Abstract
As has been seen in primary coronary artery bypass surgery (CABG), the patient population undergoing surgical secondary revascularisation (RECABG) has changed during the last twenty years. An increasing number of older patients, with more coexisting disease, are presented for RECABG. Beside the demographic changes, there are also changes as a part of the results of the different strategies used in CABG. The extensive use of arterial grafts in CABG results in an increase of the event-free period and of the period between CABG and RECABG. But results also show a challenge for RECABG with a patent arterial graft. Also, routine use of antiplatelet drugs and statins after CABG have an influence on the patient population presented for secondary revascularisation. Probably the most important aspect here is the evolution in percutaneous coronary intervention (PCI), especially in combination with a patent arterial graft protecting part of the myocardium. The purpose of this paper is to review the evolutionary trends in the patient population undergoing secondary revascularisation.
Introduction
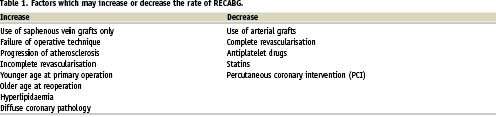
In 1983, Loop postulated that about 7% of patients undergoing primary coronary arterial bypass grafting (CABG) in time would need a second operation for recurrent angina1. During the last decade, much has changed in the fields of cardiac surgery, anaesthesia and intensive care which have resulted in lower mortality rates and a shift away from cardiac related mortality and morbidity after CABG to non-cardiac related mortality and morbidity. Loop’s postulation, however, has turned out to be true, because the percentage of re-operative coronary artery bypass grafting (RECABG) currently varies between 6-10% of the patient population.1-3 There seems to be a paradox here. On the one hand, the results of CABG have improved remarkably, with longer life expectation of the overall population even with the acceptance of older patients for cardiac surgery. On the other hand, more patients with suboptimal distal coronary arteries undergo CABG with a higher risk of recurrent angina. (Table 1) However, in the last years there is a decrease of RECABG.2,3
Early and late return of angina - early and late graft failure
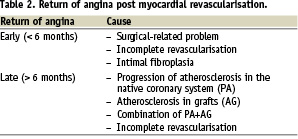
Coronary artery bypass surgery is a well recognised treatment for coronary artery disease. The use of arterial grafts have improved long-term results in terms of survival as well as in return of ischaemic symptoms.4 However, the process of atherosclerosis cannot be stopped, and the return of angina pectoris seems inevitable. This return seems to be biphasic: an early return of angina pectoris within six months after CABG, and a late return more than six months after CABG. Early graft failure, due to intimal fibroplasia5 and incomplete revascularisation are the main reasons for this early return. Late return is due to progression of atherosclerosis in the native coronary artery system, in the vein grafts, or both (Table 2).
It seems that the reason for RECABG is time related: in the early seventies, the majority of the patients underwent a RECABG because of progression of atherosclerosis in the native coronary system, or due to incomplete revascularisation at the CABG. Later in the eighties, the reason for RECABG had shifted to predominantly failure of the graft. Furthermore, in the seventies the mean interval between the CABG and RECABG for graft failure alone was approximately 25 months and 45 months for the combination of graft failure and progression of the atherosclerosis in the native coronary system. Later, with more experience, these intervals increased up to 66 months and 90 months respectively. These data indicate that even after a successful CABG, the patency of grafts is compromised, predominantly by vein graft atherosclerosis. Currently, the interval between the CABG and RECABG is still increasing because of the better patency of arterial grafts compared to vein grafts, as well as due to the acceptance of older patients for RECABG. However, the use of arterial grafts will not hold back the process of atherosclerosis; it only prolongs the interval free of angina pectoris. As a result, the biphasic pattern will flatten because the early return of angina pectoris will decline and the late return will occur later. The need for a RECABG, therefore, cannot be abolished simply because the process of atherosclerosis cannot be stopped in spite of the use of arterial grafts and other precautions to improve the patency of the grafts.2,3
It was through the popularisation of off-pump surgery there was a result in an increased early return of angina pectoris. With off-pump techniques, the anastomosis are made on the beating heart with the aid of special tools to stabilise the anastomotic region without hampering the heart function. It is a striking phenomenon, that in several cardiac-surgery centres with off-pump techniques, significantly less distal anastomosis are performed compared to classic on-pump surgery. However, there are no data or reports confirming this statement.
