Abstract
Many patients will experience a return of symptoms after their initial revascularisation procedure necessitating secondary revascularisation (SR). The options for this second procedure are inherently influenced by the primary method adopted for revascularisation. Patients with single vessel disease are most suited to percutaneous coronary intervention (PCI) for both primary and secondary revascularisation. The arrival of drug eluting stents, and evidence from trials of highly select populations has threatened the place of coronary artery bypass grafting (CABG) as the preferred method of revascularisation in those with multivessel disease. At present, and without robust evidence, PCI is increasingly being used to treat highly complex lesions, such that many question whether CABG is still has a role in primary revascularisation. The consequence for SR is that currently it is increasingly likely to be in response to in-stent restenosis, whereby previously it was performed in those with prior CABG. The recent SYNTAX trial has reaffirmed the position of CABG in the treatment of those with complex coronary disease. Consequently we believe that matters have turned a full circle, and expect that SR in the future is most likely to be in form of PCI on patients 8-15 years post primary CABG.
Introduction
Coronary artery disease (CAD) is the leading cause of mortality worldwide. Coronary revascularisation, either through percutaneous coronary intervention (PCI) or coronary artery bypass graft surgery (CABG) is advocated when symptoms remain uncontrolled despite optimal medical therapy.1 The duration of benefit from revascularisation is variable and some patients will return with a recurrence of symptoms requiring secondary revascularisation (SR). This is because of either restenosis or occlusion of the stent or bypass graft, progression of underlying native CAD, or incomplete initial revascularisation. The ‘problem’ is compounded by the overall increased life expectancy, such that patients are now ‘out living’ their primary revascularisation (PR). The consequence is that SR is likely to be an increasing part of the daily workload of today’s and future cardiologists and cardiac surgeons.
The preferred method of initial revascularisation has varied over the years, and ultimately this inherently influences the method of SR available to the patient. The increasing use of PCI to treat ever more complex CAD has led many to question whether cardiac surgeons still have a role in PR.
In this article we initially describe the trends of PR in patients with single vessel disease (SVD) and multivessel disease (MVD), and describe how these trends may influence the method of SR. Finally, we will discuss the SYNTAX trial, and give our opinion as to how we feel SR will change following its publication.
Trends in the management of single vessel disease
Revascularisation for SVD carries a significantly lower mortality compared to those having MVD. Early trials of revascularisation showed a distinct advantage for CABG compared with medical therapy in patients with specific SVD – namely a significant proximal left anterior descending artery (LAD) lesion.2 Furthermore, evidence from both the New York and Duke registries showed that CABG also conferred a significant survival advantage over PCI in these specific patients.3,4 It is no surprise then that in the New York surgical registry of over 29,000 patients, of whom 8.7% had a single vessel CABG, the indication was proximal LAD disease in 74.3% (n=1,917).4
These early registries have limited clinical applicability in the current era. Two main factors which may have influenced outcome were stent usage, which was only 11.8% in the New York registry, and usage of left internal mammary artery (LIMA) grafts. The Duke registry ran from 1984 to 1990 and the New York registry from 1993-1995, and although there is no comment on LIMA usage, in the 1980s studies have reported rates of LIMA use of approximately 15%,2 whilst in the late 1990s rates of over 90% have been reported.5 The relevance of low or even moderate use of the LIMA graft is the fact that they have significantly higher patency at follow-up, and confer a long-term survival benefit when compared with saphenous vein grafts.6,7
In recent times, evidence has emerged from two meta-analyses examining outcomes in patients with proximal LAD disease randomised to either PCI or CABG. Kapoor et al, concentrating on any surgical technique,8 whilst Aziz et al examined specifically those having the minimally invasive direct coronary artery bypass (MIDCAB).9 Notably, the use of stents and LIMA grafts was much higher than documented in the previously mentioned registries. Results from both studies showed that no significant difference in survival amongst patients assigned to either CABG or PCI, this extending out to five years in Kapoor’s study. Repeat revascularisation however, was significantly less after CABG than after PCI; with results maintained to five years in Kapoor’s study (7.3% v 33.5%, p<0.0001). The excellent long term prognosis of both treatments is further enhanced following the publication of Goy et al’s randomised study comparing bare metal stenting with LIMA grafting for proximal LAD lesions, which showed no mortality difference at 10 years follow up (PCI 8% vs. CABG 4% p=0.4).10
In summary, for SVD other than the proximal LAD, most clinicians historically and currently would have no hesitation in contemplating PCI. With regards to proximal LAD disease, historically these patients were predominantly referred for CABG, however evidence now suggests that PCI offers a similar survival benefit (up to 10 years), and therefore is a viable alternative.
