Abstract
Although percutaneous interventions in the context of perioperative coronary artery surgery ischaemic complications are not unusual, this type of secondary revascularisation is rarely addressed in the literature. Information on aspects such as complications and clinical outcome is limited, in spite of this being a high-risk population. To shed light on the subject, the present article presents a systematic review of the literature on this topic, along with the analysis of the institutional experience at a centre with high surgical and percutaneous revascularisation case volume.
Introduction
Coronary artery bypass surgery (CABG) continues to be a key therapeutic option in treating coronary artery disease patients1. In the United States every year more than 600,000 patients are treated with CABG with a high success rate. Long-term failure of bypass conduits due to atherosclerotic involvement is frequently treated with PCI2. Specific issues like the prevention of atheroembolism with embolic protection devices, or the use of either bare metal or drug-eluting stents, have been studied in randomised trials addressing both safety and clinical benefits.
On the contrary, information on the use of PCI in the acute setting of perioperative ischaemic complications of CABG as a rescue procedure are far more limited3-13. This contrasts with the fact that perioperative ischaemic events are not uncommon and that they constitute a major threat for the patient being associated with substantial increase in morbidity and mortality, both in-hospital and in the long-term. Around 5% to 30% of patients present raised myocardial damage markers and a similar proportion of patients develop electrocardiographic changes following revascularisation procedures14. Current figures of PCI performed in this setting are unclear, since PCI registries do not include this indication as a separate one. However, there is indirect evidence that the figure has increased substantially over the last 10 years. Probably as a result of implementation of 24 hour primary angioplasty programmes in many hospitals.
To shed light on this issue, we performed a systematic review of the literature on the subject, and revisited our experience at our institution on the use of diagnostic coronary angiography and PCI as a rescue procedure for early post-CABG acute cardiac events.
Methods
Systematic review of available literature
An extensive literature search was performed using Pubmed without any date limitation and included articles in all languages. The following search terms were used: “coronary artery surgery”, “coronary artery bypass” “perioperative” and “percutaneous coronary intervention” that revealed 193 articles which were then reviewed. A second search was performed with the Cochrane data base, using the same search terms which uncovered 206 articles, out of these 11 articles were seen to address the same issue: four being case reports, while the other seven were case series.
Review of institutional experience on the subject
We conducted a review of our institutional database in order to identify patients who underwent coronary angiography/PCI within 30 days after CABG between 2004 and 2008. During this period, a total of 21,260 angiograms, 7,675 PCI and 1,220 CABG were performed, of which all procedural data was entered in a dedicated database system. Preoperative angiography reports, operative notes, post operative notes, angiographic / PCI records and discharge reports of the identified patients were reviewed. Preoperative and postoperative angiography / PCI films were assessed by two interventional cardiologists.
The following variables were assessed: findings in angiography preoperatively and postoperatively, therapeutic actions (PCI to native arteries, PCI to graft, redo-CABG) and major adverse cardiac events (MACE) during the hospital stay included death, myocardial infarction, major bleeding and further revascularisation.
Patients were followed up in an outpatient clinic and were assessed by a cardiologist or an interventional fellow who conducted phone interviews. Endpoints were also measured during follow-up, and these included death from cardiac causes, myocardial infarction, revascularisation or recurrence of angina.
Statistical analysis and data management were performed using the SPSS v14 statistical package. Categorical variables are presented as frequencies and percentages while the continuous variables are presented as mean, median and standard deviation.
Results
Literature search
Systematic review of the literature identified a total of four case reports3-6 and seven patient cohorts7-13 assessing the value and safety of emergent coronary angiography and PCI immediately post CABG. Reifart et al reported on 58 patients out of 1,263 consecutive CABG procedures that were complicated by acute myocardial infarction immediately after surgery, demonstrating the safety of coronary angiography for assessment of the underlying problem (0% severe complications), and the feasibility and benefit of PCI in these patients.7 Gobel et al studied the use of angiography in 2,635 stable patients and 311 unstable patients post CABG, demonstrating also its safety, with negligible mortality and complication rates (no deaths, 0.08% MI, 0.7% clinically important complications in the stable group versus 0.6% death and 1.3% MI in the unstable group)8. The above mentioned series also showed that in 13%-42% of the studied patients no graft complications and/or occlusion of epicardial coronary vessels in relation to pre-CABG coronary angiography could be demonstrated7,10,11,15.
