- meta-analysis
- systematic review
- atrial septal defect
- treatment
- surgery
- transcatheter
Abstract
Aims: To summarise data from studies comparing surgical (SC) versus percutaneous closure (PC) of atrial septal defects (ASDs).
Methods and results: Electronic databases, journals and major international conference proceedings were systematically searched for pertinent clinical studies comparing the two methods of closure (percutaneous and surgical) published up to December 2008, including only those reporting on more than 20 patients. Primary endpoints: occurrence of death and of total and major early complications. Thirteen original studies (3,082 patients) were included. All studies were non-randomised. One death was reported in the surgical group (0.08%; 95% C.I. 0-0.23%). Analysis of postprocedural complications showed a 31% rate (95% CI 21-41%) in SC patients and a 6.6% rate (95% CI 3.9-9.2%) in PC subjects. The adjusted OR for SC vs. PC total complications was 5.4 (95% CI 2.96-9.84; p<0.0001), significantly in favour of PC. The postprocedural major complication rate was 6.8% (95% CI 4-9.5%) in SC patients and 1.9% (95% CI 0.9-2.9%) in PC patients. The adjusted OR for SC vs. PC major complications was 3.81 (95% CI 2.7-5.36; p=0.006), again favouring PC.
Conclusions: The largest cohort to date of patients with secundum ASD shows that treatment by a percutaneous approach has a significantly lower rate of either total or major early postprocedural complications compared to surgery.
Introduction
The secundum atrial septal defect (ASD) is one of the most common congenital heart malformations, accounting for 10 % of all congenital heart defects1. Surgical closure was performed for the first time in 19532 and has been considered the standard treatment for patients with a secundum ASD. Surgery provides known good early post-operative and long-term results3-7. However, percutaneous options have become available over the last 10 years8. In the literature there are some observational studies in which the results of these two techniques have been compared9-21. However, comparison in a very large data set is lacking. To overcome this issue, and to provide an evidence-based evaluation of the comparison between these two techniques, we performed a comprehensive meta-analysis of all currently available studies comparing surgical and transcatheter approaches.
Methods
Data sources and searches
Relevant articles published between January 1998 and December 2008 were systematically searched in BioMedCentral (http://www.biomedcentral.com), Google Scholar (http://www.scholar.google.com) and PubMed (http://www.pubmed.gov). Previous qualitative and systematic reviews, if available, were checked for additional studies. The following query terms were used: atrial septal defect, closure, surgery, percutaneous, transcatheter. Further studies were sought by means of a manual search of secondary sources, including references from primary articles (backward snowballing), contacts with international experts and major international conference proceedings. No language restrictions were enforced.
Study selection
Citations were first screened at the title/abstract level by two independent reviewers (G.B., G. B.-Z.), and retrieved as complete manuscripts if potentially pertinent. Disagreements were resolved after consensus. Identified articles were independently appraised according to the following inclusion criteria by the same reviewers (all criteria requiring fulfilment for study inclusion, dispute again resolved by consensus): a) cohort studies, either prospective or retrospective, comparing the clinical results of b) percutaneous vs. surgical closure of secundum ASD associated with right ventricular overload which c) enrolled a minimum of 10 patients in each treatment arm. Studies in which authors closed PFOs or ASDs with no preprocedural haemodynamic sequala were excluded.
When more than one article originating from the same centre met the selection criteria, the study reporting on the most patients was reported and those with the least were excluded to avoid duplication. The main exclusion criterion was publication only as an abstract or unpublished data as no detailed data on patient selection and multivariable adjustment could be obtained. We also excluded papers comparing physiological or instrumental data between patients treated with the two techniques.
Data extraction, outcomes and quality assessment
The following data was recorded by two independent reviewers (M.C., A.F.) on pre-specified forms, with disagreement resolved after consensus: author, journal, study interval and publication year, study design, sample size, patients’ characteristics, gender, age, method of imaging used to diagnose the septal defect, type of device used for percutaneous septal defect closure, procedural data (procedure time, fluoroscopy time, bypass time, aortic cross clamp time), total complication rate, major and minor complication rate, details about complications, hospital stay, residual shunting, success rates, costs, and follow-up.