How will this influence SR of these patients? It is apparent from the previous discussion, as well as the fact that only 4% of CABG is currently performed for SVD, that the majority of patients with SVD have PCI as the initial method of revascularisation. For patients with in-stent restenosis (ISR) of a proximal LAD stent, repeat PCI is effective. Moreno et al has shown cumulative survival rates in patients of 98.3±1.2% at one year, and 95.2±2.5%, at three years amongst 123 patients treated for ISR of a proximal LAD stent.11 In those patients initially treated with CABG, a LIMA graft is increasingly likely to have been utilised as the bypass graft for isolated proximal LAD disease. These grafts are unlikely to restenose, but the commonest site for restenosis is the insertion point on the LAD12 – which is effectively treated with PCI. In essence PCI is the preferred method of PR for patients with SVD and appears to be well suited for SR in these patients.
Trends in the management of multivessel disease
After its introduction in 1960s, CABG become the accepted treatment for MVD,13 however advances made in the percutaneous treatment of stable CAD from balloon angioplasty (POBA) to stenting with initially bare metal stents (BMS)14 and now drug eluting stents (DES),15-17 have made PCI a progressively more attractive alternative.
In 1995, before the widespread use of coronary stents, a three year meta-analysis was published comparing POBA to CABG for the management of MVD and found no difference in the rates of death and non-fatal MI (CABG vs. POBA HR 1.03, 95% CI 0.81–1.32, p=0.81).18 The use of coronary stents became increasingly prevalent following the superior results achieved with stenting when compared with POBA.14 A subsequent meta-analysis of five randomised trials comparing stenting with BMS to CABG in MVD, showed a similar rate of major adverse cardiovascular and cerebrovascular events (MACCE); and a higher rate of repeat revascularisation in the PCI group at both at one and five year follow-up.19-21
The development of DES led to significant improvements in the rates of restenosis and repeat revascularisation when compared to BMS in the setting of randomised trials. Their effectiveness in the ‘real world’ was also confirmed through multiple registries.22 The first randomised trial to compare DES to CABG in MVD was the ARTS-II study, which prospectively collected data on 607 patients, treated with DES, and then compared this data to the historical CABG control from the ARTS-I study.23 One year follow-up showed that PCI with DES was non-inferior to CABG with respect to MACCE rates, however the rates of repeat revascularisation, although lower than in the BMS arm of ARTS-I, were still significantly higher than in the historical CABG controls.
In summary, in patients with MVD all randomised clinical trials to-date, whether performed in the early days with POBA, or more recently with BMS or DES, show no mortality difference between PCI and CABG.18,21,24 Of note, PCI has always been associated with higher rates of re-intervention, however the advantage CABG holds over PCI in this respect has progressively narrowed with advances in stent technology (Figure 1).
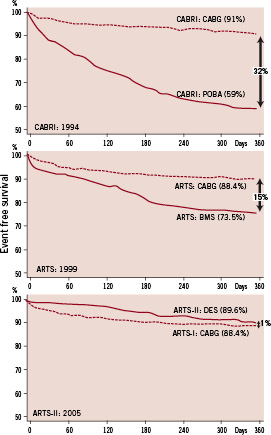
Figure 1. Event-free survival at one year follow-up in the CABRI, ARTS-I and ARTS-II studies showing a reduction in the difference in outcomes between CABG compared with balloon angioplasty, bare metal stenting and drug eluting stents.