Patients presenting with cardiac arrest immediately after CABG do better with early reintervention, either by redo-CABG or PCI than a non-interventional approach as was shown in a recent study by Guney et al13. This study supports the previous evidence that revascularisation is better than non-revascularisation in perioperative myocardial infarction. In the immediate, post-intervention period, there was no difference in mortality, however haemodynamic stabilisation time (p=0.012), duration of hospitalisation (p=0.00006) and mechanical support use (p=0.003) were significantly decreased by re-revascularisation. During the mean 37±25 months of follow-up period, long-term mortality (p=0.03) and event-free survival (p=0.029) rates were significantly in favour of the revascularisation group.
Very few studies directly compared conservative treatment, redo-CABG and bailout PCI in perioperative MI. Thielmann et al11 reported on 118 patients who underwent coronary angiography within the first 24 hours after CABG. The study revealed no significant differences between the three groups regarding 30 days and one year mortality (30 days FU: 12%, 20% and 14.8% respectively; one year FU: 20%, 27% and 18.5%) and this trend continued after six years of follow-up. Another study by Abdulmalik et al favoured PCI over redo-CABG and conservative treatment.10 At one year angiographic and clinical follow-up, these authors found a 14% restenosis rate of the target vessel in the PCI group, while 47% of the no-PCI group (including surgical and conservative treatments) were readmitted with recurrent ischaemia. Only one small study examined the use of drug-eluting stents in immediate post-CABG complications, this was conducted by Price et al12. The authors reported that angiographic results were improved, but at a cost of 17% major bleeding complications.
A recent study by Zhao et al examined the collaboration between surgeons and interventionalists in assessing the immediate results of CABG.16 The study was performed in a hybrid operating room in which angiographic assessment of the results of CABG was performed before the patient leaves the operating room. In the reported initial 366 procedures, suboptimal results of CABG were identified in 12% of the cases and were corrected either by surgical revision or by hybrid PCI, with good short-term results and no significant difference in operative mortality between hybrid versus standard CABG (2.6 and 1.5% respectively). The one year follow-up results of this study are pending publication.
Institutional experience at Hospital Clinico San Carlos
Looking again at our own experience, we found that out of the 1,220 CABG performed during the study period, 65 patients (5%) underwent coronary angiography±PCI within 30 days after surgery. Detailed review of medical records showed that 11 (17%) of these procedures were actually scheduled as part of a hybrid procedure (CABG+PCI) and therefore were excluded from further analysis. The remaining 54 patients (4.4% of all CABG procedures) that underwent coronary angiography as an emergent diagnostic procedure constitute the study population we shall be discussing hereafter.
BASELINE CHARACTERISTICS AND INDICATIONS FOR ANGIOGRAPHY
The demographic baseline characteristics of the study population are shown in Table 1. The most frequent indication for urgent coronary angiography was perioperative myocardial infarction that was diagnosed by development of ST segment elevation or new Q waves in the ECG or a significant rise in the CPK (5 x ULN)3 (Table 2).
The majority of the patients had two grafts implanted (33, 61%). While the rest of the patients are distributed as following: one graft (10,19%), three grafts (9,17%) and four grafts (2,4%). Major intra-operative complications were recorded in three patients, included major bleeding required transfusion, disconnection of a newly implanted venous graft that was discovered during postoperative coronary angiography (Figure 1) and aortic dissection, while the rest of the patients had a non-eventful intra-operative course.