Primary endpoints
The primary endpoints studied were: death and total major and minor complication rate. When authors simply described the occurrence and type of complication, two independent authors –one surgeon and one interventional cardiologist (M.C, A.F.)– blinded for the treatment group, classified the complication as major or minor according to previously published classifications5,9,15,22,23. Controversies were resolved by consensus agreement.
Complications were classified as: (1) minor, (2) major, and (3) death, on an intention-to-treat basis.
1)Minor complications:
We defined a complication as minor if it could be completely treated by drugs and caused no haemodynamic abnormality. Such complications included transient arrhythmias or drug terminated arrhythmias, mild pericardial effusion, mild pneumothorax, anaemia not requiring transfusion, upper respiratory tract infections, fever, groin haematoma, and others.
2)Major complications:
We defined a complication as major if it caused haemodynamic instability and/or needed immediate invasive/surgical treatment. In the group treated with surgery these complications were heart failure, pericardial or pleural effusion requiring surgical drainage, pneumothorax needing surgical drainage, cardiac tamponade, arrhythmias needing immediate external cardioversion, thrombus formation on the atriotomy treated by heparin, redo operation, and severe anaemia needing blood transfusion.
Major complications in the percutaneously treated group were device embolisation/malposition needing surgical retrieval and surgical closure of the defect, vascular injury of the femoral vessels requiring surgical repair, pericardial effusion with or without cardiac tamponade due to wall perforation by the device, in addition to the complications described for the surgically treated group.
3)Death
Secondary outcomes studied were: length of hospital stay and feasibility of percutaneous closure.
The quality of included studies was appraised according to established methods24,25, by two independent reviewers aware of the study origin and journal, with divergences resolved after consensus. In particular, we separately estimated the risk of selection, performance, detection and attrition bias judged as low risk of bias (A), moderate risk of bias (B), high risk of bias (C), or incomplete reporting leading to inability to ascertain the underlying risk of bias (D). Other major avenues of appraisal were the following: a)whether the sample of patients was representative; b)whether the patients were sufficiently homogeneous with respect to prognostic factors; c)whether follow-up was sufficiently complete; d)whether objective and unbiased outcome criteria were used; and, e)the likelihood of outcome occurrence over time.
Data synthesis and statistical analysis
Categorical variables are reported as n (%) and quantitative variables as median (1st quartile-3rd quartile range). A DerSimonian-Laird method was used for dichotomous variables, whereas ageneric inverse variance weighting was used for pooling of individual point estimate values (with pertinent standard errors). The Cochrane Collaboration RevMan 4.0 freeware package (http://www.cochrane.org) was used for analysis. Meta-regression was performed with STATA 9.1 (StataCorp, College Station, TX, USA) to explore the impact of age, ASD, difference in age between groups, and year of publication on the dependent variables (total complication, major complication, length of hospital stay), considered as study outcomes.
Specifically, a linear regression was carried out with empirical Bayesian estimation, selecting the natural logarithm of the response rate as the dependent variable, the prevalence of the moderator of interest as the independent variable, and the standard error of the dependent variable as weighting. Small study bias was appraised by means of funnel plot inspection and Egger test. Statistical heterogeneity was tested by means of forest plot inspection, computation of the Q statistic, comparison with a χ² distribution, and calculation of corresponding p values. Statistical inconsistency was appraised with I2. Two-tailed p values and 95% C.I. are reported throughout, with a 0.05 threshold for hypothesis testing of effect and a 0.10 threshold for statistical homogeneity.
Results
Study identification
Database searches initially retrieved 4,342 citations, from which 4,297 hits were excluded at the title or abstract level. After thorough assessment, according to the selection criteria, we further excluded 32 citations, finally including 13 studies in the analysis (3,082 patients: 1,270 treated surgically and 1,812 treated by using a percutaneous approach)9-21.
