Abstract
Patients undergoing coronary re-operations have a higher risk profile. Also reoperations are technically more demanding and can be very challenging to perform. This patient group commonly has severe and diffuse distal coronary artery disease and aortic and non-cardiac atherosclerosis. Some technical hazards, including the presence of patent arterial grafts and/or diseased vein grafts are common. A careful preoperative assessment and planning of the surgical technique are mandatory.
Introduction
Hospital morbidity and mortality after re-operative coronary artery bypass surgery is higher than after primary surgery. This is due to the increased technical difficulty and the higher risk-profile. The complexity and risk are increased by the sternal re-entry, pericardial adhesions, patent internal thoracic artery (ITA) and patent, but diseased, saphenous vein grafts, among others. Besides, patients undergoing re-operations are older and more likely to have vascular disease, left ventricular dysfunction and extensive coronary artery disease. Despite these factors, mortality and morbidity associated with coronary reoperation has decreased because of the greater surgical experience and the better management of patient comorbidities1-6.
The profile of patients undergoing redo-coronary artery surgery
The higher mortality of these patients is mainly attributable to the higher risk profile. Patients undergoing redo coronary surgery are older, have more comorbidity and more severe and diffuse coronary disease7. A great amount of factors may have a deleterious effect on patient outcome and they should be considered and treated if possible before the operation, such as: chronic kidney disease or potential causes for deterioration of renal function; pulmonary disease; history of preoperative cerebral vascular disease or the presence of carotid bruits; electrolyte disturbances; any medical condition or drug that would predispose the patient to bleeding; and overall malnutrition.
Age
We know that the higher the age, the higher the mortality. Although we agree with G.E. Thibault8 when he says “there is nothing like cardiac surgery to bring out a patient´s true age”, we must also say that age, per se, should not be considered a contraindication for surgery. The decision should be made taking into account the cardiovascular disease, the comorbidity and some individual considerations such as patient’s wishes, family support, cognitive function, nutritional status, and others9. The department of geriatric medicine should have a key role in the preoperative assessment of the elderly population.
Kidney function
Most preoperative cardiac risk stratification systems include creatinine as a predictive factor of mortality. However serum creatinine is not a precise measure of kidney function. The estimated glomerular filtration rate (using the MDRD-4 equation or others) defines more accurately the stage of the disease and a low rate is associated with a higher mortality. In our series10, patients with an estimated rate < 60 ml/min/1.73 m2 were 2.4 times more likely to die than those whose rate was > 60, both groups being adjusted for age and sex (p<0.001, OR 2.4, 95% CI 1.6-3.4). A careful evaluation and treatment of these patients by the nephrologist is mandatory in an attempt to improve the kidney function and decrease the risk.
Lung function
Chronic obstructive pulmonary disease (COPD) is an important preoperative risk factor for mortality and morbidity11. Respiratory dysfunction after cardiac surgery is multifactorial (general anaesthesia, sedation, sternotomy, pleural opening and cardiopulmonary bypass, among others) and the presence of previous lung disease (mainly chronic obstructive pulmonary disease, COPD) and/or current smoking are the best predictors. Spirometric pulmonary function tests help us in the decision to operate or not to operate and, especially, allow us to identify the patients who will benefit from an intensive pre- and post-operative respiratory physiotherapy.
Carotid artery occlusive disease
Carotid disease is frequently seen in patients who require coronary artery surgery, as the two diseases entail a similar pathologic process. It may result in a stroke if it is untreated due to the haemodynamic fluctuations during the cardiac surgery12. The odds ratio for stroke in presence of significant carotid disease is 5 to 10. Based on AHA/ACC guidelines13, the criteria for preoperative carotid screening are carotid bruits, left main disease, peripheral vascular disease, history of cerebrovascular accident, history of heavy tobacco use, and age >65 years (Figure 1). There is no general agreement, but the AHA/ACC guidelines13 recommend that a carotid stenosis of 80% or more, even if asymptomatic, should be treated before the coronary artery surgery (Class IIa recommendation, level of evidence C). This staged approach is favoured by many surgeons, although a simultaneous procedure may be preferable in patients with acute ischaemic changes and/or very severe cardiac lesions.
Figure 1. Severe stenosis of the right internal carotid artery.
Coronary artery disease
Progression of vein graft disease is the most common cause of reoperation, but progression of native coronary artery disease frequently coexists. A carefully analysis of the preoperative angiography is necessary to assess the distal bed of coronary arteries. Patients requiring reoperation should have at least one target artery with a diameter of 1.5 mm or greater supplying viable myocardium. Sometimes a patent vessel beyond an occlusion is not seen in angiography and contrast-enhanced multidetector computed tomography (CT) is very useful in locating it14,15 (Figure 2). A viability test should be necessary in presence of left ventricular dysfunction and history of myocardial infarction. Magnetic resonance imaging is the technique of choice because it allows us to analyse not only the viability and ischaemia, but also left ventricular size and function and anatomic relations16 (Figure 3).
