note: fixed effects estimates for early (four studies, 971 patients, HR: 1.41, 95% CI: 0.85 to 2.34; p=0.18, I2=0%) and long-term all-cause mortality (four studies, 971 patients, HR: 1.43, 95% CI: 0.96 to 2.14; p=0.08, I2=0%).
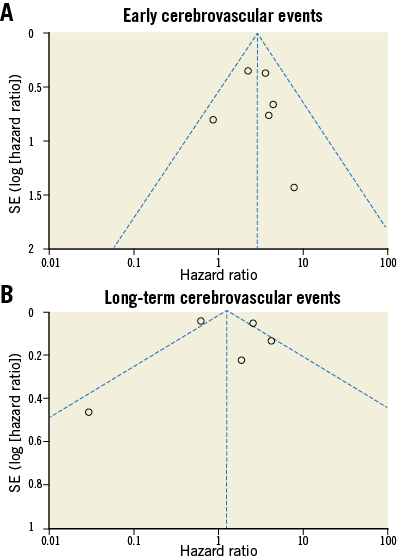
On the other hand, NOAF proved to be a significant predictor of CVE at short-term follow-up (six studies, 2,025 patients, HR: 2.86, 95% CI: 1.88 to 4.34; p<0.00001, I2=0%) (Figure 4A, Appendix Table 2-Appendix Table 4), while there was a non-significant increase in the incidence of CVE at long-term follow-up (five studies, 3,997 patients, HR: 1.44, 95% CI: 0.50 to 4.10; p=0.50, I2=79%) (Figure 4B, Appendix Table 2-Appendix Table 4).
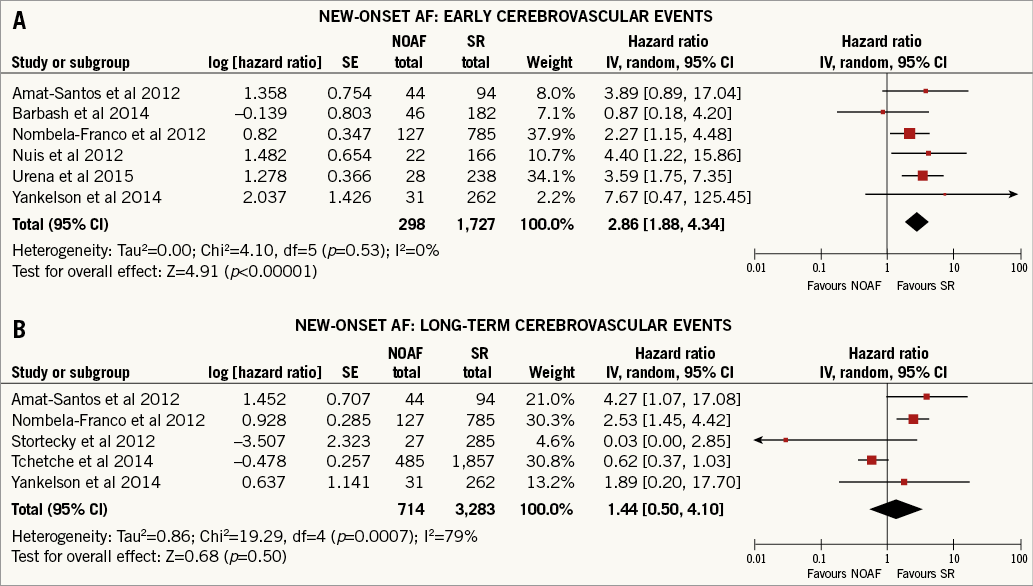
Figure 4. Impact of NOAF on early and long-term cerebrovascular events. Figure showing random effects hazard ratio and 95% confidence interval for early (A) and long-term cerebrovascular events (B). Note: fixed effects estimates for early (six studies, 2,025 patients, HR: 2.86, 95% CI: 1.88 to 4.34, p<0.00001, I2=0%) and long-term cerebrovascular events (five studies; 971 patients, HR: 0.26, 95% CI: 0.88 to 1.79; p=0.21, I2=79%).
Meta-regression analysis showed no relationship between all the analysed effect modifiers and the outcomes of interest (all p-values >0.05) (Appendix Table 5, Appendix Table 6).