Characteristics of included studies
All studies were non-randomised and observational. Many of the papers included were retrospective, with data coming from a single centre (Table 1). Only the papers by Du15 and Jones21 were multicentre studies, while prospective studies were carried out by Thomson12, Hughes10, Du15 and Jones21. Most patients were treated percutaneously using an Amplatzer ASD occluder (Table 2).
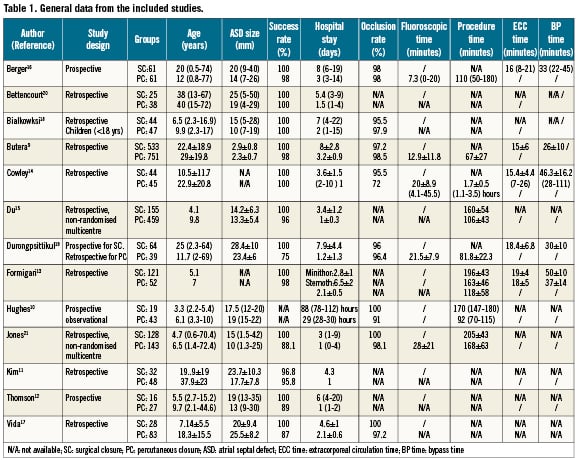
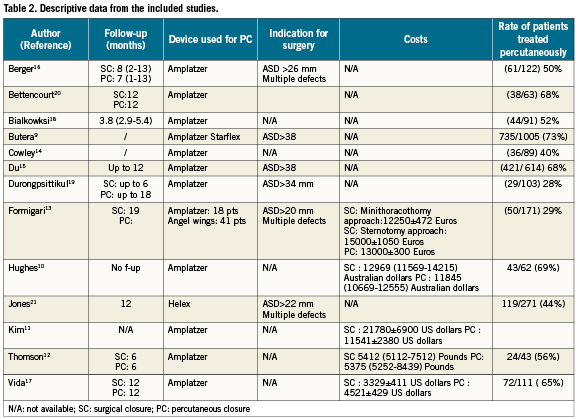
Exclusion criteria for percutaneous closure according to ASD size varied in studies reported and over publication time (Table 2). In fact, in early reports (between 1999 and 2001) using the Amplatzer occluder, authors closed only single defects with a diameter up to 20-26 mm13,16, while afterwards single defects up to 34-38 mm and multiple holes were closed percutaneously. Patients treated using the Helex device were treated when the defect was a single one, with a diameter up to 22 mm21. In all papers good rims (more than 5-7mm) were mandatory to close the defects percutaneously. The only exception was the absence of the aortic rim which did not prevent percutaneous closure in many studies.
In almost all papers percutaneous closure was performed under general anaesthesia with TEE control. Berger16 and Bettencourt20 performed procedure under conscious sedation and TEE control. Jones et al21 reported the use of ICE to control for device implantation. Surgical closure was undertaken according to accepted standard surgical protocols by using either patch or direct closure. Midline sternotomy was performed in all papers except one by Formigari et al13 in which a group having minimally invasive sternotomy was described. After percutaneous closure, all studies treated patients with antiplatelet therapy for 3-6 months.
Quantitative synthesis of primary outcomes
All studies provided enough details for the primary endpoints (mortality, total complication rate, major complication rate and length of hospital stay). Mortality occurred in only one subject treated surgically21 in whom cardiac tamponade occurred six days after surgery (0.08%; C.I. 95% 0-0.23%). Quantitative synthesis of total postprocedural complications showed a 31% (95% CI 21-41%) rate in patients treated surgically and a 6.6% (95% CI 3.9-9.2%) rate in subjects treated percutaneously. Comparison of percutaneous closure versus surgery showed an adjusted odds ratio for total complications of 5.4 (95% CI 2.96-9.84; p<0.001 for effect; χ²=59.8; degrees of freedom=12; p<0.001 for heterogeneity; I2=80%), demonstrating a significantly higher risk for surgical closure (Figure 1). Quantitative synthesis for major postprocedural complications gave a rate in surgical patients of 6.8% (95% CI 4-9.5%) compared to a 1.9% rate (95% CI 0.9-2.9%) after percutaneous closure. Comparison of percutaneous closure versus surgery showed an adjusted odds ratio for major complications of 3.8 (95% CI 2.7-5.36; p=0.006 for effect; χ²=11.7; degrees of freedom=12; p=0.47 for heterogeneity; I2=0%), showing a higher risk for surgical patients (Figure2).