Is this the end of CABG for primary revascularisation?
The improved outcomes in PCI with the use of DES has led to increasing confidence in tackling ever more complex disease, some of which was previous only the realm of the cardiac surgeon.25 Diabetic patients and patients with ever more complex lesions such as bifurcation lesions, chronic total occlusions, and left main stem disease are all increasingly undergoing PCI as the primary method of revascularisation, despite the absence of supportive, robust clinical evidence.
Many question whether CABG still has a role in PR. This is reflected in the current trends of revascularisation that reveal ever-increasing rates of PCI, whilst CABG rates appear to have reached a plateau (Figure 2). The available technology is such that most CAD can be dealt with by PCI, however is this the correct approach for the patient? It is important to remember that the evidence base for the use of PCI in these settings is currently limited. SR is heavily influenced by the primary method of revascularisation and from the above evidence, it may seem apparent that PCI can be used to treat the majority of lesions in PR, such that CABG can be ‘saved’ or deferred for SR; if it is actually required at all.
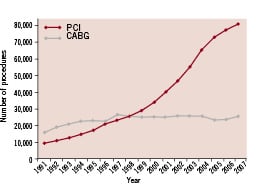
Figure 2. Graph showing the rising rate of PCI, and static rate for isolated CABG in the United Kingdom over the past 16 years.30 Image courtesy of Peter F Ludman on behalf of British Cardiovascular Intervention Society.
Before confining CABG to the history books for the management of CAD, it is important to consider some of the limitations of the available data, and question whether the randomised data truly reflected daily practice. In the trials comparing POBA to CABG, only 5% of patients screened for entry were randomised18 – common exclusions were patients with left main stem (LMS) disease, or those with ‘severe’ triple vessel disease (3VD).26 In trials comparing BMS to CABG only approximately 4% of patients initially screened were eventually randomised,21 with a common exclusion being those with impaired left ventricular function.13 It would seem apparent that the conclusions of these trials are based on a highly selected population, and not one that reflects daily clinical practice. Clearly additional evidence is required to confirm these initial promising results for PCI in the ‘real-world’ population.
The SYNTAX Trial – a saviour for CABG?
The SYNTAX trial27 (SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery) attempted to answer several important questions pertinent to the management of patients with MVD in the current era. Following on from the view of some die-hard interventional cardiologists, who felt no lesions were unsuitable for PCI, the SYNTAX trial sought to identify if any specific patient groups were solely eligible for CABG. In addition it sought to compare CABG and PCI in those high risk patients with MVD who had CAD suitable for either type of revascularisation. No evidence from randomised clinical trials existed for this patient group as they had largely been excluded from the previously conducted randomised trials. To aid the comparison between the CAD in each patient, the trial introduced the newly developed SYNTAX score to assess coronary lesion complexity.28 The ultimate goal of the SYNTAX score was to help provide guidance on optimal revascularisation strategies for patients with high-risk lesions. Importantly, to ensure the population studied reflected real world practice, the trial was designed as an all comer’s trial. The limited exclusion criteria were those patients who had had prior revascularisation, a recent MI, or required concomitant cardiac surgery. On the contrary only patients with 3VD or LMS disease (isolated or with any CAD) were included.
It is of paramount importance to understand the trial’s design when considering its impact on the role of PCI and CABG in PR and SR. The trial is comprised of three equally important and informative arms:
(1) Randomised Group – 1,800 patients (903 PCI, 897 CABG).