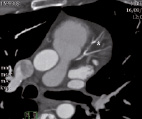
Figure 2. Multidetector CT: distal left anterior descending artery (asterisk). The angiography was unable to show it.

Figure 3. MRI: Delayed enhancement (white area) showing transmural anterior necrosis without myocardial viability, and a mural thrombus (arrow head).
The incidence of chronic ischaemic mitral insufficiency is higher in patients requiring reoperation because of the more extensive coronary disease, the higher incidence of myocardial infraction and the poorer left ventricular function. It is associated with higher operative mortality and lower survival rates. Since mitral valve repair preserves better the ventricular function than valve replacement, it is the treatment of choice17. Data suggests that mitral repair might improve late outcomes if it can be performed with little additional operative risk and low incidence or residual mitral regurgitation. Analysis of the mitral valve with transthoracic echocardiography should be done in all patients in order to know the mitral function. If mitral insufficiency is present a transesophageal echocardiogram is essential in determining the mechanism and the severity of the mitral regurgitation.
Primary surgery
The surgical and the clinical report give us information about the operative findings, the surgical technique, surgical and anaesthetic incidences and postoperative events such as sternal wound infections and reoperations for bleeding, which can help us in planning the operation. The risk of damage of a patent left ITA at reoperation is related to the care taken at the primary operation to protect the graft18 (Figures 4 and 5). The reading of the surgical report might allow us to know if the left ITA has been routed into the pericardium though a slit keeping it from becoming adherent to the posterior sternal table.
Figure 4. Angiography: patent LITA close to the posterior sternal table (asterisk).

Figure 5. Multidetector CT: patent LITA close to the posterior sternal table (asterisk).
Technical challenges
Sternal re-entry
The pericardium is usually not closed after heart surgery and these vital structures may adhere to the underside of the sternum, with an increased risk of injury during re-sternotomy (Figures 6-8). Catastrophic haemorrhagic events, as well as left ITA graft injury, have been reported to occur in 2-6% and 5-38% respectively. In the largest reported series the injury to the left ITA graft was followed by a perioperative infarction in 40% of patients18. Although using an oscillating saw decreases the risk, it does not eliminate it. Standard preoperative evaluation using chest radiographs and coronary angiograms provides only imprecise anatomic information. Gasparovic et al15 found that in 85% of patients they were unable to obtain all pertinent topographic information about vital mediastinal structures from these methods of evaluation. Contrast-enhanced multidetector CT provides us with a detailed three-dimensional imaging of mediastinal anatomy and an accurate identification of the position of patent grafts, with the exact relation between the sternum and these structures. It should be implemented into the routine preoperative evaluation of cardiac surgical patients with previous coronary artery surgery. If preoperative imaging suggests the risk of damage, extra measures before opening the sternum can be adopted, such as peripheral cannulation. In patients requiring limited revascularisation, risk of sternal re-entry can be avoided by using alternative incisions, such as anterior mini-thoracotomy, lateral thoracotomy or epigastric approach.
Figure 6. Multidetector CT: patent vein graft close to the posterior sternal table (asterisk).
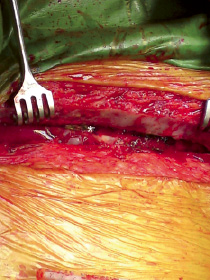
Figure 7. A patent vein graft is stuck to the sternum (asterisk).
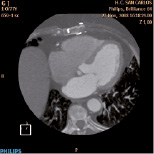
Figure 8. Multidetector CT: risk of injury to the right ventricle free wall during re-entry.
Atherosclerotic/calcified ascending aorta
Patients undergoing reoperation are more likely have an atherosclerotic or calcified aorta. Neurologic dysfunction is one of the most common major complications after cardiac surgery, and although carotid disease account for some of these complications, most events are related to emboli from the ascending aorta19. A diseased aorta also presents technical problems, such as finding the most suitable site of cannulation, aortic clamping and construction of adequate proximal anastomoses. The analysis of the ascending aorta can be done with the angiography, the transesophageal echocardiography and CT. Alternative cannulation sites with or without ascending aortic replacement, off-pump surgery and/or construction of T-grafts may be necessary in order to avoid the high risk of stroke. If on-pump surgery is unavoidable, the best choice for arterial cannulation is the axillary artery, because these patients usually have aortic arch, descending thoracic aorta, aorto-iliac and femoral atherosclerosis as well.
Patent atherosclerotic vein grafts
Embolisation of atherosclerotic debris may occur if these grafts are manipulated during dissection of pericardial adhesions20. If the angiographic assessment shows patent but extensively diseased venous grafts the manipulation must be avoided before the aorta is clamped. Retrograde cardioplegia is used to remove vein graft atherosclerotic debris that inadvertently has embolised to a coronary artery. If we are operating off-pump, diseased venous grafts must be left in place, with no manipulation.
Conclusions
The indications for reoperation are generally the same as those for primary surgery. The benefits are also similar and the difference in hospital mortality between primary and reoperative coronary surgery has narrowed considerably. A careful preoperative assessment and planning of the surgical technique make the risk of reoperative surgery approach that of primary surgery.