Patient selection
The two major indications for CABG are: improvement of the prognosis and relief of complaints due to reversible myocardial ischaemia not responding to medication.6 For RECABG, the indications for surgery are actually similar. Improvement of prognosis after RECABG is especially seen in patients with late vein graft stenosis to the left anterior descending coronary artery (LAD) more than five years after CABG with revascularisation of the LAD using the left internal mammary artery (LIMA)7. In the last two decades, nearly all patients have received a LIMA graft to the LAD, so this cohort gradually has become rare. The indications for RECABG are thus similar to the indications for CABG, albeit that the perioperative mortality of the RECABG is higher (2-18%) compared to CABG (1-4%).2,3,8
Resternotomy
The risk of a resternotomy is related to fibrosis and scarring of the pericardium and mediastinum. Haemorrhagic complications due to laceration of the right ventricle during resternotomy can be life threatening. In 1983, Loop concluded that control and management of the mediastinal adhesions, was the prime reason for the improved results in RECABG.1 With increasing experience, repeat median sternotomy is no longer considered as an incremental risk factor for mortality for RECABG.8 To avoid the potential problems of resternotomy, alternative approaches were introduced as an alternative to the resternotomy such as the posterolateral thoracotomy, a left anterior small thoracotomy for minimal invasive procedures, or even laparotomy.9-11 These approaches have an advantage in that they enter the chest by a non-operated route. However, the drawback is that they offer only limited exposure to the heart, which can compromise total myocardial revascularisation
Grafts, old and new
Certainly in RECABG, vessel identification can be difficult, and lack of bypass conduits may contribute to incomplete revascularisation. Specific for RECABG is the presence of old vein grafts. Progression of atherosclerosis involves not only the native coronary artery system, but also the vein graft. A study from the Cleveland Clinic reported that five to 12 years after CABG, 40% of the vein grafts were stenotic or totally occluded.12 Of clinical importance is that vein graft atherosclerosis is more dangerous than native vessel coronary artery disease. The mechanism by which late vein grafts occlude, produces clinical events such as embolisation of atherosclerotic debris and graft failure. Furthermore, it differs distinctly compared to native coronary artery atherosclerosis. Coronary artery atherosclerosis is focal, with eccentric plaques that have a fibrous cap overlying a centre of lipid debris, whereas vein graft atherosclerosis does not with the result that the debris is exposed directly to the blood stream.13 These lesions are friable and fragile and might result in embolisation by manipulations of the heart, arterial pressure fluctuations and antegrade delivery of cardioplegic solution during re-operations.
To decreases the risk of embolisation during manipulation, the patient should be put on bypass with the so called ‘no-touch’ technique, retrograde delivery of cardioplegia and cardiac dissection when the heart is still and flaccid. Ligation of diseased vein grafts is dangerous because this might result in squeezing debris into the distal coronary circulation. Some advocate graft division or favour replacement of the old vein grafts, but even these options are debatable. An argument against ligation or division of the old graft is the so-called ‘hypoperfusion syndrome’. This means that when a patient with a diseased vein graft to the LAD artery is disconnected and replaced by an IMA-graft, hypoperfusion of the coronary area might occur, manifested as ST-segment changes, arrhythmia or hypotension. This problem could be avoided by adding a new vein graft to the LAD, or with preservation of the old and diseased vein graft.12
With the increased use of the IMA-grafts during CABG, re-operations in patients with a patent IMA-graft is challenging in terms of preservation of the patent IMA and myocardial protection of the IMA-dependent myocardium. These problems can be adequately solved with the use of retrograde delivered cardioplegia. Thus, a patent IMA should not be considered as a risk factor for mortality or morbidity in reoperations.14
Most RECABG can be done using the classic conduits like the saphenous veins, the internal mammary arteries, the gastro-epiploic, radial and even the inferior epigastic artery.15 Other, alternative conduits, which are used infrequently are the lesser saphenous vein, cubital veins and homografts. The use of bovine heterograft arteries has now been abandoned due to unacceptable low patency rates. In some patients, however, there will be just enough length of conduits, so that maximal use is important. Also Y- or T graft constructions can be performed. In patients with a patent IMA-graft, a recycling of this IMA graft can be done successfully without compromising this graft. This recycling technique was first described by the Nijmegen group.16
Myocardial protection
The mortality of a RECABG exceeds the mortality of a CABG. Also, the difference between RECABG and CABG with regard to perioperative myocardial infarction is another striking finding.1-3 Furthermore, in CABG, there is a shift away from cardiac-related postoperative morbidity and mortality in contrast to RECABG.