The Heart team, comprising of an interventional cardiologist and cardiac surgeon, determined which patients had CAD suitable for treatment by either PCI or CABG. Patients in this group were then randomised to either CABG, or PCI with Taxus® paclitaxel DESs (Boston Scientific, Natick, USA).
(2) PCI Registry – 198 patients.
This group of patients were those who were thought to be unsuitable for CABG. These patients represented those with the greatest comorbidities, and the subsequent highest operative risk, as depicted by their notably higher EuroSCOREs (Euro SCOREs PCI registry vs. Randomised Group, 5.8 vs. 3.8 respectively). Of note, these patients were not necessarily those with the most complex CAD. Their average SYNTAX score was 31.6, which is not markedly different from the PCI and CABG patients in the randomised group whose mean SYNTAX scores were 28.4 and 29.1 respectively.
(3) CABG Registry – 1,077 patients.
This group of patients were those who had CAD thought to be unsuitable for PCI. It comes as no surprise that these patients had the most complex CAD as shown by their high mean SYNTAX score of 37.8.
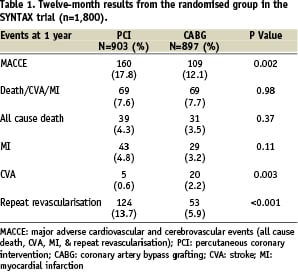
The trial enrolled 3,075 patients, who were entered into the appropriate arm of the trial after the Heart Team had reviewed their coronary angiogram. Overall, the majority of patients (n=1974, 64.2%) underwent surgical revascularisation; however it is important to note that over half these patients (n=1077, 54.6%) did so because the interventional cardiologist did not feel the CAD was suitable for PCI. On the other hand, only a minority of the patients undergoing PCI (n=198, 18.0%) did so because the cardiac surgeon felt their CAD and comorbidities precluded CABG. The remaining 1,800 patients all had CAD that was suitable for both types of intervention, and were therefore randomised. This data is somewhat at odds with the perception that CABG is confined to the, “back seat of the revascularisation vehicle.”29 To add further confusion to matters the results of all 1,800 patients in the randomised group of the study, which are summarised in Table 1, show no significant difference in rates of death, MI or death/MI/stroke. These results are reminiscent of the published trials of CABG against POBA, and BMS.18,21,24
So why is there such a discrepancy between what is perceived as the most suitable method of revascularisation (i.e. PCI), and the actual method employed in clinical practice (i.e. CABG)? Furthermore, would the outcomes of all those patients in the randomised group actually be the same or better with PCI compared to CABG, as the earlier trials suggest?
To help answer these questions, and further redefine the map as to which patients are more suitable for CABG compared to PCI, it is important to consider the results of the patients in the randomised group according to the their SYNTAX score. The drawback of considering the randomised group “en mass” is that this approach does not take into consideration the complexity of the patient’s CAD – there is a wide spectrum of 3VD and common sense and experience tells us that outcomes are not the same for all 3VD.
Patients in the randomised group can be split according to their SYNTAX score into tertiles, with the groups being defined as those with a SYNTAX score less than 23, between 23 and 32, and greater than 32. Figure 3 shows the one-year outcomes of patients in each of these three groups. Those patients with the least complex coronary anatomy have comparable results with PCI or CABG, and therefore the final treatment decision will be dependent on patient and physician choice, and individual patient preference. The group with the most complex disease (SYNTAX score >32) had a significantly better outcome with CABG, indicating that in these patients PCI should not be considered as the method of primary revascularisation.
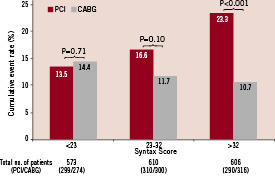
Figure 3. The twelve-month outcome of patients from the randomised arm of the SYNTAX trial grouped according to their SYNTAX score.