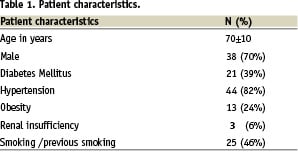
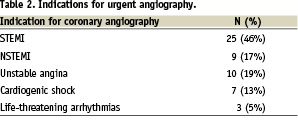
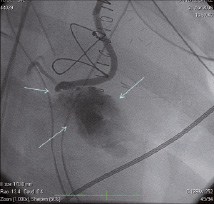
Figure 1. Disconnection of a vein graft in a patient presented immediately after CABG with cardiogenic shock. The arrows point to the site of disconnection at the distal anastomosis and to the extravasated contrast in the pericardial space.
ANGIOGRAPHIC FINDINGS
Most angiograms and PCI´s were performed on the same day of surgery (24, 44%) or the day after (9, 17%), while the rest (21, 39%) were performed between day three and 30.
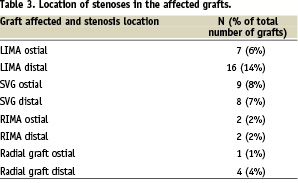
The most frequent finding in coronary angiography was acute total or partial occlusion of a newly implanted graft (39 patients, 72%), while in 14 (26%) patients all the grafts were found to be patent and with no evidence of progress in native arteries disease. In one patient (2%), there was an acute occlusion of a non-vascularised native coronary. Out of 111 grafts implanted, 49 (44%) were affected; the details are summarised in Table 3.
PROCEDURAL OUTCOME
Out of the 54 patients who underwent emergency coronary angiography, 33 (61%) patients (3% of all CABG procedures) underwent PCI to native arteries, grafts or both as a bailout procedure; 6 (11%) were referred for urgent redo-CABG and 15 (28%) were treated conservatively. Of those who underwent PCI, seven out of 33 (21%) were treated with balloon angioplasty in the graft, three (9%) with stenting of the graft, 19 (58%) with stenting of native coronary vessels, and four (12%) with stenting of both grafts and native coronaries.
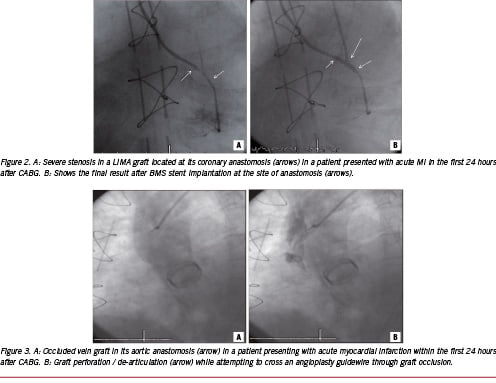
During the procedure, 19 (58%) patients had no complications and this was the group we defined as having procedural PCI success (Figure 2A and B), while in four (12%) patients PCI failed. Complications observed during PCI in 10 out of 33 (30%) patients included five out of 14 patients who underwent graft PCI (36%) and five out of 19 patients who underwent native coronary artery PCI (26%). Extravasation of contrast, suggestive of dissection / perforation of grafts or native arteries during PCI, occurred in five (15%) patients. Only one of them developed cardiac tamponade. Other complications included: cardiac arrest (1,3%), no reflow (1,3%), intra-procedural MI (1,3%), loss of major side-branch (1,3%) and localised aortic dissection while trying to advance a guidewire into an occluded vein graft (1,3%) (Figure 3A and B). Intra-aortic balloon pump was used in five (15%) patients out of the 33 patients during PCI.
IN-HOSPITAL OUTCOME AND FOLLOW-UP
Out of the 54 patients who needed urgent angiography, there were 14 (26%) deaths. Overall in-hospital mortality was 20% (11/54 patients). In-hospital mortality for patients undergoing PCI was 15% (5/33). During follow-up (median 27 months), two patients (6%) died.