The funnel plots (Appendix Figure 4-Appendix Figure 7), Egger’s test (Appendix Table 2) and the trim and fill method did not show any publication bias, in all the analyses performed.
Discussion
The present meta-analysis demonstrated that AF is common among high-risk elderly patients undergoing TAVI, with a prevalence of 33.4% in this patient population, and that AF is associated with a significantly increased risk of all-cause mortality at long-term follow-up. However, the presence of AF at baseline does not seem to represent a risk factor for 30-day all-cause mortality or for CVE in the long term following TAVI. On the other hand, NOAF occurred in 17.5% of patients after TAVI and was not associated with increased mortality, but with an increased risk of CVE.
AF is the most common cardiac arrhythmia, and is associated with structural heart disease, in particular hypertensive heart disease, coronary artery disease and valvular heart disease. Due to the high prevalence of AF in the elderly population and to the similarity of risk factors for both AF and severe degenerative AS, both conditions coexist in almost 50% of patients. Similar to the general population, in whom AF is estimated to carry a 1.5-fold increased risk of death among men and 1.9-fold among women5, our meta-regression analysis confirms these data also for patients undergoing TAVI, with a higher HR for all-cause mortality.
The observed differences in outcome among patients in SR and patients with baseline AF are not surprising and may be attributable to a worsening in heart failure from decreased ventricular filling secondary to loss of atrial systolic contraction, tachycardia-induced cardiomyopathy and/or complications associated with systemic embolisation, all conditions also contributing to all-cause mortality37,47. Indeed, heart failure might be precipitated in hypertrophied left ventricles with a lower ejection fraction because of the sudden loss of the Frank-Starling mechanism in cardiac reserve compensating in part for the reduced left ventricle contractility. This is particularly relevant in pressure-overload left ventricular hypertrophy, when geometry is often concentric and myocardial mechanics are substantially depressed due to structural modifications. As far as NOAF is concerned, although inflammatory components have been shown to be responsible for its occurrence after cardiac surgery48, the mechanisms leading to the arrhythmia after TAVI have still to be clarified. No hypothetical differences between different types of valve or procedure have emerged up to now. Indeed, the results of our meta-regression analysis did not evidence any significant difference between the CoreValve® (Medtronic, Minneapolis, MN, USA) and the Edwards SAPIEN (Edwards Lifesciences, Irvine, CA, USA) valve, or between transfemoral and transapical implantation in terms of the incidence of NOAF.
The results of this meta-analysis demonstrate that pre-existing AF is a predictor of all-cause mortality in the long term following TAVI. This provides clarification to the current literature, since, even in recent publications, AF was not identified as a predictor of all-cause mortality31.
It is important to underline that patients undergoing TAVI exhibit an incidence of stroke which is not negligible49: this is principally due to manipulation of large catheters in atherosclerotic and calcified aortas and to embolisation after valvuloplasty or valve implantation. On the other hand, AF itself represents a risk factor for stroke. Interestingly, the result of this meta-analysis, although coming from a pooled analysis of only five studies with a limited number of patients (4,604), clarifies that patients with pre-existing AF did not experience a higher incidence of new CVE when compared to patients in SR. These data, probably corroborating what has been previously shown, might support the concept that the main causes of stroke following TAVI are technical. However, in the subset analysed in this meta-analysis, we were not able to reach a statistical significance on this outcome. This might be due to a variety of issues. First, the total number of CVE is generally low and the number of studies/patients for this analysis is relatively low to draw consistent and final conclusions. Second, it has to be taken into account that, both in patients with pre-existing AF and in those with NOAF, drug therapy was administered. Unfortunately, we were not able to consider the effects of drugs on CVE because often these data were not reported in the primary studies. Conversely, the occurrence of NOAF seemed to be linked to a higher incidence of CVE, particularly at short-term follow-up.
However, while pre-existing AF analysis demonstrating increased mortality was obtained in up to 8,000 patients, the results in NOAF were observed in fewer than 1,000 patients. Therefore, we cannot exclude an impact of NOAF on mortality, and future studies in larger populations of NOAF are needed.