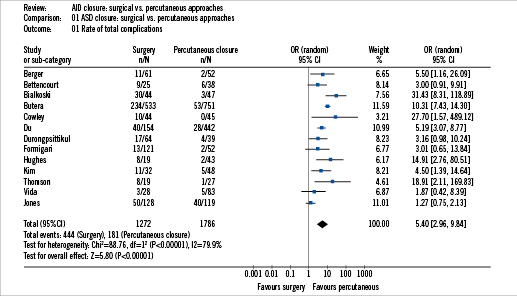
Figure 1. Total complications.
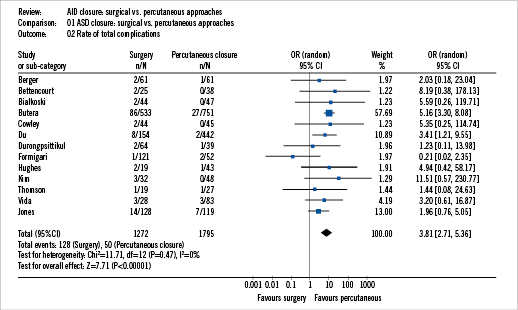
Figure 2. Major complications.
Details on major complications
Surgical group
Redo surgery occurred in nine subjects (five patch dehiscence and four major bleeding) (Table 3). A surgical drainage tube was needed in 34 subjects (seven pneumothorax, nine pleural effusion and 16 pericardial effusions). Wound infection occurred in five patients. Haemodynamically significant arrhythmias needing urgent electrical or pharmacological treatment was reported in 38 patients (one ventricular tachycardia, 34 atrial flutter or fibrillation, three complete AV block). Blood transfusion was performed in 94 subjects. Athrombus was seen on the atriotomy in eight patients. Other major complications occurred in 12 subjects (endocarditis=1; seizures=1; ischaemic stroke=1; duodenal perforation=1; Horner syndrome=1; cardiac arrest=1; need for inotropic support=6). Severe sequelae were seen in three subjects (one with severe heart failure and two with neurologic sequelae). Finally death occurred in one subject21.
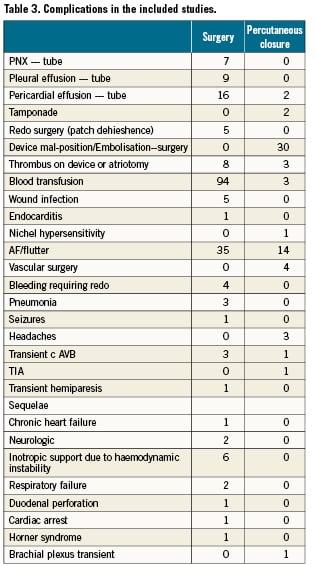
Transcatheter group
The most frequent major complications in the transcatheter group were embolisation or malposition needing surgery or further transcatheter approach in 30 subjects. Perforation of the heart due to the device erosion was reported in three subjects (one treated with the angel wing device and two treated with Amplatzer devices). Significant pericardial effusion needing surgical drainage was needed in two subjects. Four patients underwent vascular surgery due to a femoral venous or arterial lesion. Thrombus formation on the device was seen in three subjects and was treated medically. Atrial flutter or fibrillation needing electrical or pharmacological treatment was reported in 10 patients. Other complications occurred in six subjects (transient ischaemic attack=1; transient complete AV block=1; transient brachial plexus injury=1; and blood transfusion=3).