Overall, there was no significant difference in the outcomes for those patients in the middle group, (SYNTAX score 23-32) however the outcome was slightly better in those having CABG compared to PCI (11.7% vs. 16.6% respectively, p=0.1). A clearer picture of the optimal method of revascularisation of these patients is achieved by considering the outcomes according to the distribution of CAD (any LMS or 3VD), and the patient’s diabetic status (Table 2). Therefore considering the data presented in Table 2, CABG is the preferred method of revascularisation in those patients with a SYNTAX score of 23-32 who are either diabetic (LMS and/or 3VD), or those with 3VD. Those patients who are not diabetic with LMS disease have comparable outcomes with PCI or CABG, and therefore individual choice and patient characteristics need to be taken into consideration.
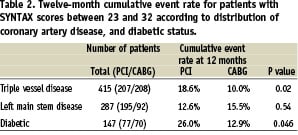
Figure 4 provides a summary of the important information the SYNTAX trial has provided on the optimal method of PR in patients with CAD. Over a third of patients with complex CAD, have lesions that are not suitable for PCI, and are best treated with CABG. In addition, comorbidities ensure that just over 5% of patients are not suitable for surgical revascularisation. Coronary anatomy is important in determining the most appropriate method of revascularisation in those with disease suitable for PCI or CABG. Those with the most complex anatomy, and a corresponding SYNTAX score greater than 32 are best treated with CABG. Overall, for 66% of patients with LMS and or 3VD, CABG offers the best initial method of revascularisation; for the remaining patients PCI offers an excellent alternative. These results provide a suitable evidence base to dispel those ‘rumours’ that CABG does not have a future in primary coronary revascularisation.
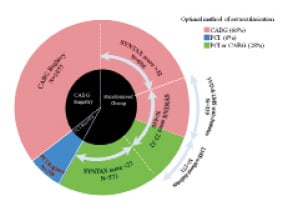
Figure 4. A pie chart summarising the optimal method of revascularisation of all patients in the SYNTAX trial taking into account both the initial decision of the Heart team and the SYNTAX score. The central pie chart (black) shows the distribution of patients on entry into the study, whilst the outer pie chart shows those patients in the randomised group split according to their SYNTAX score. Finally, the colours represent the preferred method of primary revascularisation for each subgroup considering all relevant factors.
So how does this effect secondary revascularisation?
Previously secondary revascularisation in patients with MVD involved managing those who had had prior CABG. The available options comprised of either PCI of a native vessel or bypass graft, or reluctantly offering redo CABG. Currently, following the unprecedented numbers of patients who have had multivessel PCI, it is likely that secondary revascularisation is increasingly being performed because of in-stent restenosis. The treatment options therefore comprise of repeat PCI, or CABG, with repeat-PCI the favoured option. In the SYNTAX trial at one year, the rate of repeat revascularisation for those treated initially with PCI was 13.7%; over four-fifths of these patients underwent repeat PCI. The SYNTAX trial has dispelled those thoughts that PCI would be the primary method of revascularisation in all patients with MVD, and dispelled those ideas that CABG would be left only for those patients with restenosis that was not amenable to repeat PCI. In addition it has confirmed the significantly lower rate of repeat revascularisation at twelve months in those receiving PR with CABG (5.9% vs. 13.7%, p<0.0001), and shown that PCI is the preferred method of SR in these patients (SR with PCI 79.7% vs. CABG 22.0%). Considering all this evidence, we believe that in the future, interventional cardiologists are again likely to be faced with performing PCI on patients 8-15 years after their primary surgical revascularisation.
Conclusions
In conclusion, debate has long raged over the best method of coronary revascularisation. Evidence and current practice suggests that SVD is most likely to be treated by PCI both for primary and secondary revascularisation. In those with LMS and/or 3VD the SYNTAX trial has shown that CABG is appropriate for two-thirds of the patients, therefore it continues to be an important method of primary revascularisation. Trends in secondary revascularisation follow from this, and matters appear to have turned a full circle – the difference however is that now a strong evidence base exists, something that was previously absent.

