Today, catheter interventional closure is the preferred first-line treatment for children and adults with congenital septum secundum atrial septal defects (ASD) when technically feasible. In most centres, a relatively rigid, self-centring double-disc device, comprising a nitinol mesh in combination with polyester fibres, is used123. The significant difference in these double-disc devices is the delivery mechanism. Some variations in nitinol strut thickness, coating, and assembly of the wires do not seem to be of major clinical importance. The AMPLATZER Septal Occluder (ASO; Abbott) has been used to close ASDs up to 36 mm in size for almost 30 years in many tens of thousands of patients worldwide4. ASO implantation under echocardiographic guidance is straightforward with high procedural success and a very low complication rate.
In contrast to the majority of these occluders, the Gore Cardioform ASD Occluder (GCA) (W.L. Gore & Associates) is composed of a platinum-filled nitinol wire frame covered with expanded polytetrafluoroethylene (ePTFE) and is available in 5 sizes (27, 32, 37, 44 and 48 mm). During deployment, the GCA forms a double disc with self-centring capabilities, adapting partially to the dimensions of the defect. The device is locked by a nitinol pin running through the central eyelet with a retrieval cord attached to the right-sided eyelet. The adaptative features of this relatively soft device allow each occluder to cover a range of ASD diameters5.
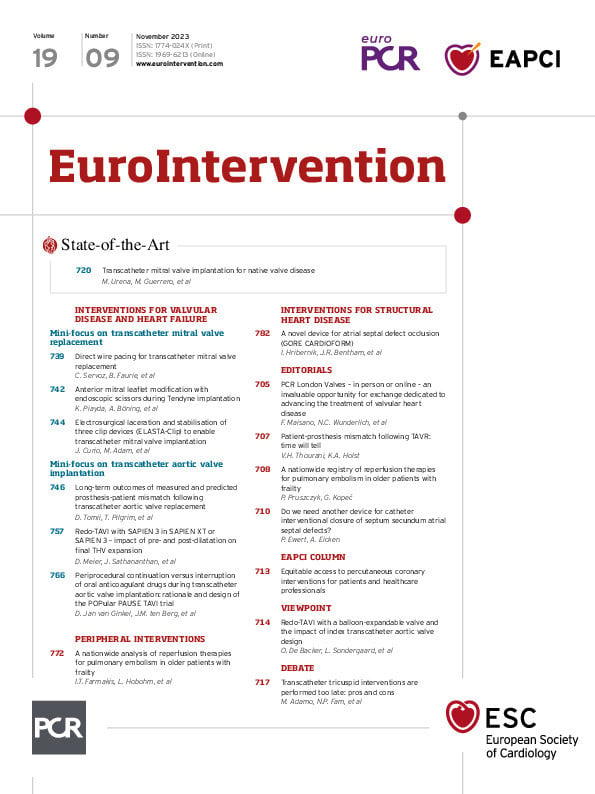
Following the ASSURED clinical study in the US, the GCA received U.S. Food and Drug Administration (FDA) approval and a CE (European conformity) mark. So far, the published experience with this occluder is scarce6. In the current issue of EuroIntervention, Hribernik and colleagues publish the results of a multicentre trial for ASD closure with the GCA device in four UK centres7 and compare their results with those of the US trial. A total of 128 ASDs (95%) were closed successfully. The median device size was 37 mm, the median age at intervention was 49 years, and 20 patients (15%) were children or adolescent, the youngest being 4 years old. The device was oversized in 63 patients (49%), 36 of these patients had deficient rims. The GCA was upsized in 13 patients, and in 4 cases, an alternative nitinol mesh device was selected.
The results of the current study mirror the results of the ASSURED trial. The rate of serious adverse events at 30-day follow-up (mainly new-onset arrhythmias) was higher than in the US trial (7.0% vs 4.8%), possibly explained by the older UK collective. Fluoroscopy to exclude wire fractures was not done in the current study. The results of this study are excellent.
Finally, do we need another ASD closure device? The answer is yes. The most feared complication after interventional ASD closure with an ASO is erosion8. Amin et al postulated a saw blade mechanism if the ASO was oversized and the stiff edges of the occluder impinge on the atrial wall behind the aortic root, most likely in the absence of an aortic rim. The true incidence of potentially fatal erosion is not known. A frequency of 1:1,000 procedures is postulated7. The current instructions for use of the ASO express a warning concerning anatomical anterior aortic rim deficiency, a finding seen in up to 40% of patients with an ASD II9. The same warning may also be expressed for all other rigid metallic double-disc ASD occluders. Not so for the GCA occluder, which is significantly softer than the other devices and for which – to the best of our knowledge – no incidence of atrial wall erosion has been reported thus far. On the other hand, potential disadvantages of this occluder are the stiff delivery system and the large sheaths necessary to implant the larger devices. These may limit its use in small children but not in adults. Further studies are needed to highlight the true incidence of arrhythmias and the impact of wire fractures, which were reported as a rate of 36% at a relatively short follow-up period in the US study. However, in the US collective, these fractures were without clinical relevance.
Conflict of interest statement
The authors have no conflicts of interest to declare.