The inefficiency of myocardial protection in RECABG is related to several problems. First, the complex anatomy, mostly expanded with a collateral circulation of the myocardial blood supply, the routes of myocardial perfusion with patent and diseased vein grafts as well as the blood flow through patent IMA-grafts, are the reasons that the antegrade delivered cardioplegia is suboptimal in protecting the heart. Secondly, embolisation of debris from atherosclerotic vein grafts during antegrade infusion of cardioplegia jeopardises the run-off of the distal coronary arteries, which might lead to a perioperative myocardial infarction. In order to prevent this, one could argue that it might be wise to disconnect the diseased vein graft before cardioplegic delivery is given. The drawback with this option is that it might provoke hypoperfusion of the myocardium. Therefore, retrograde, trans-atrial perfusion of cardioplegia through the coronary sinus seems to be the most effective alternative. The advantages are that there is no atherosclerosis in the venous system, the debris in the coronary arteries will be washed out, and the cardioplegia can be delivered independently of the position of the heart. With this preservation technique, the Cleveland group has shown a significant decrease in perioperative myocardial infarction and postoperative morbidity, thereby underscoring the effectiveness of the retrograde trans-atrial delivery of cardioplegia in RECABG.17,18
Perioperative mortality and morbidity
Perioperative mortality and morbidity, such as myocardial infarction after RECABG, are still troublesome and higher than in CABG. Mortality rates vary between 4-18% for RECABG versus 1-4% for CABG, and the incidence of perioperative myocardial infarction varies from 6-15% in RECABG versus 2-6% in CABG.1-3
There is no doubt that advances in perioperative anaesthetic management, myocardial protection and surgical techniques in the last decades have reduced the risks of RECABG. However, in spite of these changes, the prevalence of risk factors for hospital mortality and morbidity has further increased over the years. A clearer insight into the demographic profile of the cardiac patients for RECABG is crucial to unravel the problem of a persistent high mortality and morbidity in RECABG.3 Non-elective procedures, perioperative myocardial infarction and retrograde delivery of cardioplegia are all identified as independent variables for mortality and morbidity rates.2,3,8 Still, it is difficult to compare these studies and come to a definitive conclusion because the endpoints ‘mortality’ an ‘morbidity’ are not consistently defined. Some series use in-hospital mortality and morbidity and others 30-days mortality and morbidity. In our series, we advocate a 6-month mortality and morbidity, because it is known that the operative risk, certainly in high-risk patients, is prolonged.8
Long-term results
Ten-year survival after successful RECABG is about 80%.2,3,7,12,17,19 A number of these patients return with symptomatic coronary disease, as coronary artery sclerosis is a progressive disease in both the native coronary system and the conduits. It is generally accepted that with each subsequent reintervention the probability of an “angina-free period”, as well as the interval between these periods, diminishes. The long-term results after revascularisation of the coronary vessels are not only influenced by graft choice and completeness of the revascularisation, but also by older age, impairment of the left ventricle, hypertension, diabetes mellitus and congestive heart failure.8 For RECABG, it seems that the long-term results are predominantly determined by the perioperative risk; and that survival of the postoperative period is the first step in long-term survival.
Off-pump surgery and percutaneous coronary intervention
Due to the relative high morbidity and mortality for RECABG, there is a some reservation for “classic”, on-pump, RECABG. However, because most patients have one or two patent arterial grafts, the jeopardised myocardium can be approached by percutaneous techniques, with less mortality and morbidity. But also alternative routes as anterolateral or posterolateral thoracotomy, and off-pump techniques can be used for revascularisation. These off-pump techniques avoid a lot problems of on-pump RECABG, as described in this report, and in all studies there is a trend towards a reduction in mortality and morbidity in de redo-off-pump groups.20
Conclusion
RECABG is a challenge for the cardiac surgeon. The increasing incidence of the procedure itself, along with the persistently elevated rates of morbidity and mortality, all add to the challenge. RECABG is technically more complicated than CABG. Most of these complications are related to each other and are the consequence of our strategies at primary CABG. Off-pump surgery can avoid several pitfalls of on-pump redo surgery. Percutaneous coronary interventions are, however, preferable for these patients.