Additional analysis
We pooled data to obtain an estimate of age difference and ASD size between the patients treated percutaneously and those treated surgically. Patients treated surgically were younger (–3.9years [95% C.I. –7.5 to –0.36 years]; p=0.03; χ²=60.2; degrees of freedom=12; p<0.001 for heterogeneity; I2=80%) and had larger defects (+3.6mm [95% C.I. 1.6 to 5.6mm; p=0.001; χ²=86.5; degrees of freedom=10; p<0.001 for heterogeneity; I2=88%). Meta-regression showed a significant relationship between rate of major complications and age difference between the two treatment groups (beta –0.247; p=0.021) (Figure 3). This analysis showed that percutaneous therapy had a lower rate of major complications both when patients were younger and when they were older. Patients’ age did not thus account for the occurrence of major complications.
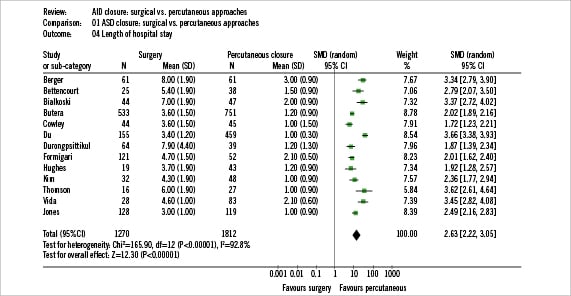
Figure 3. Meta-regression between rate of major complications and difference in age between the two treatment groups.
Pooling the available data showed that surgical patients had significantly longer hospital stays compared to device patients (2.6days [95% C.I. 2.2 to 3.1 days]; p<0.001 for effect; χ²=165.9; degrees of freedom=12; p<0.001 for heterogeneity; I2=93%) (Figure 4).
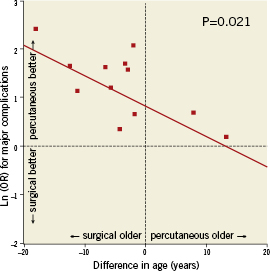
Figure 4. Length of hospital stay.
The possibility of closing a secundum ASD percutaneously during the period of study was 53.6% (95% C.I. 44.2-63.1%; χ²=256.5; degrees of freedom=11; p<0.001 for heterogeneity; I2=96%). When we selected only papers in which an Amplatzer device was used, the possibility of performing successfully a transcatheter closure was 57.2% (95% C.I. 48.3-66.1%; χ²=149.1; degrees of freedom=9; p<0.001 for heterogeneity; I2=94%) while the rate of closure utilising other devices was (36.9% [95% C.I. 22.2-51.6%]; χ²=7.7; degrees of freedom=1; p=0.006 for heterogeneity; I2=87%). Inspection of funnel plots and the Egger test for publication bias did not show evidence of small study bias (p=0.70 for total complications and p=0.15 for major complications).
Additional issues
Some authors studied the impact of closure on social life. Hughes10 reported that fathers of children undergoing surgical closure took a median of four days off work versus one day taken by fathers of those patients undergoing device closure. Thomson12 showed that patients returned to normal daily activity after a mean of two weeks for the Amplatzer group and a median of 5.5 weeks (p<0.01) for the surgical group. Hughes10 showed a significantly lower post procedure pain score and analgesia use in the percutaneous group.
Length of follow-up was different between various studies ranging between one and 18 months. However, in each study follow-ups were not different between the two types of closure. In some studies length of follow-up was not available (Table 2).
Costs were reported in few studies10-13,17. Thomson12 found no difference in costs. Kim10 and Hughes10 showed higher costs for surgical approach. Formigari13 found that the conventional sternotomy surgical approach had higher costs when compared to the minithoracotomy surgical technique and transcatheter closure.
Vida et al17 showed that, in a developing country, percutaneous closure by using an Amplatzer device has higher costs when compared to the surgical approach.
Finally, Jones21 evaluated the propensity score analysis that satisfied the non-inferiority hypothesis comparing device closure with surgery. In fact, overall clinical success was 85.5 % for surgery and 89.9% for percutaneous closure.
Discussion
Surgical ASD closure has been considered the standard treatment for more than 40 years. However, in the last 10 years, percutaneous techniques have been widely embraced8-22. There seems to be less physical and psychological impact when the percutaneous approach is utilised as opposed to surgery. Atrial septal defects were one of the first congenital heart diseases treated percutaneously by paediatric cardiologists. In fact, percutaneous closure was performed more than 30 years ago for the first time8. However, only in the last 10 years, technological improvements have led to its widespread use.