Certainly, these results might have been induced by the different therapeutic strategies adopted in AF patients when compared to patients in SR. Unfortunately, the absence of the use of a standardised therapy in the available trials made it impossible to analyse, in this meta-analysis, the effect of different antithrombotic regimens on outcome after TAVI, in particular in AF patients. Therefore, future randomised studies are needed to determine the most appropriate antithrombotic therapy in arrhythmic TAVI patients. In addition, this meta-analysis is limited by the inclusion of observational studies not directly comparing AF and non-AF patients, except in one case. The limitations of this study are mainly related to differences in the studies included, as is the case for all meta-analyses. All the studies were observational and the data reported were not sufficient to analyse the role of AF subtypes or AF clinical management. Due to incomplete/unequal reporting of data, not all studies were analysed for all outcomes.
Long-term CVE for both pre-existing AF and NOAF showed a high heterogeneity (>70%) not explained by analysis of potential modifiers or publication bias. Therefore, the results should be considered with caution. However, this heterogeneity reflects the contrasting results among the studies included on this issue, supporting the need for a meta-analysis and future larger studies.
Finally, among the studies included there were no overlapping populations (duplicates were excluded in the eligibility screening). However, given that many studies are multicentre, a small number of overlapping patients cannot be excluded.
Conclusions
In conclusion, pre-existing AF, but not NOAF, is a predictor of long-term mortality. NOAF, on the contrary, predicts new CVE in the short term after TAVI. Screening patients’ rhythm may help to identify a subgroup at higher risk of future major events, while preventing NOAF may help to reduce CVE in patients undergoing TAVI. Thus, similar to the results with SAVR, AF should be taken into account when referring a patient for a TAVI procedure.
| Impact on daily practice Despite the clinical safety of TAVI, mortality and cerebral events still occur. New prognostic predictors could be useful for future risk scores and for decision making in daily practice for patients with moderate-to-severe aortic stenosis. These findings should be taken into account not only when selecting patients for TAVI, but also after treatment in order to reach an appropriate diagnosis, to decide on clinical management and to reduce clinical events, optimising prognosis after TAVI. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
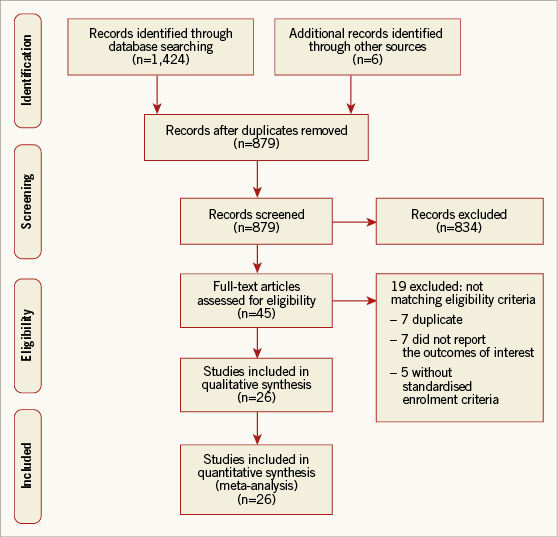
Appendix Figure 1. Meta-analysis flow chart.
Appendix Figure 2. Early and long-term all-cause mortality in pre-existing AF. Fixed effects model.
Appendix Figure 3. Long-term cardiovascular mortality and cerebrovascular events in pre-existing AF. Fixed effects model.
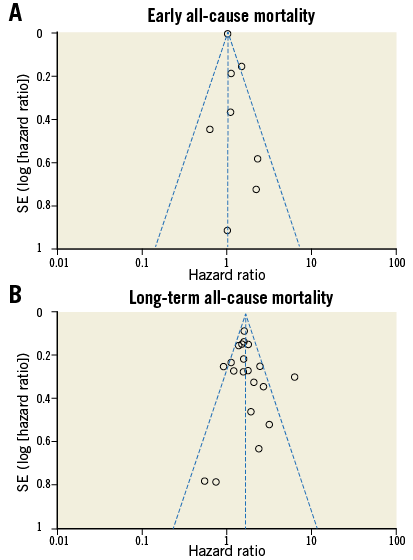
Appendix Figure 4. Pre-existing AF: funnel plots of outcome.
Appendix Figure 5. Pre-existing AF: funnel plots of outcome.
Appendix Figure 6. New-onset AF: funnel plots of outcome.
Appendix Figure 7. New-onset AF: funnel plots of outcome.