As limitations to this review of our institutional experience, we must mention its retrospective character, the limited number of patients included as well as its focus on the characteristics and results of PCI which constitutes the topic of this article, without making a comparison with the results of redo-CABG.
Discussion
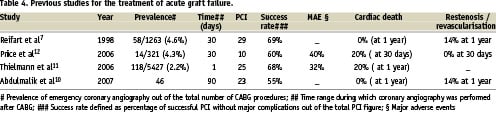
Our review confirms the lack of adequate knowledge on PCI as a rescue procedure after CABG. Most of the studies conducted were small case series (Table 4) and specific recommendations on the management of these high-risk patients have been collected in clinical practice guidelines. This lack of adequate knowledge contrasts with the substantial proportion of post-CABG patients treated with PCI which, according to our experience and to that of other authors, appears to be around 3-5% of all CABG procedures.
Several considerations should be made. First, early diagnosis and prompt decision-making appear to be of paramount importance and may influence short and long term prognosis11. Second, early diagnosis of perioperative ischaemic complications is challenging, as ECG changes and raised myocardial markers are common after CABG; hence the need of specific criteria and diagnostic algorithms for early detection and subsequent referral for emergent coronary angiography. Third, working with a freshly implanted graft seems to be associated with a higher risk of graft rupture or anastomotic dehiscence than in the chronically implanted setting. Finally, the patients are critically ill, with more frequent haemodynamic instability as a result of the immediately preceding cardiac surgery and may benefit from concomitant use of an intra-aortic balloon pump17.
The present systematic review of the literature as well as the clinical experience of an institution with a large workload volume, underline the key role that coronary angiography plays in ascertaining the cause of ischaemic complications in the perioperative period. In agreement with previous reports, we found that the occlusion of a freshly implanted graft is the most frequent cause of perioperative myocardial ischaemia. In spite of this finding, PCI to native arteries was the preferred procedural approach (70%), rather than treatment of grafts. In 26% of our patients, coronary angiography did not reveal graft failure or new native artery occlusion. This percentage is comparable to that reported in previous studies that (13-42%)10,11. Although no evidence on the underlying cause of myocardial ischaemia can be demonstrated, air embolism or micro-circulatory damage related to the intervention is potentially observed and can be proposed as possible mechanisms.
When compared with percutaneous interventions in other contexts, PCI as a bailout treatment for patients with acute perioperative cardiac events is associated with a significant mortality and morbidity. Bailout PCI after CABG had, in our experience, an associated mortality rate of 21% (15% in-hospital and 6% during the follow-up period) which is comparable to that reported in other series11. It is difficult to extrapolate any conclusions on the available evidence as to whether PCI is safer that redo-CABG in this emergency context. A complex native coronary anatomy might, in many cases, be the reason for which CABG was chosen as the method of revascularisation. The time required to organise an operating room in emergency circumstances may, on the other hand, contribute to the development of more extensive necrosis and haemodynamic instability; an accessible catheterisation laboratory can save the precious time needed to salvage the myocardium. Likewise, it is not possible to infer whether the use of drug-eluting stents in bailout PCI provides additional benefits. A high-risk of major bleeding was shown in the only study reporting on this subject12, although double antiplatelet therapy should also be initiated in case of using bare metal stents during the critical perioperative period, which is when rescue PCI takes place.
Developments in this field might come, on the one hand, from the availability of hybrid catheterisation laboratories, which might be useful not only to angiographically ensure an optimal result of CABG, but also to facilitate decisions as to the technique of reintervention (surgical or PCI)16. Potentially, multi-detector coronary angiography might also be of use as a screening tool for graft patency as reported in non-acute settings18, although, in the context of perioperative complications, this appears logistically far more complex.
Further information on the management of these patients will probably come from dedicated entries in PCI and CABG registries since a randomised design does not appear feasible. Close cooperation between cardiac surgeons, interventional cardiologists and intensive care unit personnel appears to be of paramount importance to provide urgent, multidisciplinary care to these patients19.