Several authors have reported traditional reviews on the treatment of ASDs26-28. Furthermore there are few studies reporting on a large number of subjects in which the two techniques have been compared. Butera et al9 reported a large single centre series and Du et al15 and Jones et al21 reported large multicentre studies where results of surgical and transcatheter approaches were compared. However, until now, neither randomised studies nor very large data sets have been published. In these cases modern statistical approaches and, in particular, the use of meta-analysis may be helpful in reaching a higher degree of scientific evidence.
A total of 3,082 patients were treated in the studies selected in our meta-analysis. One thousand two hundred and seventy (1,270) patients were treated surgically while 1,812 were treated using apercutaneous approach.
A higher rate of both total and major complications related to the surgical approach was found. In fact patients treated surgically had a 5.4-fold and 3.8-fold higher risk of total and major complications occurring respectively. By pooling data, we discovered that patients treated surgically were slightly younger (by 3.9 years) and had slightly larger ASDs (by 3.6mm). Meta regression showed no relationship between age and the occurrence of total complications however. A significant relationship was found between age and the occurrence of major complications but this relationship was clearly in favour of the percutaneous approach. Finally, length of hospital stay was 2.5 times longer in patients treated surgically.
Interestingly, our data are not in line with a study of DiBardino et al29. These authors compared data from the MAUDE (Manufacturer and User facility Device Experience) database accessed by the USFDA main web page and data from the Society of Thoracic Surgery congenital cardiac surgery database. They found that overall crude mortality for device and surgical closure of secundum ASD were equivalent while the need for rescue surgery was more common in percutaneous patients. Finally they showed that mortality for surgical management of a device complication was higher than that of elective surgical closure.
This study is very interesting but has several significant limitations and differences when compared to our meta-analysis. In fact the DiBardino et al study also included patients with patent foramen ovalis and data came from all US centres, including those with probably low levels of experience. The authors also estimated the total number of Amplatzer implants as they did not have direct knowledge of the total number of implants over the period of study, possibly leading to significant bias.
Meta-analysis studies have been reported in several fields of medicine except in the field of congenital heart disease. Our study is an attempt to address the deficiency in the currently available literature of ASD closure.
Limitations
Our study has several limitations. First of all, studies included were not randomised and were largely retrospective. However true randomisation of these two management strategies is not easily obtainable; in an era in which patients and parents of children coming from Western countries are very aware of therapeutic options, a randomised trial about ASD closure would be hard if not impossible to accept. In addition, Benson and Hartz30 found little evidence that estimates of treatment effects in observational studies (including retrospective studies) are different from those obtained in randomised controlled trials. Therefore the true superiority of randomised over well-designed observational studies has recently been questioned30,31. Probably a meta-analysis of observational studies is the best possible evidence in this field.
Secondly, other drawbacks of this paper are those typical of systematic reviews and meta-analysis32. Pooling of observational studies is considered by several investigators as hypothesis generating only32. In addition, there may be some issues of inconsistency; definition of major complications was not homogeneous throughout the studies examined. However two independent authors, blinded for the treatment group, classified the complications as major or minor according to previously published classifications5,9,15,22,23. The included studies also differed in terms of clinical settings, endpoint definition, duration of follow-up, defect diameter, patient age and case selection. Nonetheless, given such weaknesses, the results appear to be quite homogeneous and strong.
Finally, it is obvious that comparison is possible only for defects that may be approached by both techniques. In fact surgery has no limits whereas transcatheter approaches have several limitations related to defect size, position, rim anatomy and consistency. However, these limitations have been modified and reduced over the years. The results of our study may encourage the further development of devices designed to overcome these limitations for successful percutaneous secundum ASD closure.
Conclusions
The largest cohort analysis to date of patients with secundum ASDs shows that treatment by a percutaneous approach has comparable results to surgery but with a significantly lower rate of either total or major early postprocedural complications.
Conflict of interest statement
The authors have no conflicts of interest to declare.